Transcatheter aortic valve implantation (TAVI) is now indicated across all risk categories of patients with symptomatic severe aortic stenosis and has been proposed as a first-line option for the majority of patients ≥75 years old. The former discussion of whether a patient should undergo surgical aortic valve replacement (SAVR) or TAVI is shifting from patient age and surgical risk to life expectancy and the associated lifetime management of aortic stenosis for an individual patient1.
As indications for TAVI expand to include younger and healthier patients who are expected to outlive their initial transcatheter heart valve (THV), understanding the long-term implications of the initial intervention is paramount, since “the first cut is the deepest”. TAVI with a next-generation device has become a mature intervention that should grant the patient high procedural safety with low mortality and a low stroke rate, a low rate of conduction disturbances, and excellent haemodynamic performance without paravalvular leakage or leaflet thrombosis2.
However, for younger patients who have the realistic expectation of the need for reintervention, the implications of the initial intervention play a more pivotal role regarding durability, accessibility of coronary arteries, and future options to overcome bioprosthetic failure that include THV explant with SAVR or TAV-in-TAV with a second THV. Additionally, there are patients who have a realistic chance of requiring a third valvular intervention. The initial treatment strategy may limit reintervention options in the future12.
An intra-annular balloon-expandable valve has a shorter prosthesis stent frame with lower leaflets and skirt height, facilitating coronary access and reintervention with less risk of coronary obstruction. When performing valve-in-valve TAVI, the leaflets of the initial bioprosthesis are pinned into an open position by the second THV and a so-called “neoskirt” is created, which, for patients with low coronary height or a small aortic root can result in sinus sequestration or direct obstruction at the coronary ostium. Recent recommendations of higher THV implantation relative to the aortic valve annulus, to reduce the risk of conduction disturbances, may specifically limit the anatomical feasibility of TAV-in-TAV, especially when using self-expanding valves with a supra-annular valve position.
Most self-expanding valves have a longer prosthesis stent frame that anchors in the native aortic annulus and the ascending aorta, thereby hampering coronary access through prosthesis stent struts and commissural posts that are not aligned with the coronary ostia. However, the self-expanding design allows repositionability and might be associated with more favourable haemodynamics.
Taking all these considerations together, the new ACURATE neo2 Aortic Valve System (Boston Scientific Corporation) could be a jack of all trades: this THV consists of a self-expanding nitinol stent frame with three porcine pericardial tissue leaflets in a supra-annular position, without stent struts in the supra-annular position hampering access to the coronary ostia. The valve features a self-aligning design and a novel radiopaque marker to facilitate accurate positioning in the native aortic valve. The double pericardial skirt is intended to prevent paravalvular leakage. The device is currently available in three sizes for a native aortic annulus diameter range between 21 mm and 27 mm3.
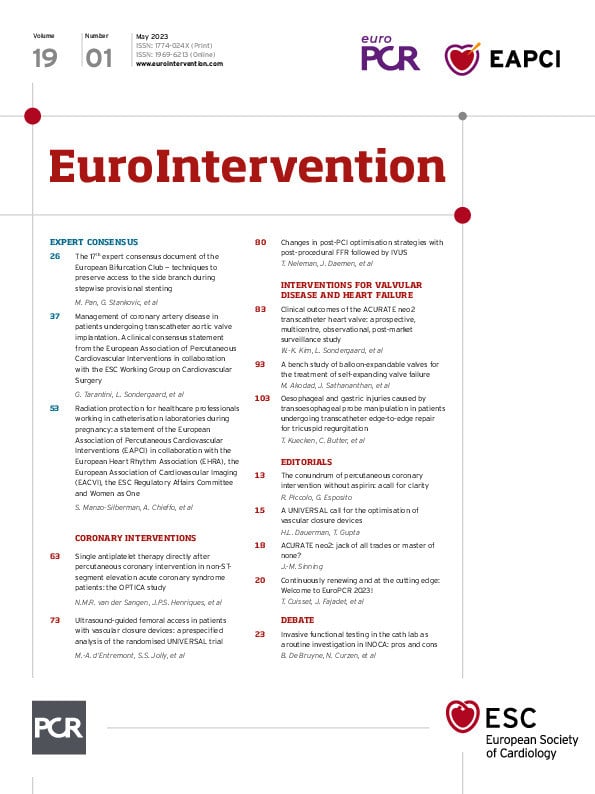
In this issue of EuroIntervention, Kim and colleagues can be congratulated on an interesting study that enrolled 250 predominantly intermediate- to high-risk patients at 18 centres in 8 European countries. In this observational post-market surveillance study, the ACURATE neo2 THV showed excellent results with a very low rate for 30-day mortality (0.8%), stroke (0.8%), and pacemaker implantation (6.5%)3.
The haemodynamic performance of this THV was superior to its predecessor with none to only mild paravalvular leakage (PVL) in 98.1% of the patients. Hypoattenuated leaflet thickening (HALT) as the primary imaging endpoint could be detected in 50 of 204 patients with the computed tomography (CT) imaging data available but did not lead to a significantly increased transvalvular gradient during short-term follow-up compared to patients without HALT3.
However, in 4 of 250 patients, the ACURATE neo2 THV could not be implanted in the appropriate position due to high positioning in the aorta and subsequent THV embolisation with the need for an immediate TAV-in-TAV procedure with a non-study balloon-expandable valve. One of these patients died due to coronary occlusion and cardiac tamponade. As the authors state in their discussion, these results are in line with the overall embolisation rate of approximately 1% in the TRAVEL registry. It seems that the ACURATE neo2 THV has overcome the weakness of its predecessor, the ACURATE neo, with a significantly lower PVL rate3.
Altogether, the ACURATE neo2 THV is a promising candidate to be an alternate THV option, in addition to the SAPIEN (Edwards Lifesciences) and the Evolut (Medtronic) prostheses. The ACURATE neo2 guaranteed an "event-free" TAVI procedure without the “Big 5” TAVI complications: rates for disabling stroke (0.0%), life-threatening bleeding (2.9%), more than mild PVL (1.9%), acute kidney injury (0.0%), and complete heart block (6.5%) were very low in this registry and should be reconfirmed in a randomised controlled study. Of course, long-term data are also needed to better understand its capabilities34.
Finally, a word of caution has to be said, as the results from this registry cannot be directly compared to clinical outcomes with other THV devices from randomised clinical trials as the authors properly state in the limitations section. Enrolment decisions were made per the discretion of the local Heart Team, so the possibility of site-based differences in patient selection cannot be ruled out. Notably, the fact that patients with severely calcified aortic valves might have been treated with other THVs cannot be ruled out as selection bias3.
Although the original saying is “a jack of all trades is a master of none, but oftentimes better than a master of one”, the ACURATE neo2 THV seems to be an interesting option, combining the advantages of self-expanding and balloon-expandable THVs in a single device. This could not only guarantee an “event-free” TAVI procedure for the patient but also an optimised landing zone for future interventions regarding skirt height and coronary accessibility.
Conflict of interest statement
J.-M. Sinning is proctor for Medtronic and Boston Scientific; receives research support from Boston Scientific, Edwards Lifesciences, and Medtronic; and speaker honoraria from Abbott, Abiomed, Boston Scientific, Edwards Lifesciences, and Medtronic.