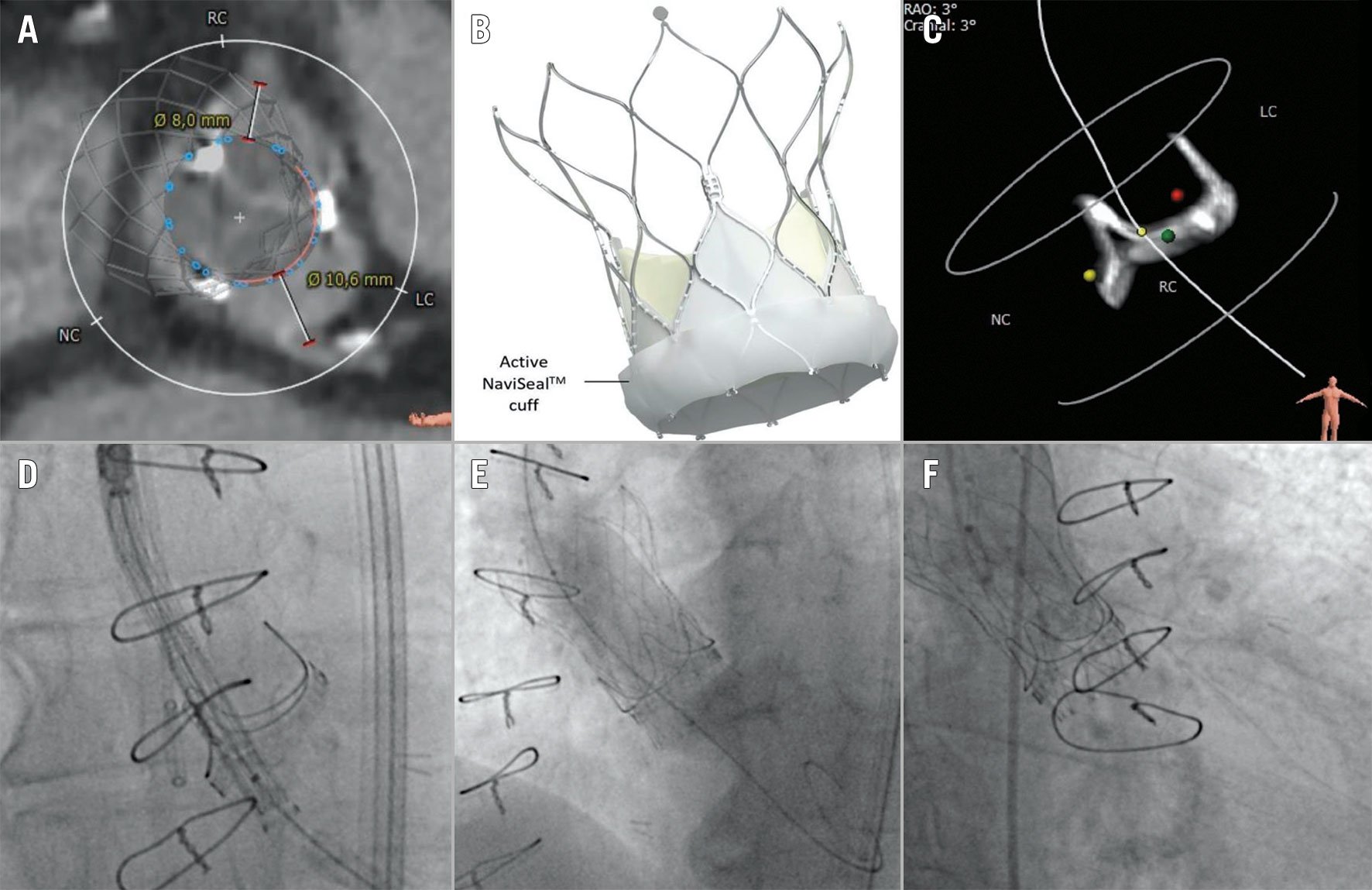
Figure 1. ViV with Navitor. A) Virtual THV-to-coronary ostial distances to the right (8.00 mm) and left (10.6 mm) coronary artery. B) New active outer NaviSeal cuff at the inflow part and the curved aortic outflow part of the Navitor THV. Image courtesy of and provided by Abbott. C) Cusp overlap view predicted by preprocedural CT by isolating the radiopaque bioprosthetic stent post between the LC and RC. D) Positioning of the radiopaque marker of the delivery catheter at the annulus level. Also note the alignment of both delivery catheter plane and surgical bioprosthesis annulus plane in the LC/RC cusp overlap view. E) Post-dilatation using a 22 mm True Dilatation balloon. F) Final position of the Navitor THV with no PVL. CT: computed tomography; LC: left coronary cusp; NC: non-coronary cusp; PVL: paravalvular leakage; RAO: right anterior oblique; RC: right coronary cusp; THV: transcatheter heart valve; ViV: valve-in-valve
A 67-year-old male was referred for valve-in-valve transcatheter aortic valve implantation (VIV-TAVI) due to the symptomatic, severe and structural deterioration of a 23 mm PERIMOUNT 2800 valve (Edwards Lifesciences) implanted 12 years earlier because of a severely stenotic bicuspid aortic valve. The latest transthoracic echocardiography showed a mean transprosthetic gradient of 80 mmHg, but no regurgitation. Preprocedural computed tomography (CT) revealed adequate virtual valve-to-coronary distances (>4 mm) (Figure 1A). The patient was scheduled for VIV-TAVI with a 25 mm Navitor transcatheter heart valve (THV; Abbott) under local anaesthesia. Compared to the Portico system (Abbott), this latest-generation Navitor THV (Figure 1B) has an active outer NaviSeal Cuff (Abbott) to prevent paravalvular leakage (PVL), to optimise radial force, and a curved aortic outflow part to mitigate the risk of aortic injury.
After placement of a SENTINEL device (Boston Scientific) for cerebral embolic protection, the Navitor THV was introduced within the FlexNav delivery system (Abbott) over a Safari small, preshaped stiff guidewire (Boston Scientific). The aortic arch and surgical aortic bioprosthesis were crossed without difficulty (Moving image 1). A left and right coronary cusp (LC/RC) overlap view, as predicted on the preprocedural CT by isolating the radiopaque bioprosthetic stent post between the LC and RC (Figure 1C), was used for deployment of the THV. There are multiple advantages to using the cusp overlap view: 1) the left ventricular outflow tract (LVOT) is elongated and thereby the real implantation depth can be visualised during THV deployment, 2) the THV and surgical bioprosthesis are typically aligned with the imaging plane (i.e., without parallax); and 3) the LC/RC cusp overlap view also allows THV implantation with patient-specific commissural alignment1.
The radiopaque positioning marker on the FlexNav delivery catheter was placed at the surgical bioprosthesis annulus level (Figure 1D). The deployment steps were identical to the Portico system, as previously described. The THV position remained stable throughout the entire deployment (Moving image 2). The THV was successfully implanted at a depth of 3 to 5 mm below the annulus. To ensure full expansion of the THV stent frame, post-dilatation was performed using a 22 mm True Dilatation balloon (Bard Peripheral Vascular)(Figure 1E). Post-deployment haemodynamic assessment revealed no residual transvalvular gradient. The final angiogram showed patent coronary artery flow, a mild degree of commissural misalignment and no PVL (Figure 1F, Moving image 3). Furthermore, there were no new postprocedural conduction abnormalities.
Several issues become important for younger patients with a longer life expectancy who are undergoing TAVI, including optimal haemodynamic performance, future access to the coronary arteries, and avoidance of conduction abnormalities. VIV-TAVI has been reported using the Portico system2 but this first report of VIV with the Navitor THV illustrates both the technical aspects as well as the favourable haemodynamic findings of this procedure. The large-cell stent design geometry and intra-annular valve design can preserve coronary access and facilitate future coronary intervention. This case also demonstrates that the LC/RC cusp overlap technique is feasible – and even preferable – during a VIV procedure with the Navitor THV, without compromising procedural safety or valve haemodynamics.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Crossing of the aortic arch and the surgical aortic bioprosthesis by the Navitor and FlexNav delivery system.
Moving image 2. Deployment of the Navitor transcatheter heart valve at the cusp overlap view.
Moving image 3. Final aortogram showing the position of the Navitor transcatheter heart valve.