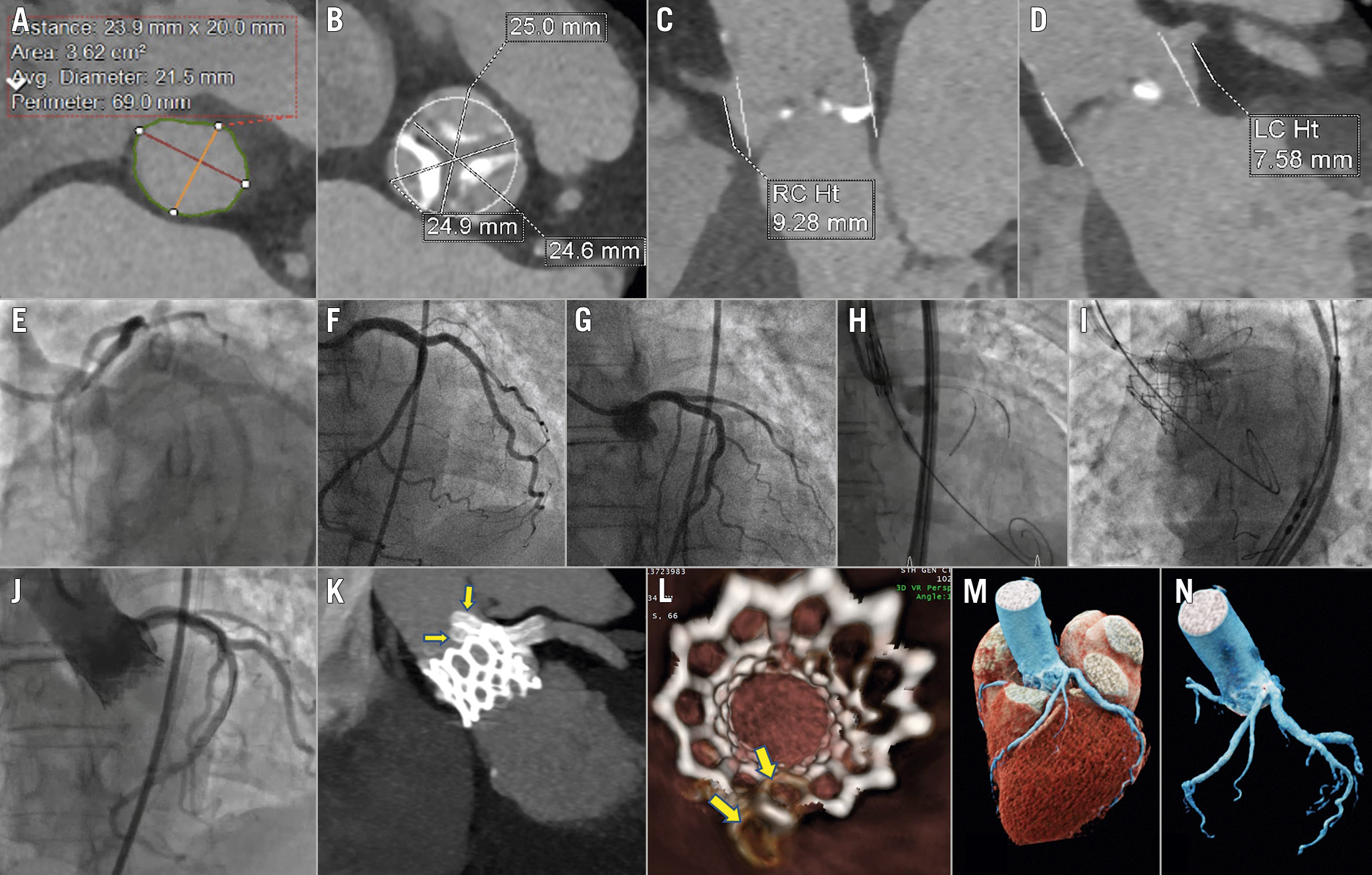
Figure 1. Chimney simultaneous kissing stenting after TAVI. A. Aortic annulus size (average diameter: 21.5 mm, area: 362 mm2, perimeter: 69 mm); B. Sinuses of Valsalva diameter: 25×24.9×24.6 mm; C. RCA – annulus distance: 9.28 mm; D. LMS – annulus distance: 7.58 mm; E. Non-selective coronary angiogram: absence of LMS with separate origin of the LAD and LCx coronary arteries; F. Selective angiography of the LCx prior to TAVI showing a normal vessel; G. Selective angiography of the LAD prior to TAVI showing a normal vessel; H. Secure positioning of the stents inside the vessels of interest (LAD and LCx) prior to valve deployment; I. Chimney PCI technique with simultaneous kissing stenting following post-TAVI acute LAD and LCx compromise: the stents are deployed simultaneously several mm before the origin of the LAD and LCx ostia and above the valve frame, on the grounds of keeping down the native aortic valve leaflet and maintaining patency of the LAD and LCx coronary arteries; J. Final angiography following successful stent implantation showing TIMI 3 flow in the LAD and LCx; K. CT coronary angiography showing the stents protruding outside the coronary ostia and along the TAVI bioprosthesis frame (yellow arrows); L. CT axial 3-dimensional reconstruction of the TAVI bioprosthesis and the stents. At 6 o’clock the two stents appear patent and well expanded, above the valve frame (yellow arrows); M. CT 3-dimensional anatomy of the left coronary system after TAVI and stent implantation; N. CT 3-dimensional anatomy of the left coronary system after TAVI and stent implantation. CT: computed tomography; LAD: left anterior descending artery; LCx: left circumflex artery; LMS: left main stem; PCI: percutaneous coronary intervention; RC/RCA: right coronary artery; TAVI: transcatheter aortic valve implantation
An 82-year-old female with symptomatic severe aortic stenosis was scheduled for a transcatheter aortic valve implantation (TAVI). A dedicated TAVI computed tomography (CT) scan demonstrated an aortic annular area of 362 mm2, perimeter of 69 mm and average diameter of 21.5 mm (Figure 1A). The sinus of Valsalva (SoV) diameter was 25 mm and the distances to the left main stem (LMS) and right coronary (RCA) arteries were 7 and 9 mm, respectively (Figure 1B-Figure 1D). Based on the small size of the SoV (<27 mm) and our better experience with balloon-expandable valves, our Heart Team consensus advocated for a 23 mm SAPIEN 3 Ultra (Edwards Lifesciences) implant and an upfront coronary artery protection strategy with a pre-TAVI guidewire and stent positioning in the coronaries due to an increased risk for acute coronary artery occlusion following TAVI. Coronary angiography before TAVI revealed a non-dominant, unobstructed RCA and the absence of the LMS with separate ostia of the left circumflex (LCx) and left anterior descending arteries (LAD) (Figure 1E-Figure 1G). As the RCA was hypoplastic with a small risk of occlusion, we decided only to protect the LAD and LCx with a single 8 Fr JL3.5 guiding catheter and simultaneous positioning of two 3.5x24 SYNERGY drug-eluting stents (Boston Scientific) (Figure 1H). Instead of a pigtail catheter, the JL3.5 was used to inject contrast dye during TAVI (Moving image 1).
Following TAVI, the patient developed widespread ST-depression, hypotension and chest discomfort. Due to a high suspicion of coronary obstruction, LAD and LCx stents were pulled back into the aortic root, thus traversing the LAD and LCx origins and the TAVI frame. Resolution of electrocardiographic changes confirmed leaflet obstruction of the LAD and LCx. We then performed a successful chimney simultaneous kissing stenting (SKS) establishing TIMI 3 flow in both vessels (Figure 1I-Figure 1J, Moving image 2).
To further evaluate correct stent positioning in relation to the valve frame, a CT coronary angiography (CTCA) was performed, which showed patent stents with good positioning along the bioprosthesis frame (Figure 1K-Figure 1N).
Since the introduction of CT for routine procedural planning, acute coronary occlusion after TAVI is uncommon, with a reported incidence of <1%12. The LMS is mostly involved (87%)12. Well-recognised risk factors include a short distance between the annulus and coronary ostia <10 mm and a narrowed aortic root <28 mm at the level of the SoV12. Both these factors increase the risk of displacement of the native aortic leaflets over the coronary ostia, with subsequent acute or late coronary occlusion. This is the first reported case of separate LAD and LCx ostia occlusion following TAVI, which was successfully negotiated with a single 8 Fr guiding catheter and chimney SKS. Furthermore, post-TAVI CTCA was useful to ensure a good stent positioning and an intact aortic valve bioprosthesis (Figure 1K-Figure 1N).
Although there is still lack of data regarding the long-term outcomes and stent patency after chimney PCI, the latter is a simple, effective and frequently used technique to achieve and maintain patency of the coronary arteries after abrupt coronary artery occlusion following TAVI3.
Conflict of interest statement
S. Redwood has served as a proctor for and received speaker fees from Edwards Lifesciences and has served on the advisory board for Medtronic. B. Prendergast has received unrestricted research and educational grants from Edwards Lifesciences and has received speaker/consultancy fees from Abbott, Anteris, and Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. The 8 Fr JL3.5 guiding catheter was used instead of the conventional pigtail catheter to inject contrast dye during TAVI to guide the valve deployment.
Moving image 2. Coronary angiogram after successful chimney PCI demonstrating normal TIMI 3 flow in LAD and LCx.