
Valve-in-valve interventions in Freedom Solo™ valves (Sorin Group [now LivaNova], Milan, Italy) are high risk due to the supra-annular stentless design, with long leaflets potentially jeopardising the coronary ostia1,2.
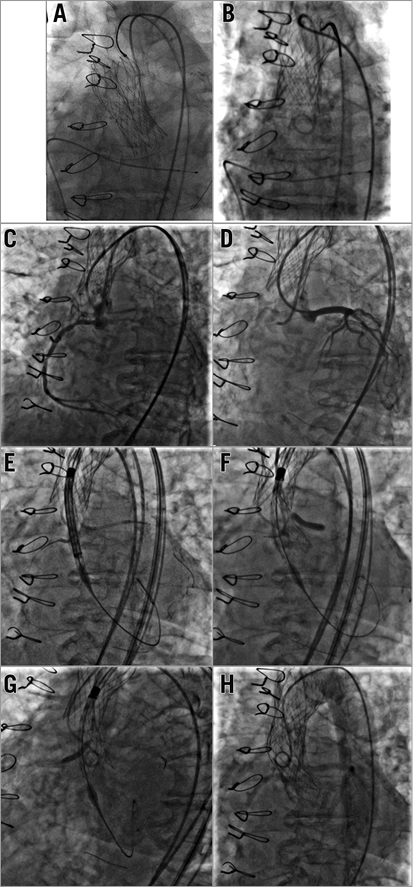
Three years previously, an 83-year-old lady had a 26 mm CoreValve® (Medtronic, Minneapolis, MN, USA) implanted inside a stenosed 23 mm Freedom Solo valve (the 23 mm CoreValve was then unavailable). Preliminary balloon valvuloplasty was performed with contrast aortography, confirming good coronary flow. A guide catheter was placed in the left main stem as a precaution. On deployment of the valve, however, the right coronary artery immediately occluded. The left coronary appeared to have good flow and was not stented but occluded upon guide withdrawal. The valve was therefore snared into the ascending aorta under conditions of cardiac arrest, relieving coronary obstruction (Panel A, Panel B). The patient improved significantly following this procedure.
Aged 86, she developed severe symptomatic valvular restenosis (peak gradient 80 mmHg, AVA 0.70 cm2, STS score 7.2) so we reluctantly agreed to re-attempt TAVI.
Right femoral artery access was achieved with a 14 Fr sheath. Cine and fluoroscopic image captures revealed the previous TAVI deployed in the ascending aorta (Panel B, Panel C). Both coronary ostia were simultaneously engaged (EBU3.5 for LCA, JR4 guide for RCA, Runthrough® floppy wires [Terumo Corp., Tokyo, Japan] to both) (Panel C, Panel D). 3.5x18 mm and 4x20 mm Resolute Onyx™ stents (Medtronic) were positioned in readiness in the RCA and LCA ostia, respectively (Panel E). A 23 mm Evolut™ (Medtronic) was taken around the aortic arch over a Safari™ wire (Boston Scientific, Marlborough, MA, USA), without the need for snaring the previous valve (Panel E). The CoreValve was incrementally deployed in a good position just below the Freedom Solo neoannulus (Panel F, Panel G) with serial contrast injections performed to confirm coronary artery patency. Through staged valve release, the LMS (Panel F) and RCA (Panel G) were stented with marginal overhang into the aorta. Once the valve was fully released, both stents were post-dilated to ensure no stent crush from the second TAVI. On this occasion, coronary flow was maintained following full valve release and guide catheter withdrawal (Panel H).
Practical implications
This represented a successful TAVI implant with no transvalvular/paravalvular leak of note by fluoroscopy or transthoracic echocardiography. The patient was discharged on warfarin (for atrial fibrillation [AF]), clopidogrel 75 mg OD for two weeks and aspirin 75 mg OD for life and remains clinically well at six-month follow-up. Careful planning of procedural strategy may help obviate potential complications when performing valve-in-valve interventions. Whilst this “chimney” stenting technique successfully protected the coronary ostia, this requires further scrutiny and should only be employed where no other viable options exist.
Conflict of interest statement
D. Hildick-Smith is a proctor for Medtronic. The other authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Redo TAVI into failing Freedom Solo valve.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Redo TAVI into failing Freedom Solo valve.

