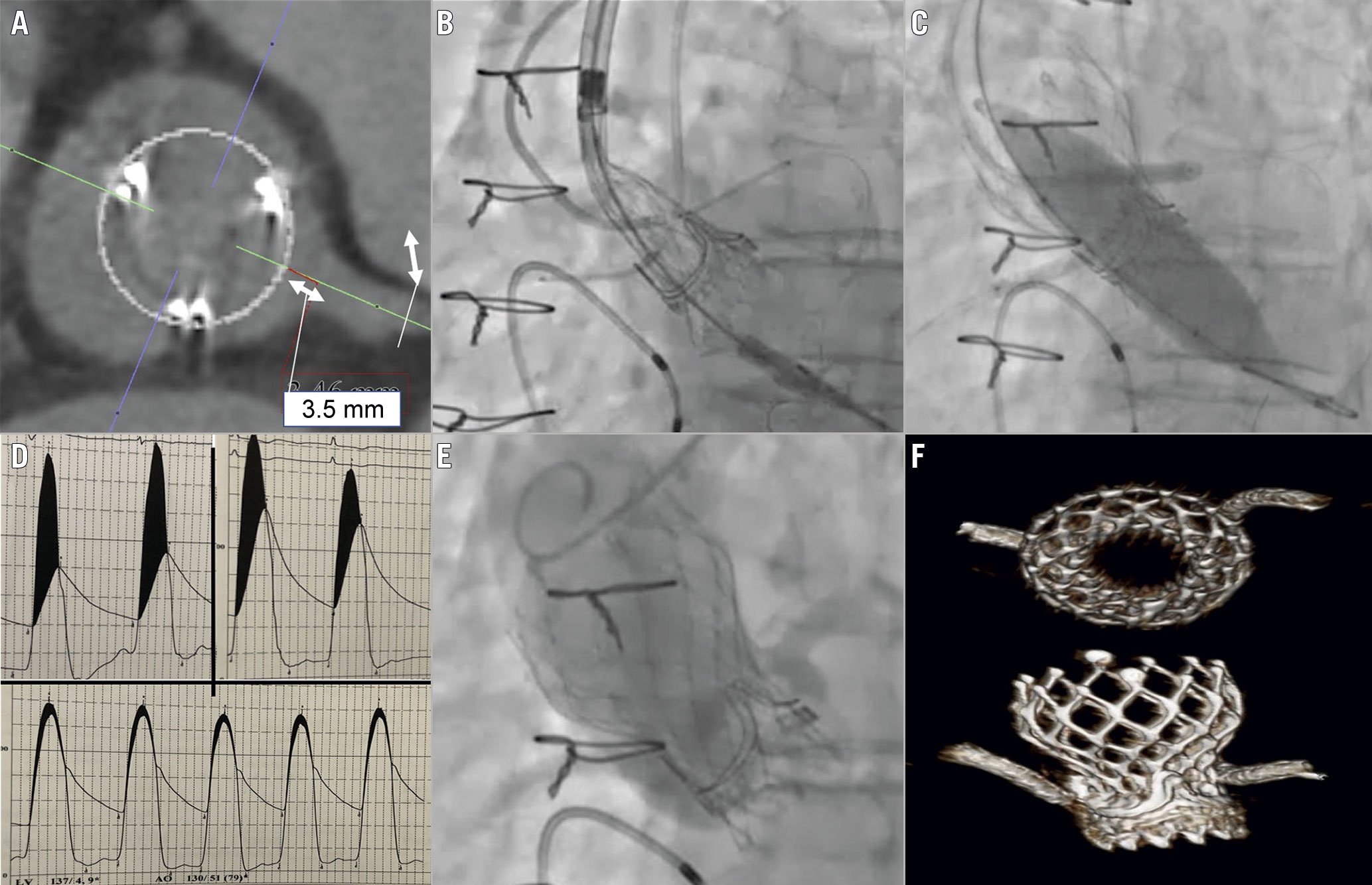
Figure 1. A novel way to prevent bilateral coronary obstruction in a high-risk case of valve-in-valve TAVI requiring balloon valve fracture. A) CT highlighted risk of bilateral coronary obstruction, with virtual THV to left coronary ostium (VTC) distance of 3.5 mm. B) Proximal segments of coronary stents protruding into the aortic root to cover the bioprosthetic valve leaflets. C) Inflated stent balloons followed by the 18 mm Atlas Gold balloon. D) MG dropped to 9 mmHg. E) Aortography demonstrated patent coronary arteries and no paravalvular leak. F) Post-TAVI CT showed a well-expanded THV with no stent deformation. CT: computed tomography; MG: mean gradient; TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve
Valve-in-valve (ViV) transcatheter aortic valve implantation (TAVI) is an established treatment for degenerated surgical aortic bioprostheses but carries an elevated risk of coronary obstruction1. Techniques to mitigate this risk include “chimney stenting”, where a coronary stent is deployed protruding into the ascending aorta, or BASILICA, where electrocautery is used to lacerate valve leaflets ensuring they splay either side of the coronary ostia when displaced by the transcatheter heart valve (THV). Bilateral chimney stenting or laceration of two leaflets can be undertaken when both coronary arteries are at risk23. However, neither technique has been reported when balloon valve fracture (BVF) is also required to obtain adequate THV expansion. We describe a novel approach to prevent coronary obstruction during ViV TAVI with BVF.
An 88-year-old female who had undergone surgical aortic valve replacement with a 19 mm Magna Ease (Edwards Lifesciences) bioprosthesis 14 years prior presented with dyspnoea. Transthoracic echocardiography revealed critical bioprosthetic valve stenosis with a mean gradient (MG) of 60 mmHg and valve area of 0.78 cm2. We planned ViV TAVI with a 23 mm Evolut PRO+ (Medtronic) followed by BVF. Computed tomography (CT) highlighted a risk of bilateral coronary obstruction, with a virtual THV to left coronary ostium (VTC) distance of 3.5 mm (Figure 1A), whilst the right coronary arose 7.2 mm above the bioprosthesis basal plane. Virtual THV to sinotubular junction distances were 0.9 mm and 5.0 mm above the left and right coronaries, respectively. Therefore, we undertook bilateral chimney stenting for coronary protection and triple kissing balloon inflation to prevent stent deformation during BVF.
A transfemoral approach and conscious sedation were used. 4.0×23 mm and 3.5×23 mm drug-eluting stents were positioned in the left and right coronary arteries, respectively, with the proximal segments protruding into the aortic root to cover the bioprosthetic valve leaflets (Figure 1B, Moving image 1). Once the Evolut PRO+ was released to 80%, the stents were deployed and balloons left in situ. The THV was then deployed and released. The MG was reduced from 65 to 54 mmHg, confirming the requirement for BVF. To prevent coronary stent deformation during BVF, we first inflated the stent balloons followed by the 18 mm Atlas Gold (Bard Peripheral Vascular) balloon (Figure 1C, Moving image 2). The Atlas Gold was then deflated prior to stent balloon deflation. The MG dropped to 9 mmHg (Figure 1D) and aortography demonstrated patent coronary arteries and no paravalvular leak (Figure 1E, Moving image 3). Post-TAVI CT showed a well-expanded THV with no stent deformation (Figure 1F). The patient was discharged without symptoms and was well at 30-day follow-up.
Chimney stenting presents a challenge for future coronary access as co-axial engagement may not be possible. Therefore, this approach may not be appropriate for young patients or those with coronary artery disease who may require future intervention. Since our patient was 88-years-old with normal coronaries, we deemed the likelihood of requiring future intervention to be low.
In conclusion, we demonstrate the feasibility and safety of double chimney stenting and triple kissing balloon inflation with BVF to prevent coronary obstruction during ViV TAVI. Given the unpredictable degree of valve expansion after BVF, this technique provides a novel strategy to optimise haemodynamics while maintaining coronary patency.
Conflict of interest statement
N. Fam is a consultant for Edwards Lifesciences, Abbott, and Cardiovalve. S. Alnasser receives consulting fees and speaker fees from Medtronic. M. Peterson receives consulting fees from Medtronic and is a proctor for Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Initial valve deployment. This clip shows the Medtronic Evolut Pro+ valve and coronary stents deployed, with stent balloons left in situ. Aortography shows patency of the coronary arteries, but the valve frame is significantly constrained by the surgical valve ring.
Moving image 2. Triple kissing balloon inflation. This clip shows the triple kissing balloon inflation which was used to prevent deformation of the coronary stents during balloon valve fracture. The balloons within the coronary stents were inflated prior to inflation of the Atlas Gold balloon. Fracture of the surgical valve ring, with resultant expansion of the Evolut Pro+ valve, can be seen.
Moving image 3. Final angiographic result. The frame of the Evolut Pro+ valve is visibly better expanded following balloon valve fracture. Aortography shows no paravalvular or intravalvular regurgitation and patency of the coronary arteries.