A 69-year-old male was referred to our centre for transcatheter aortic valve implantation (TAVI). He suffered from a severe aortic stenosis (NYHA Class III, multiple collapses) in addition to having a severely impaired left ventricular ejection fraction (20%), moderate mitral regurgitation, chronic obstructive pulmonary disease, and pulmonary hypertension. Multi-detector row computed tomographic imaging showed a calcified and tortuous aorto-iliac route, such that the Heart Team preferred to perform a transapical TAVI using a balloon-expandable Edwards SAPIEN valve (Edwards Lifesciences Inc., Irvine, CA, USA).
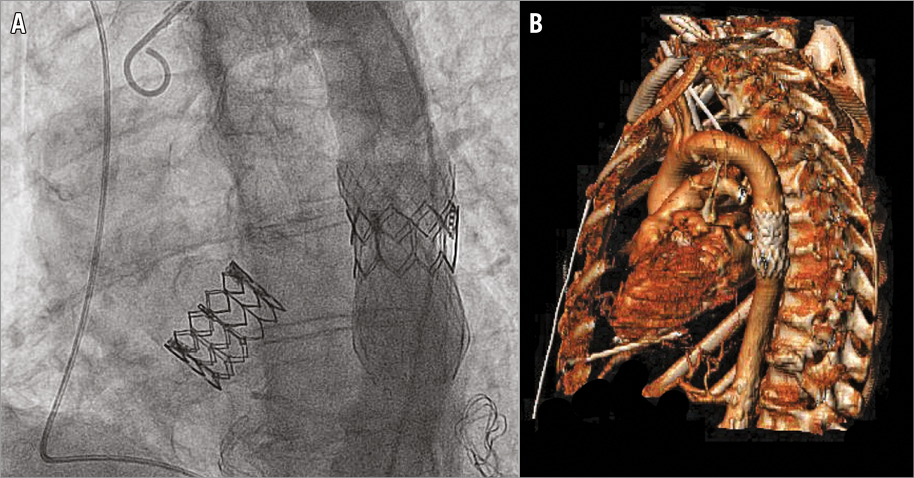
During the procedure, we exposed the cardiac apex using a small left anterolateral thoracotomy. After left ventricular puncture, we performed a balloon predilation during rapid right ventricular pacing (RVP) at 180 bpm. Upon subsequent implantation of the SAPIEN valve, RVP malfunctioned. Due to some missing beats, the valve dislocated into the ascending aorta (Moving image 1). We advanced the embolised device into the aortic arch for stabilisation (Moving image 2). Subsequently, a second SAPIEN valve was successfully implanted. Hereafter, the first device dislocated from the aortic arch. Upon advancing it into the descending aorta for stabilisation, the valve accidentally flipped 180°, completely blocking the blood flow (Moving image 3). Immediate action was required, but no vascular stents were immediately to hand. We prepared an improvised stent using a Medtronic CoreValve® (Medtronic, Minneapolis, MN, USA) prosthesis from which we removed the valve apparatus. Thereby, we were able to stent the SAPIEN valve in the descending aorta (Panel A, Panel B, Moving image 4).
This case is an illustrative example of the caveats of distally embolised prostheses, and provides an improvised solution for valve stenting in the acute setting.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Implantation.
Moving image 2. Embolisation.
Moving image 3. Fixation in the descending aorta.
Moving image 4. Implantation of the CoreValve.
Supplementary data
To read the full content of this article, please download the PDF.
Implantation.
Embolisation.
Fixation in the descending aorta.
Implantation of the CoreValve.