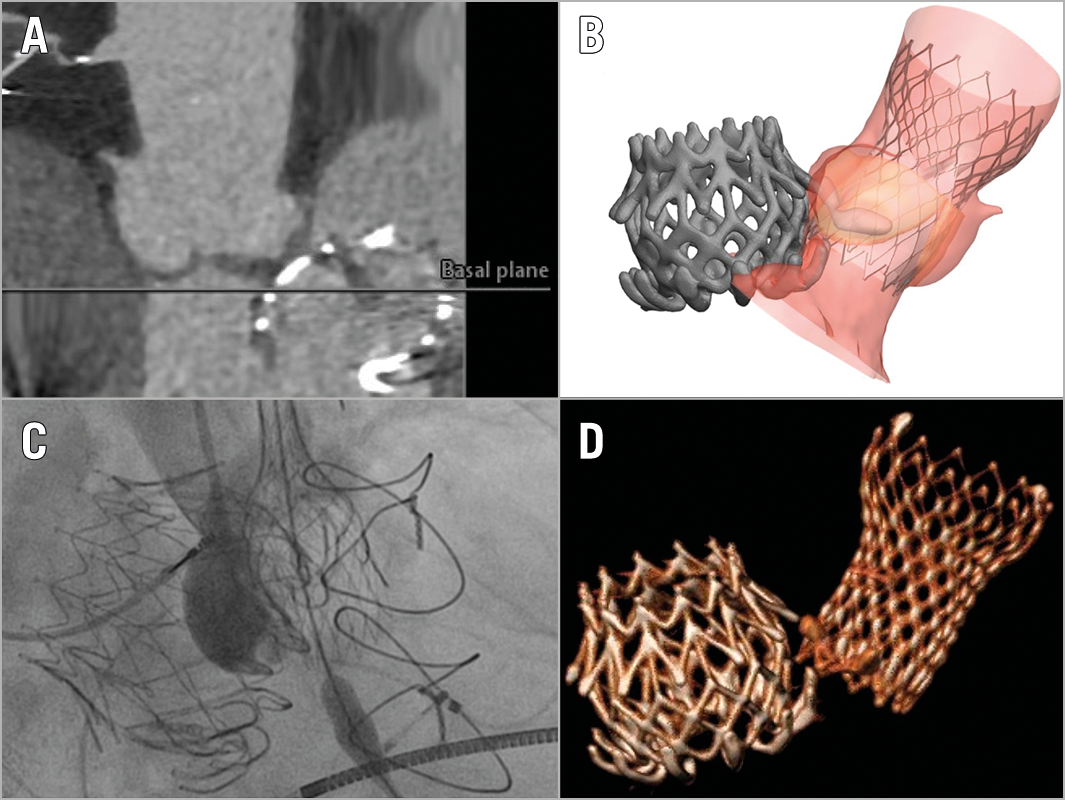
Figure 1. Planning and execution of transcatheter aortic valve implantation. A) Preprocedural CT scan illustrating a protrusion of the CardiAQ prosthesis into the LVOT. B) Preprocedural simulated implantation of Evolut prosthesis (FEops, Belgium). C) Intraprocedural fluoroscopic view with partial deployment of the prosthesis. D) Post-procedural CT scan analysis using 3mensio software (Pie Medical Imaging, Maastricht, the Netherlands) showing the final position of the two prostheses.
A patient was admitted with dyspnoea after prior transcatheter mitral valve implantation (TMVI) (CardiAQ; Edwards Lifesciences, Irvine, CA, USA)1. Echocardiography showed a good result after TMVI but revealed a low-flow low-gradient aortic valve stenosis on the basis of valvular calcification.
The patient was accepted for transcatheter aortic valve implantation (TAVI). Protrusion of the left ventricular anchors of the CardiAQ valve into the left ventricular outflow tract (LVOT) (Figure 1A) challenged the use of a balloon-expandable prosthesis since the stiffness of the CardiAQ valve was unpredictable. Simulated implantation using a self-expanding prosthesis (Figure 1B, Moving image 1) illustrated the optimal position. Transfemoral implantation of a 34 mm CoreValve® Evolut™ prosthesis (Medtronic, Minneapolis, MN, USA) was planned.
Intraprocedural echocardiography revealed a trivial paravalvular leak, a maximal pressure gradient of 9 mmHg and no alteration of the CardiAQ prosthesis (Figure 1C).
After two months, the patient presented with clinical improvement. Computed tomography (CT) analysis and echocardiography confirmed the desired position with no interaction with the CardiAQ valve (Figure 1D, Moving image 2).
Various devices have been successfully implanted in patients with prior MV surgery; mitral valve prostheses have been identified as a risk factor for TAVI-device embolisation2. This case presented with a protruded mitral prosthesis into the LVOT. Preprocedural simulation was helpful to assess the optimal position of the prosthesis. Intraprocedural post-dilatation would have been performed in case of a relevant paravalvular leak using a larger balloon but was not necessary since optimal positioning with further expansion of the valve due to the nitinol frame resulted in a good primary result.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Preprocedural simulation based on the routine computed tomography of the aortic root to assess the optimal positioning of the Evolut R prosthesis in relation to the CardiAQ valve illustrated using TAVIguide™ software (FEops nv, Ghent, Belgium).
Moving image 2. Parasternal long-axis echocardiographic view at two-month follow-up showing good flow patterns of both the mitral and aortic valve prostheses and with trivial paravalvular leak of the aortic prosthesis.