It is easy to imagine that the most important decisions made while caring for patients with multivessel disease or left main coronary artery disease (CAD) are made in the coronary catheterisation laboratory. There, critical decisions occur, including the determination of the optimal revascularisation strategy and the timing of revascularisation, with the appropriate focus on anatomical complexity and burden of disease. Implementing the best evidence and revascularisation guidelines, incorporating imaging and appropriate bifurcation strategies, in addition to determining the duration of dual antiplatelet therapy are all essential to ensure the best long-term outcomes. These complex patients require a well-trained, multidisciplinary high-risk Heart Team. But what other factors critically affect long-term mortality?
In the current issue of EuroIntervention, Hara et al1 present further data from the SYNTAXES extended survival study assessing the impact of preprocedural biological markers on 10-year mortality. In this study the investigators found that what we do for our patients outside of the catheterisation laboratory and operating room greatly impacts long-term mortality. They report that amongst SYNTAXES patients, the greatest predictor of 10-year mortality was not the biomarkers at presentation but rather the lack of statin use.
This post hoc analysis of the SYNTAX/SYNTAXES trial evaluated 1,800 patients with de novo 3-vessel disease and/or left main coronary artery disease. It examined the association between long-term survival and preprocedural biomarkers of inflammation (based on measures of C-reactive protein [CRP]), haemoglobin, HbA1c, renal dysfunction (based on creatinine clearance), fasting triglyceride, low-density lipoprotein and high-density lipoprotein cholesterol. At the 10-year follow-up, 1 in every 4 patients (460/1,800) in this high-risk patient group had died. The best predictor of being alive at 10 years was being on statin therapy. This was irrespective of the preprocedural lipid levels or CRP.
The SYNTAX score II and SYNTAX 2020 risk scores have been previously externally validated to predict mortality2. These scores include evaluation of anatomical complexity and prognostic variables including age, creatinine clearance, ejection fraction, gender, chronic obstructive pulmonary disease, peripheral vascular disease, medically treated diabetes, and current smoking. The earlier SYNTAX score had included sex in the risk assessment, while the SYNTAX 2020 score does not include sex in the mortality assessment.
Although creatinine clearance is already part of the SYNTAX 2020 score, using creatinine clearance as a binary variable with a cut-off at 60 ml/min remained predictive of 10-year survival. Hara et al1 also found that survival was associated with a lower baseline CRP and HbA1c, and higher haemoglobin. The association of these periprocedural biomarkers on extended survival was not dependent on the mode of revascularisation. Despite their association with survival, these investigators demonstrated that incorporating any of these preprocedural biomarkers into existing SYNTAX II or SYNTAX 2020 resulted in no significant improvement in the predictive value of these risk scores. This suggests that these preprocedural biomarkers do not add much beyond the established SYNTAX II 2020 score.
Nonetheless, addressing these noted preprocedural biomarkers as part of the secondary prevention after revascularisation to reduce possible residual risk may be the important implication of these findings. Chronic inflammation, as reflected by CRP, has long been recognised as an underlying cause of destabilisation of atherosclerosis3, and inflammation has re-emerged as a target of treatment to reduce residual risk in both stable coronary artery disease and acute coronary syndromes45. Chronic kidney disease (CKD) has a strong association with cardiovascular disease (CVD) and mortality6, but until recently there were no specific targeted therapies. Now, the identification of CKD can impact the choices of secondary preventive therapies78.
In the SYNTAXES population, having a HbA1c ≥6.0% was associated with long-term mortality, but only in patients without a pre-existing diagnosis of diabetes. Prior studies have demonstrated that people without previously diagnosed diabetes presenting with a HbA1c ≥6% are at a greater risk of developing diabetes, cardiovascular disease and all-cause death9. For patients with established diabetes, a preprocedural HbA1c ≥6.0% did not predict mortality. Nonetheless, an interruption in the medical treatment of diabetes was associated with a signal towards a higher risk of mortality (adjusted hazard ratio [aHR] 1.66, 95% confidence interval [CI]: 1.00-2.75). Interruptions in treatment for diabetes have been previously demonstrated to increase hospitalisations and mortality1011. In the SYTAXES trial1, more than half the patients had interruptions in their diabetes medications in the first 5 years of follow-up, which was more predictive of all-cause death than the preprocedural HbA1c itself.
Some limitations of this study exist and are acknowledged by the authors. The biomarkers studied were assessed at a single preprocedural time point. As such, any changes in these biomarkers as a result of specific therapies were not assessed. It should also be noted that medical therapies were not randomised or dictated by this study protocol; the randomisation was simply PCI vs CABG, and the only endpoint of the SYNTAXES extended follow-up trial was the association on all-cause mortality. Finally, as is often the case in studies reporting 10-year outcomes, medical therapies, stent technology and guideline recommendations have evolved since the enrolment of these patients. In particular, second- and third-generation drug-eluting stents (DES) have evolved and have demonstrated improved outcomes (compared with the first-generation DES employed in the SYNTAX trial) and are now almost universally used.
What do these findings mean for our patients and our practice? They emphasise the importance of treating the underlying cardiovascular disease mediators, not just the obstruction. These results particularly emphasise the importance of secondary cardiovascular disease prevention and the need for prescribing guideline-directed medical therapies (GDMT) after undergoing revascularisation, in addition to ensuring that patients continue these life-saving medications12. The reasons for not receiving statins or for disruptions in diabetes medications in these patients are complex. Regular medical follow-up, engagement of other healthcare partners in the community, enrolment in cardiac rehabilitation and ensuring affordability of guideline-directed medications are essential. Additionally, shared decision-making in clinical practice and clear communication to ensure that patients understand the role of the specific prescribed medications for their cardiac condition should become the standard practice of our healthcare teams before discharging patients after revascularisation (Figure 1). Without this approach, improvements in long-term survival post-revascularisation will be less likely, regardless of the quality of our careful and costly efforts made in our coronary catheterisation laboratories and surgical theatres.
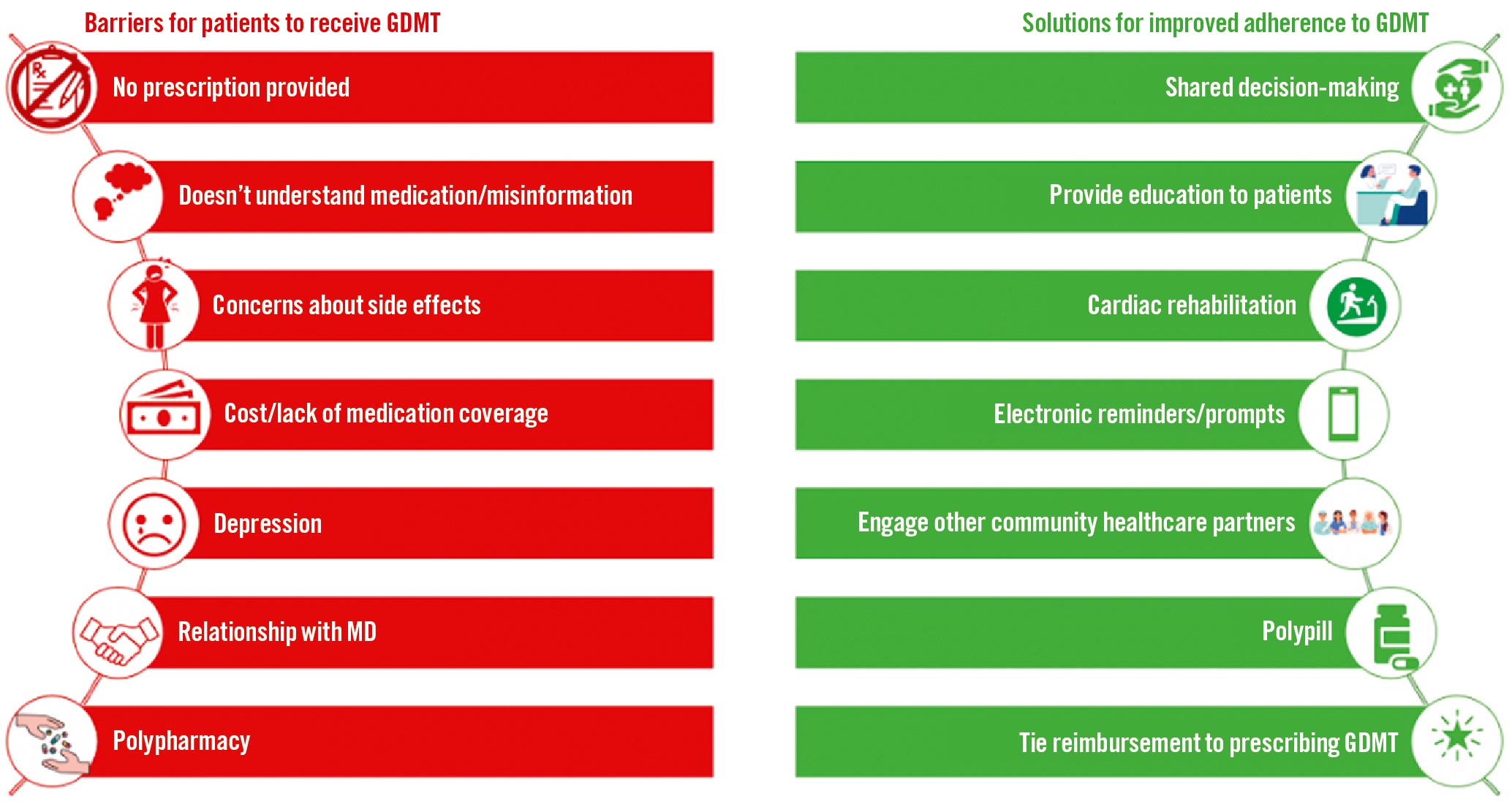
Figure 1. Guideline-directed medical therapies: barriers & solutions. GDMT: guideline-directed medical therapies
Future research needs to continue to examine prescribing practices after revascularisation and adherence to guideline-directed care. At discharge, 1 in 5 patients were not prescribed a statin in the SYNTAXES study. This low utilisation of statins is most likely higher than what would have been seen in real-world practice at the time of this trial. The American College of Cardiology's Practice Innovation and Clinical Excellence (PINNACLE) registry examined patients from 2009-2010 with obstructive coronary artery disease and reported that 22% of patients received statin therapy, but statin use was more likely in those with recent revascularisation and in men13. Despite their proven efficacy and the continued emphasis on them within our guidelines, statins continue to be under-prescribed and are inadequately dosed on discharge in the highest-risk patients with cardiovascular disease1415. Australian registry data suggest 45% of patients are not receiving high-intensity statin therapy in the 12 months after their acute coronary syndrome (ACS)16. In the US after ACS, adherence to lipid-lowering therapies is estimated to be between 60-70%, with lower adherence for women when compared with men17. The observed sex-based outcome gap for women with ACS is likely to be significantly impacted by observed differences in both prescribing for women with ACS and in subsequent adherence891011, although sex differences were unfortunately not examined in this study.
It would be easy to say we are in the golden era of cardiology, given that we have the tools to alter the progression and long-term prognosis of cardiovascular disease on a scale that cardiologists who came before us could only dream of. Nonetheless, interventional therapies are only as good as the secondary preventative therapies that follow them. We need to ensure utilisation of our proven guideline-directed medical therapies for all patients after revascularisation. One of the goals of the SYNTAX and SYNTAXES extended follow-up trials was to develop risk calculators to help predict prognosis, but if we cannot find a way to ensure that such high-risk patients are adequately medically managed after revascularisation to mitigate risk, we have failed to optimally use these risk calculators. The research done by Hara et al1 is yet another reminder that we must consistently treat patients in accordance with evidence-based medicine and accepted guidelines. The intervention we need to master is secondary prevention.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.

