Abstract
Aims: We sought to determine a reasonable level of revascularisation using the modified residual SYNergy between percutaneous coronary intervention (PCI) with TAXus and cardiac surgery (SYNTAX) score in patients undergoing PCI.
Methods and results: In 3,460 patients with multivessel disease receiving drug-eluting stents, residual SYNTAX score (rSS) was calculated for lesions with ≥50% diameter stenosis in vessels ≥1.5 mm after PCI. The “modified” rSS (mrSS) was determined by counting lesions with ≥70% diameter stenosis in vessels ≥2.5 mm only. Patients were categorised into the complete revascularisation (CR) group (rSS=0), the incomplete revascularisation (ICR) group (mrSS >0), or the reasonable ICR (R-ICR) group (rSS >0, but mrSS=0). After propensity matching, the R-ICR group (n=1,129) had a comparable risk of all-cause death (HR 0.80, 95% CI: 0.56-1.15, p=0.24) and a composite of all-cause death, myocardial infarction (MI), or repeat revascularisation (HR 0.91, 95% CI: 0.74-1.14, p=0.41) compared with the CR group (n=637) at three years. In separate propensity matching analyses, patients with R-ICR (n=1,280) had a lower risk of all-cause death (HR 0.73, 95% CI: 0.55-0.97, p=0.03) and a composite of all-cause death, MI, or repeat revascularisation (HR 0.68, 95% CI: 0.57-0.82, p<0.001) than those with ICR (n=837) at three years.
Conclusions: Complete revascularisation of lesions with ≥70% diameter stenosis in vessels ≥2.5 mm is better than ICR, and is a reasonable goal for patients with multivessel disease.
Abbreviations
CR: complete revascularisation
DES: drug-eluting stent(s)
FFR: fractional flow reserve
ICR: incomplete revascularisation
MI: myocardial infarction
mrSS: modified residual SYNTAX score
PCI: percutaneous coronary intervention
R-ICR: reasonable incomplete revascularisation
rSS: residual SYNTAX score
SYNTAX: SYNergy between PCI with TAXus and cardiac surgery
Introduction
Complete revascularisation (CR) of all diseased segments is a desirable goal in patients undergoing percutaneous coronary intervention (PCI). Despite this belief, there are conflicting data regarding whether CR is superior to incomplete revascularisation (ICR)1,2. Although CR can improve clinical outcomes by eliminating substantial myocardial ischaemia and preventing future revascularisation, multivessel revascularisation may result in an increased risk of in-stent restenosis3 and stent thrombosis4 as well as periprocedural complications5,6. Therefore, it is very important to determine a reasonable level of revascularisation. The SYNergy between PCI with TAXus and cardiac surgery (SYNTAX) score (SS) is an anatomic scoring system based on the coronary angiogram for quantification of lesion complexity7. The “residual” SYNTAX score (rSS), which is the sum of the points assigned to each coronary lesion producing ≥50% luminal obstruction in vessels ≥1.5 mm after revascularisation, quantifies completeness of revascularisation. It was reported that the rSS >8 was associated with adverse ischaemic outcomes after PCI8. However, the functional significance of intermediate lesions between 50% and 70% diameter stenosis9 or small vessel disease10 is undetermined. In a recent registry, patients who received revascularisation for all the diseased segments with diameters ≥2.5 mm had acceptable outcomes11. In addition, confirming whether or not the rSS is ≤8 (or another threshold) after PCI is inconvenient. Therefore, we developed a modified residual SYNTAX score (mrSS), which is calculated based on the lesions with ≥70% diameter stenosis in vessels ≥2.5 mm after PCI. We sought to determine a reasonable level of revascularisation using the mrSS in patients with multivessel disease undergoing PCI with drug-eluting stents (DES).
Methods
STUDY POPULATION
Consecutive patients who had multivessel disease and received at least one DES for coronary artery disease at Samsung Medical Center between January 2003 and December 2011 were included in this study. Patients who had undergone coronary artery bypass graft surgery before the index procedure were excluded. The decision on whether to perform CR or ICR was made by interventional cardiologists. Samsung Medical Center Institutional Review Board approved this study and waived the requirement for written informed consent for access to an institutional registry.
SYNTAX SCORES AND COMPLETENESS OF REVASCULARISATION
Preprocedural and post-procedural coronary angiograms were analysed at the angiographic core laboratory (Heart Vascular Stroke Institute, Samsung Medical Center, Seoul, Republic of Korea) using an automated edge-detection system (Centricity® CA1000; GE Healthcare, Chicago, IL, USA). Each coronary lesion with ≥50% diameter stenosis in vessels ≥1.5 mm was scored using the SS algorithm described fully elsewhere7. An rSS was determined as that remaining after completion of PCI. The mrSS was calculated by separately adding the individual scores of lesions with ≥70% diameter stenosis in vessels ≥2.5 mm after completion of PCI.
CR was defined as revascularisation of all coronary segments with ≥50% diameter stenosis in vessels ≥1.5 mm (rSS=0). Reasonable ICR (R-ICR) was defined as revascularisation of coronary segments with ≥70% diameter stenosis in vessels ≥2.5 mm but leaving lesions with 50%-70% diameter stenosis or in vessels of 1.5-2.5 mm (rSS >0 but mrSS=0). ICR was defined as having residual lesions with ≥70% diameter stenosis in vessels ≥2.5 mm (mrSS >0).
STUDY OUTCOMES AND FOLLOW-UP
Clinical outcomes included all-cause death, cardiac death, myocardial infarction (MI), target lesion revascularisation, repeat revascularisation, and a composite of all-cause death, MI, or repeat revascularisation at three-year follow-up.
Clinical, angiographic, procedural, and outcome data were recorded prospectively in our dedicated PCI registry by independent research personnel. Patients were followed up at one, six, and 12 months after their index procedure and annually thereafter. Additional information was obtained by telephone contact or medical records, if necessary. For validation, information about vital status was obtained up to December 2014 from the National Population Registry of the Korea National Statistical Office using a unique personal identification number.
STATISTICAL ANALYSIS
All variables were categorised according to completeness of revascularisation, such as CR, ICR, and R-ICR. Survival curves were constructed using Kaplan-Meier estimates at time to first event. Comparisons of three-year outcomes were performed using a log-rank test for overall trend and Cox regression models with Bonferroni adjustment for pairwise comparisons. Multivariable models for each outcome were constructed including variables with p-values <0.2 in univariate analyses, and irrelevant factors were removed to obtain parsimonious stable models. The model’s goodness of fit was verified based on the Schoenfeld residuals. To balance the patients for various clinical and demographic characteristics, we advocated the propensity score matching method in a pairwise manner. We considered all relevant variables as shown in Table 1 and Table 2, except some procedural variables such as the number, length or diameter of stents. The balance was deemed satisfactory when the standardised mean differences were less than 10% as well as the variance ratios of near 1.0 in all variables. The pairs were matched using many-to-one individual matching between the R-ICR and CR groups or between the R-ICR and ICR groups. Stepwise multivariable Cox regression analysis using backward elimination was performed to ascertain variables independently associated with all-cause death and non-target lesion revascularisation at three years in the patients treated with the R-ICR strategy. All tests were two-tailed, and p-values less than 0.05 were considered significant.
Results
PATIENT CHARACTERISTICS
Between January 2003 and December 2011, 3,844 patients with multivessel disease underwent PCI with DES at Samsung Medical Center. We excluded 384 patients because of previous coronary artery bypass graft surgery (n=192), inability to calculate the SS, rSS, or mrSS for technical reasons (n=187), and loss to follow-up (n=5). Paired SS, rSS, or mrSS were available in the remaining 3,460 patients (Figure 1).
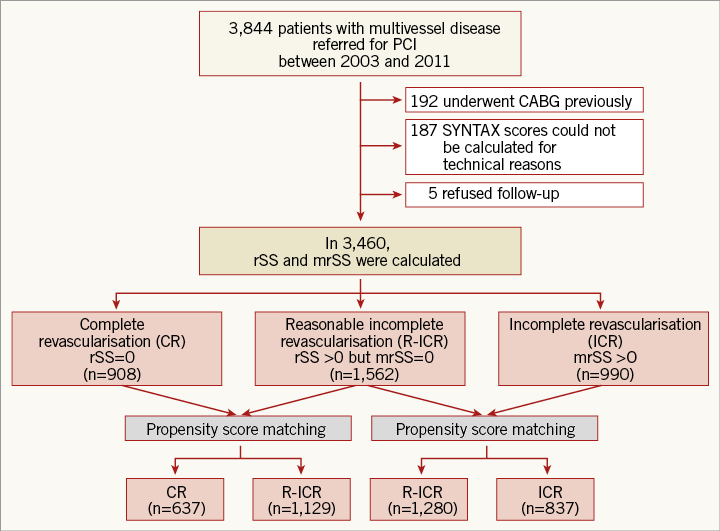
Figure 1. Patient flow. CABG: coronary artery bypass graft; CR: complete revascularisation; ICR: incomplete revascularisation; mrSS: modified residual SYNTAX score; PCI: percutaneous coronary intervention; R-ICR: reasonable incomplete revascularisation; rSS: residual SYNTAX score; SYNTAX: SYNergy between PCI with TAXus and cardiac surgery
CR was performed in 908 (26.2%) patients, R-ICR in 1,562 (45.1%) patients, and ICR in 990 (28.6%) patients. Among a total of 1,794 lesions treated in the CR group, 156 (8.7%) lesions were treated for 50%-70% diameter stenosis and 239 (13.3%) lesions were treated for vessels of 1.5-2.5 mm.
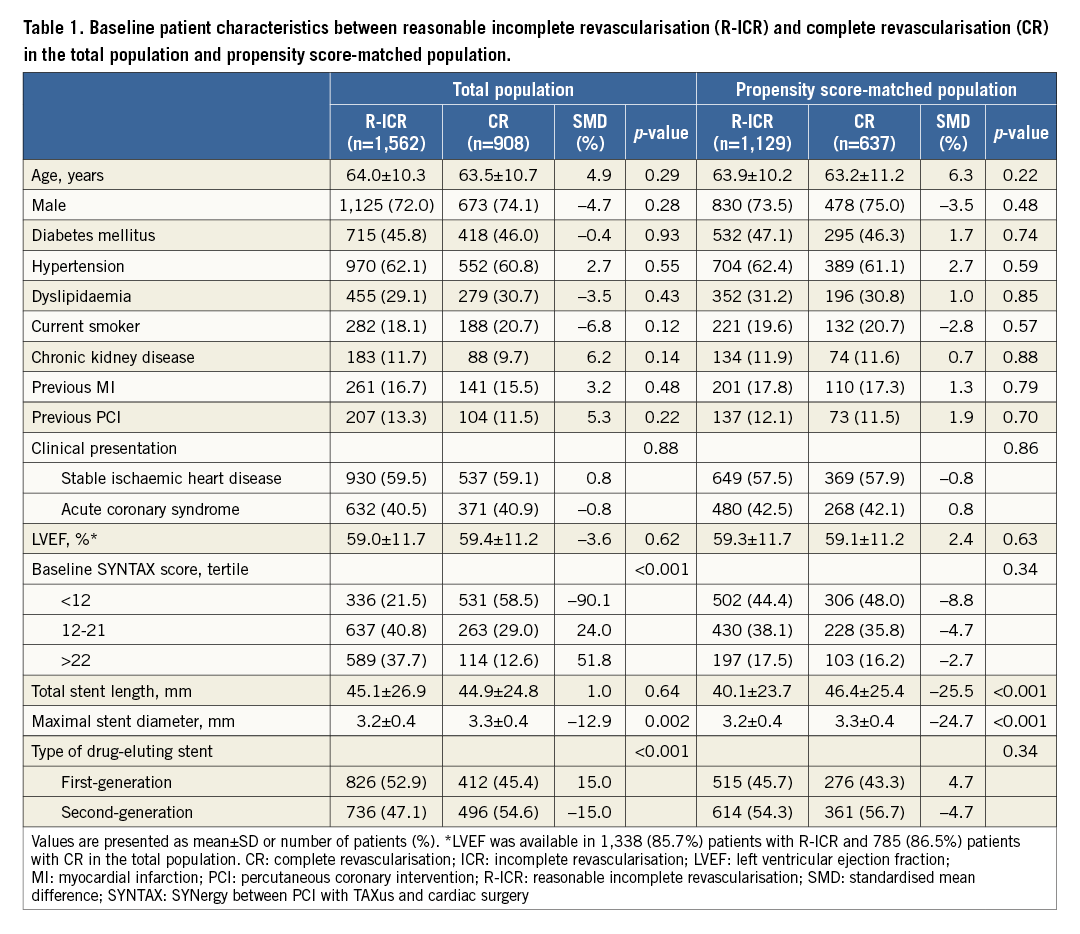
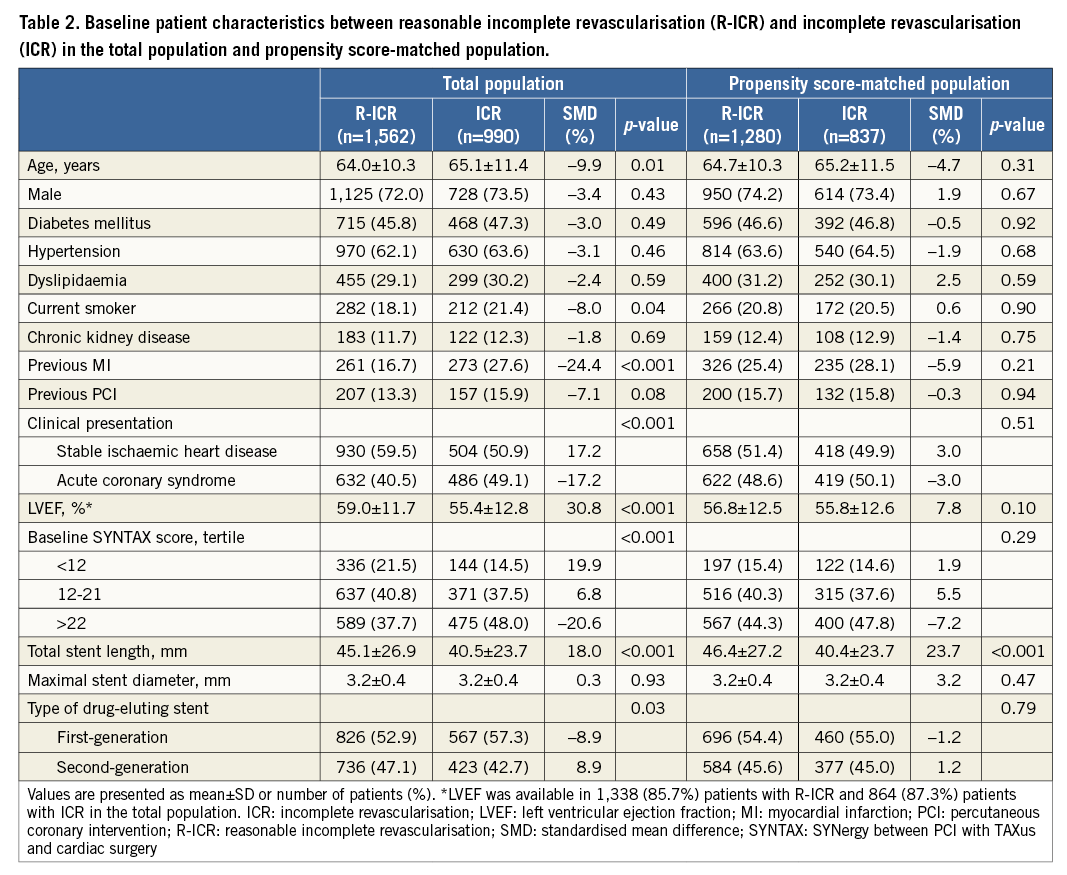
COMPARISON OF PATIENT CHARACTERISTICS BETWEEN THE R-ICR AND CR GROUPS
Compared with patients in the CR group, those in the R-ICR group had a greater prevalence of high tertile of baseline SS and received more first-generation DES (Table 1). After propensity score matching, we created matched pairs with 1,129 patients in the R-ICR group and 637 patients in the CR group. There were no significant differences in clinical, angiographic, and procedural characteristics between the R-ICR and CR groups after propensity score matching.
COMPARISON OF PATIENT CHARACTERISTICS BETWEEN THE R-ICR AND ICR GROUPS
Patients in the R-ICR group had low-risk characteristics of adverse ischaemic events compared with those in the ICR group: young age, high left ventricular ejection fraction, and less prevalence of current smoking, acute coronary syndrome, high tertile of baseline SS, and implantation of first-generation DES (Table 2). After propensity score matching, we created matched pairs with 1,280 patients in the R-ICR group and 837 patients in the ICR group. There were no significant differences in clinical, angiographic, and procedural characteristics between the R-ICR and ICR groups after propensity score matching.
STUDY OUTCOMES
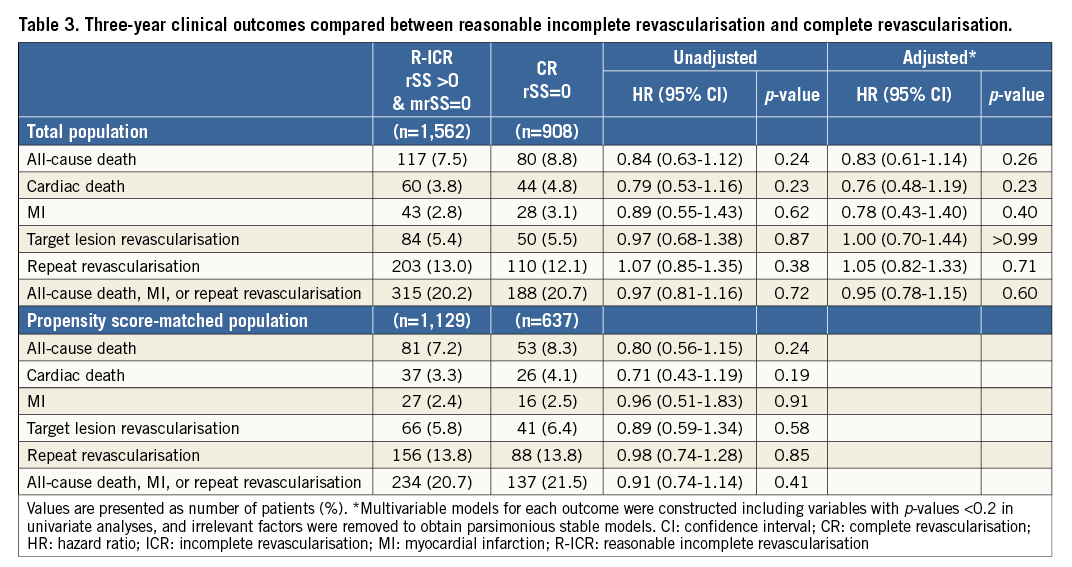
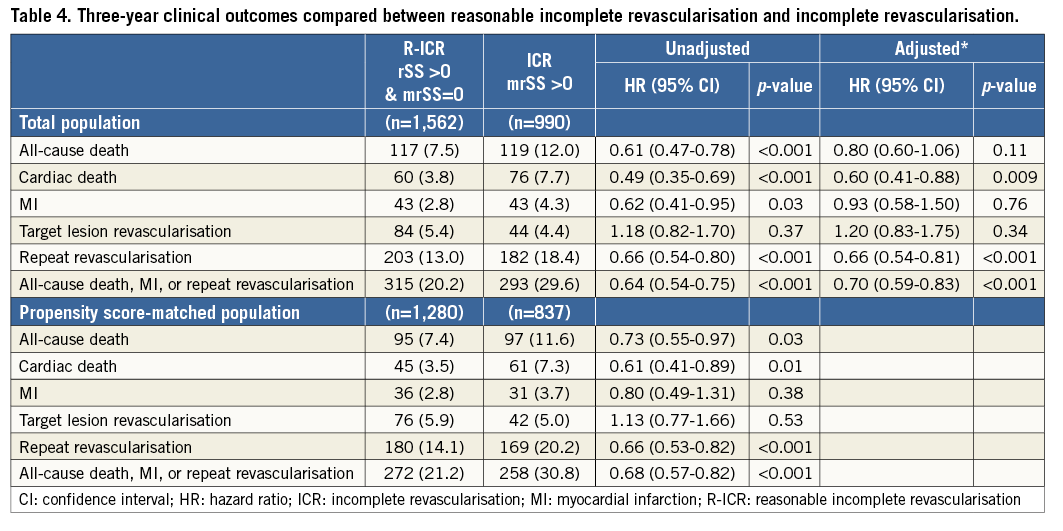
Follow-up data were available for 97.9% (3,079 of 3,144) of the eligible patients at three years after the index procedure. Cumulative event curves up to three years are shown in Figure 2. The cumulative rate of all-cause death was similar between the R-ICR and CR groups at three years. After propensity matching analyses, the R-ICR group had a comparable risk of all-cause death, as well as repeat revascularisation and a composite of all-cause death, MI, or repeat revascularisation compared with the CR group at three years (Table 3). Mortality at three years was numerically lower in the R-ICR group than in the ICR group. After propensity score matching, the R-ICR group had a lower risk of all-cause death, as well as repeat revascularisation and a composite of all-cause death, MI, or repeat revascularisation compared with the ICR group at three years (Table 4).
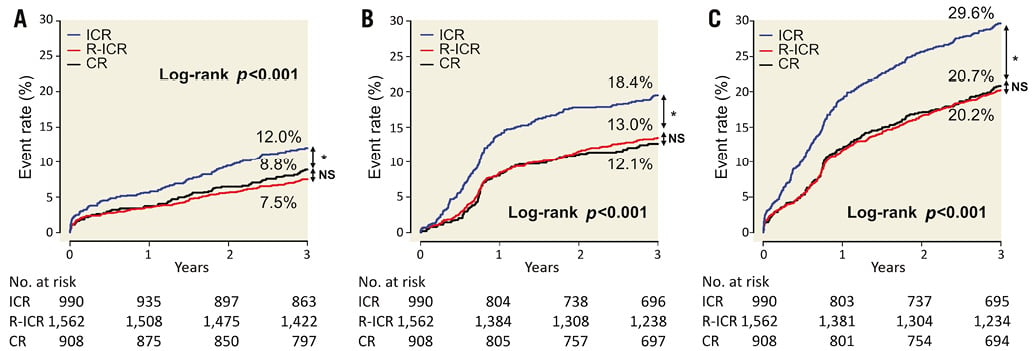
Figure 2. Kaplan-Meier curves for clinical outcomes at three-year follow-up. A) All-cause death. B) Repeat revascularisation. C) All-cause death, myocardial infarction (MI), or repeat revascularisation at three-year follow-up according to the completeness of revascularisation. *denotes p-values <0.001. CR: complete revascularisation; ICR: incomplete revascularisation; MI: myocardial infarction; NS: not significant (p-values >0.05); R-ICR: reasonable incomplete revascularisation
SUBGROUP ANALYSES
The risk of all-cause death at three years was comparable between the R-ICR and CR groups in various subgroups. However, there was significant interaction between treatment strategies and age, diabetes mellitus, and acute coronary syndrome (Figure 3). The R-ICR group had a lower risk of three-year mortality among patients of 70 years or older (interaction p=0.02), non-diabetic patients (interaction p=0.01), or those with stable ischaemic heart disease (interaction p=0.03). Compared with ICR, the favourable impacts of R-ICR on the risk of three-year mortality were consistent across various subgroups (Figure 4).
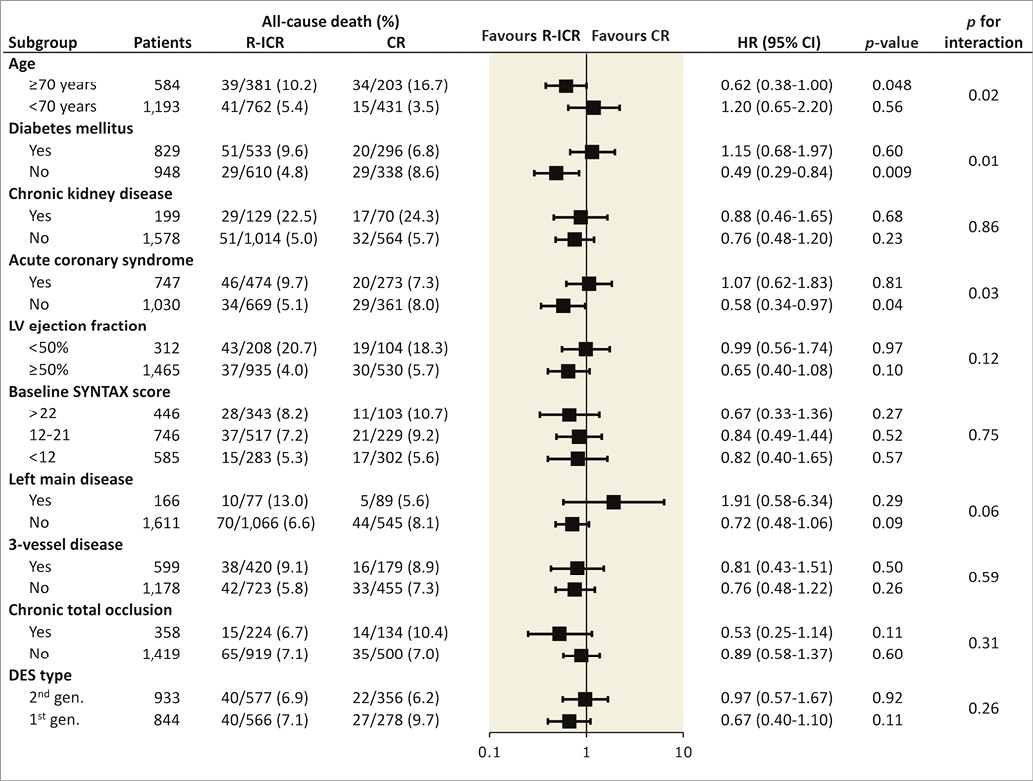
Figure 3. Impact of reasonable incomplete revascularisation (R-ICR) on three-year all-cause mortality across various subgroups in the propensity score-matched population, compared with complete revascularisation (CR). CI: confidence interval; CR: complete revascularisation; DES: drug-eluting stent; HR: hazard ratio; LV: left ventricle; R-ICR: reasonable incomplete revascularisation; SYNTAX: SYNergy between PCI with TAXus and cardiac surgery
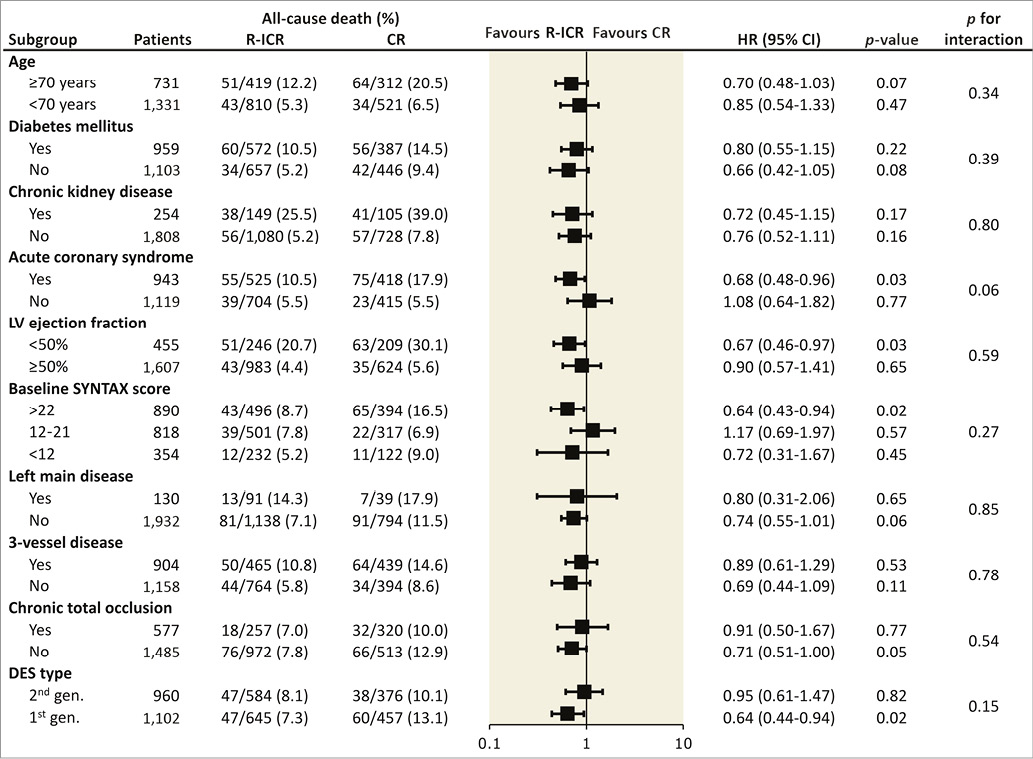
Figure 4. Impact of reasonable incomplete revascularisation (R-ICR) on three-year all-cause mortality across various subgroups in the propensity score-matched population, compared with incomplete revascularisation (ICR). CI: confidence interval; DES: drug-eluting stent; HR: hazard ratio; ICR: incomplete revascularisation; LV: left ventricle; R-ICR: reasonable incomplete revascularisation; SYNTAX: SYNergy between PCI with TAXus and cardiac surgery
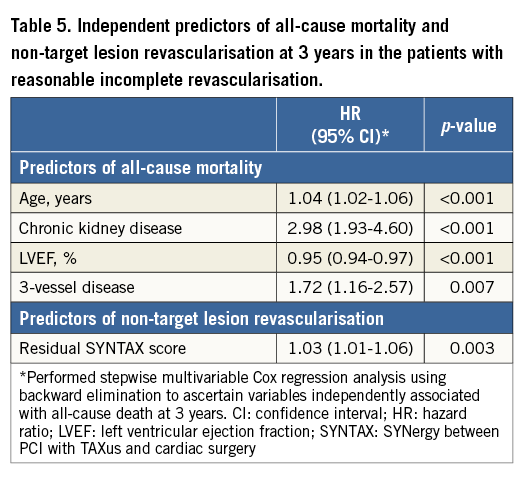
PREDICTORS OF ALL-CAUSE DEATH AND NON-TARGET LESION REVASCULARISATION AT THREE YEARS IN THE PATIENTS WITH REASONABLE INCOMPLETE REVASCULARISATION
The predictors of adverse events in patients having residual lesions with 50%-70% diameter stenosis or in vessels of 1.5-2.5 mm are presented in Table 5. Age, chronic kidney disease, left ventricular ejection fraction, and three-vessel disease were independently associated with all-cause mortality at three years. The rSS was an independent predictor of non-target lesion revascularisation at three years, but not all-cause mortality at three years.
Discussion
In this single-centre observational study, we proposed the mrSS and investigated the association between rSS, mrSS and clinical outcomes. The main findings of this study are that patients undergoing R-ICR (rSS >0 but mrSS=0) had similar clinical outcomes compared to those undergoing CR (rSS=0) and that R-ICR was associated with outcomes superior to ICR (mrSS >0). These findings suggest that PCI on intermediate lesions or small vessel disease can be safely deferred, and that revascularisation of only lesions with ≥70% diameter stenosis in vessels ≥2.5 mm (mrSS=0) is a reasonable goal for patients with multivessel disease.
A nuclear imaging study revealed that the magnitude of ischaemic burden was proportional to the risk of death or MI12. Therefore, CR may improve clinical outcomes by eliminating residual myocardial ischaemia and preventing future adverse events. However, multivessel PCI is associated with a greater risk of periprocedural complications such as cardiac enzyme elevation6 or contrast nephropathy5. Multivessel PCI may result in increased in-stent restenosis, leading to repeat revascularisation3, and stent thrombosis, because stent length has been reported to be a predictor of stent thrombosis4. Whether or not CR is necessary for favourable outcomes in patients undergoing PCI is still controversial1,2. Therefore, determining a reasonable level of revascularisation in patients with multivessel disease undergoing PCI is of great importance.
The rSS was developed to quantify the extent and complexity of residual coronary stenosis following PCI and to evaluate its impact on adverse ischaemic outcomes8. However, the rSS counts all the points assigned to each coronary lesion producing ≥50% luminal obstruction in vessels ≥1.5 mm after revascularisation. Achieving an rSS of zero may result in overly aggressive or unnecessary procedures. An rSS=0 was not associated with outcomes superior to those with rSS >0, suggesting that rSS=0 is not a reasonable goal. Some studies have reported that an rSS >8 is associated with adverse ischaemic outcomes after PCI8. However, patients with an rSS ≤8 may be quite heterogeneous, because intermediate lesions or multiple lesions in small vessels can have an rSS equal to a single significant lesion covering substantial territory. In our study, the rSS was not associated with mortality at three years in patients with intermediate lesions or small vessel disease. Moreover, confirming whether or not the rSS is ≤8 (or another threshold) after PCI is inconvenient. Therefore, we propose using the mrSS, which is calculated by adding the individual scores of lesions with ≥70% diameter stenosis in vessels ≥2.5 mm after PCI. Calculating the mrSS after PCI seems to be easier than calculating the rSS because lesions with <70% diameter stenosis in any vessels or any diameter stenosis in vessels <2.5 mm are ignored for the mrSS.
In the present study, patients undergoing R-ICR showed similar clinical outcomes to those undergoing CR. This finding is supported by other studies. Only 35% of lesions with stenosis between 50% and 70% were found to be functionally significant by fractional flow reserve (FFR)9, and long-term outcomes after deferral of PCI of intermediate lesions without functional significance were excellent13. Only one third of the lesions seen in small vessels turned out to be functionally significant10. Because small vessels generally supply limited myocardial mass, residual vascular lumen with angiographically significant stenosis might still be sufficient to maintain perfusion to the subtended myocardial territory14. PCI of small vessel disease introduces unexpected device-related disease, such as stent thrombosis and bleeding secondary to prolonged dual antiplatelet therapy. Taken together, these findings indicate that PCI on intermediate lesions or small vessel disease can be safely deferred, and patients with an mrSS=0 after completion of PCI would have favourable outcomes. However, ICR (mrSS >0) was associated with an increased risk of all ischaemic adverse events. Therefore, revascularisation needs to be attempted for lesions with ≥70% diameter stenosis in vessels ≥2.5 mm.
Compared with ICR, the favourable impact of R-ICR on the risk of three-year mortality was consistent across various subgroups, which is in line with the results of a recent left main disease registry11. A possible explanation is that the R-ICR strategy reduces the residual ischaemic burden compared with the ICR strategy while avoiding procedure-related complications compared with the CR strategy. Interestingly, the treatment effect varied depending on age, presence of diabetes mellitus, and clinical presentation between the R-ICR and CR group. Compared with CR, R-ICR had a favourable impact on three-year mortality among patients of 70 years or older, non-diabetic patients, or those with stable ischaemic heart disease. The functional significance of intermediate lesions or small vessel disease might be lower in elderly patients with limited activity; however, they are prone to PCI complications or comorbidities requiring interruption of antiplatelet therapy. Non-diabetic patients appear to have a decreased tendency for atherosclerotic rupture compared to diabetic patients, and it is possible that the progression of atherosclerosis might be slow in non-diabetic patients15. It is well known that PCI, as compared with optimal medical therapy, cannot reduce the risk of mortality in patients with stable ischaemic heart disease16. A conservative revascularisation strategy such as R-ICR might be reasonable in patients with stable ischaemic heart disease. However, these findings from subgroup analyses might have happened by chance, and should be interpreted with caution.
Limitations
This study has limitations inherent to its non-randomised, observational design. First, the SS, rSS, and mrSS were retrospectively assessed using an institutional registry. Most clinical decisions were based on visual analysis of the angiogram, and the external reproducibility of the study findings may be limited. Second, baseline characteristics were significantly different among the three groups. The selection of treatment strategies was at the discretion of the operators. In addition, incomplete revascularisation itself has a negative impact on long-term clinical outcomes. Although we performed propensity score-matched analyses to adjust for these potential confounding factors, we were not able to correct for unmeasured variables. Third, we did not measure FFR systematically before and after PCI. However, although FFR-guided PCI improved clinical outcomes compared with angiography-guided PCI, the majority of PCI procedures are still performed based on coronary angiographic findings17. Moreover, FFR may be influenced by revascularisation of other lesions and needs to be measured repeatedly after PCI to determine the functional significance of residual lesions. Our results have practical implications for determining which vessels can be left non-revascularised without FFR. Nevertheless, FFR measurement after PCI might be helpful to determine the prognostic significance of the mrSS.
Conclusions
R-ICR had favourable clinical outcomes compared with ICR, and had similar clinical outcomes compared with CR. These results suggest that complete revascularisation for patients with multivessel disease is a reasonable goal, treating all lesions with ≥70% diameter stenosis in vessels ≥2.5 mm. The mrSS can be a useful tool to determine a reasonable level of revascularisation in patients with multivessel disease undergoing PCI.
| Impact on daily practice Revascularisation of only lesions with ≥70% diameter stenosis in vessels ≥2.5 mm is a reasonable goal for patients with multivessel disease. |
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI10C2020).
Conflict of interest statement
J-Y. Hahn has received research grants from the Ministry of Health & Welfare, Republic of Korea, the Korean Society of Interventional Cardiology, and the Sungkyunkwan University Foundation for Corporate Collaboration, and speaker’s fees from Abbott Vascular, AstraZeneca, Daiichi Sankyo, Lilly, Pfizer, and Sanofi-Aventis. H-C. Gwon has received research grants from Abbott Vascular, Boston Scientific, Biotronik, and Medtronic, and speaker’s fees from Abbott Vascular, Boston Scientific, and Medtronic. The other authors have no conflicts of interest to declare.