Abstract
Aims: There is some evidence to suggest that incompleteness of coronary artery revascularisation after PCI is associated with inferior outcomes. The SYNTAX score was developed as a tool to quantify the extent of coronary artery disease in the SYNTAX study. We aimed to use this score to quantify the completeness of revascularisation after PCI (the “residual SYNTAX score”) and to determine its impact upon mortality.
Methods and results: We studied 240 consecutive patients with native three-vessel disease who underwent PCI between 2003 and 2008. SYNTAX scores prior to, and after, PCI were calculated, the difference (ΔSYNTAX) being a measure of the relative completeness of revascularisation. Median follow-up was 2.6 (1.2-3.2) years; 21% of patients were surgical turndowns, and 38% were non-elective. A residual (rSYNTAX) score of zero (full revascularisation) was achieved in 40% and median rSYNTAX was 3.5 (0-10.9). At final follow-up reduced mortality was found in patients with rSYNTAX 0 vs. others (2.5 vs. 12%, respectively, p=0.003) and for those with rSYNTAX
Conclusions: The residual SYNTAX score is a useful method to quantify incomplete revascularisation in patients undergoing PCI for 3VD. Complete revascularisation (rSYNTAX=0) is achieved in only a minority and, for them, the mortality rate is low.
Introduction
Patients with three-vessel coronary disease (3VD) may be revascularised by coronary artery bypass surgery (CABG) or percutaneous coronary intervention (PCI). The SYNTAX (Synergy between PCI with TAXUS and Cardiac Surgery) study showed that, in patients with 3VD, with or without left main stenosis, PCI with drug-eluting stents was associated with equivalent mortality to CABG, at the expense of a greater risk of repeat revascularisation, but with a reduced risk of stroke. In that study, the composite endpoint was more frequent in the PCI group for patients with high SYNTAX scores, although the difference was driven by more frequent repeat revascularisation rather than mortality1. The importance of completeness of revascularisation is well documented for CABG2-4, but less so for PCI5. The level of complete revascularisation in the SYNTAX PCI arm was 56.7%, in the CABG arm 63.2%, and in the parallel PCI registry 36.5%1. For patients presenting with non-ST-elevation acute coronary syndromes (NSTE-ACS), about 40% have multivessel disease and are treated by PCI. In current practice, a third of these receive multivessel PCI, and the remainder “culprit” vessel PCI6, even though a single culprit lesion is confidently identified in <50% patients7. No major studies have prospectively studied the effect of incomplete revascularisation in NSTE-ACS; but a few report favourable results for multivessel PCI6,8-12. For patients presenting with ST-elevation myocardial infarction (STEMI), both the European Society and American College of Cardiology guidelines recommend culprit angioplasty only, although a number of retrospective and descriptive studies have assessed the impact of complete revascularisation during the index procedure or staged at a later date with variable outcome13-18, and appropriate prospective studies are underway.
Completeness of revascularisation by PCI is often limited by the chance of technical success in treating adverse lesions such as chronic occlusions. Those patients in whom complete revascularisation is most difficult may therefore be those at highest risk of adverse events, possessing more complex coronary anatomy and additional risk factors such as age, renal impairment and extra-cardiac arteriopathy than others1,19,20. As a consequence, many of these patients are also not fit to undergo CABG, and PCI may be their only option for revascularisation, notwithstanding a high SYNTAX score.
It is important to know whether complete revascularisation affects outcome in the “real world” and, if so, what level of incomplete revascularisation is acceptable. Our hypothesis was that patients who were completely revascularised would achieve superior survival in the short and medium term. To address this question, we used SYNTAX scores and the novel concept of “residual” SYNTAX (rSYNTAX) scores to quantify the level of revascularisation achieved by PCI.
Methods
PATIENTS
This was a retrospective analysis of a prospectively constructed registry of consecutive patients with three-vessel disease (3VD) presenting to a single operator for PCI in the period 2003 to 2008. The setting was a single public tertiary cardiothoracic centre with a catchment population of 1.8 million, which undertakes about 1,600 PCIs and 900 CABGs per year. All patients had a standard indication for revascularisation, and standard contraindications to PCI (such as terminal cancer). All those patients with 3VD suitable for angioplasty were offered PCI; those who were suitable for CABG or PCI were offered both modalities, and those unsuitable for CABG but requiring palliation were offered PCI. The only group not offered PCI comprised patients who were good surgical candidates but in whom PCI would have been hazardous (e.g., occluded RCA and stenosed LMS). Therefore, included in this study were elective, urgent and emergency patients, surgical turndowns, patients presenting with STE-ACS and NSTE-ACS, and those in cardiogenic shock. “Elective” was defined as patients with stable symptoms undergoing a planned procedure, “urgent” was defined as PCI performed as an in-patient on the next available planned session, usually for NSTE-ACS, and “emergency” as PCI performed as soon as possible, usually for STEMI or cardiogenic shock. Full revascularisation was attempted, by default, at the index procedure. When this was not possible, a “staged” procedure was defined as angioplasty performed to complete a plan of revascularisation rather than due to treat new symptoms and was regarded as part of the index procedure. Baseline demographic and clinical parameters were obtained from hospital records, the catheter laboratory database and the operator’s procedural records. 3VD was defined as significant disease of all three main epicardial coronary arteries, or a significant branch thereof, the left main stem counting as two vessels. Patients with patent bypass grafts were excluded, because the SYNTAX score does not include grafts. Patients with severe aortic stenosis were also excluded from the study group because this condition was expected to impact upon outcome independent of their coronary disease, with or without subsequent valve surgery.
CLINICAL RISK
Major clinical comorbidities were recorded for each patient. STEMI and NSTE-ACS were defined according to standard criteria. Renal failure was defined by a serum creatinine >200 µmol/L at the time of procedure or pre-existing renal replacement therapy. Peripheral vascular disease was defined as extra-cardiac arteriopathy causing symptoms, requiring interventional treatment or proven by imaging. Left ventricular systolic function was recorded where available from echocardiographic data or ventriculography and recorded as normal or impaired. Impairment of LV systolic function was defined as ejection fraction <55% by visual assessment of left ventriculography or by standard echocardiographic methods. Chronic lung disease was defined as irreversible loss of lung function causing symptoms, and proven by pulmonary function testing, with forced expiratory volume of <1 L/s or a requirement for domiciliary oxygen. Body mass index was calculated. Both the New York PCI risk score21 and the logistic EuroSCORE22 were calculated.
PROCEDURES
A policy of maximum feasible revascularisation in one procedure was followed. Reasons for not achieving full revascularisation were recorded. PCI was conducted according to standard best practice. Patients received standard dual antiplatelet therapy (aspirin and clopidogrel) prior to the PCI, with 600 mg clopidogrel as the default loading dose. There was liberal use of periprocedural glycoprotein IIb/IIIa inhibitors, drug-eluting stents and intra-aortic balloon counterpulsation. Successful PCI to a target vessel was defined by the achievement of TIMI 3 flow with <50% residual diameter stenosis by eye. Procedural data were extracted from the prospectively kept operator’s records, patient notes and the catheter laboratory database.
LESION SCORING
Baseline SYNTAX and rSYNTAX scores were evaluated by two senior operators examining digitally archived diagnostic and procedural angiograms, offline. The SYNTAX score was calculated using an online calculator (www.syntaxscore.com, version 2.1). A high SYNTAX score was defined as >32, the figure identified in the SYNTAX trial as the lower limit of the highest tertile1. The rSYNTAX score was calculated by subtracting the score of each successfully treated lesion from the baseline total score. ΔSYNTAX was defined as the difference between baseline SYNTAX and rSYNTAX. The rSYNTAX score, therefore, comprised the score accumulated by any untreated lesions, a score of 0 indicating complete revascularisation. A bifurcation lesion was considered successfully treated if the main vessel residual stenosis was <50% with TIMI 3 flow and the side branch was patent, even if the residual stenosis in the side branch was angiographically severe. The only exception was the LMS bifurcation, for which success was defined by both branches (LAD and LCX) attaining residual stenoses <50%. The rSYNTAX of a chronic total occlusion (CTO) was recalculated if the vessel was successfully opened to reveal untreated distal disease. Examples are shown in Figure 1 - Figure 4.
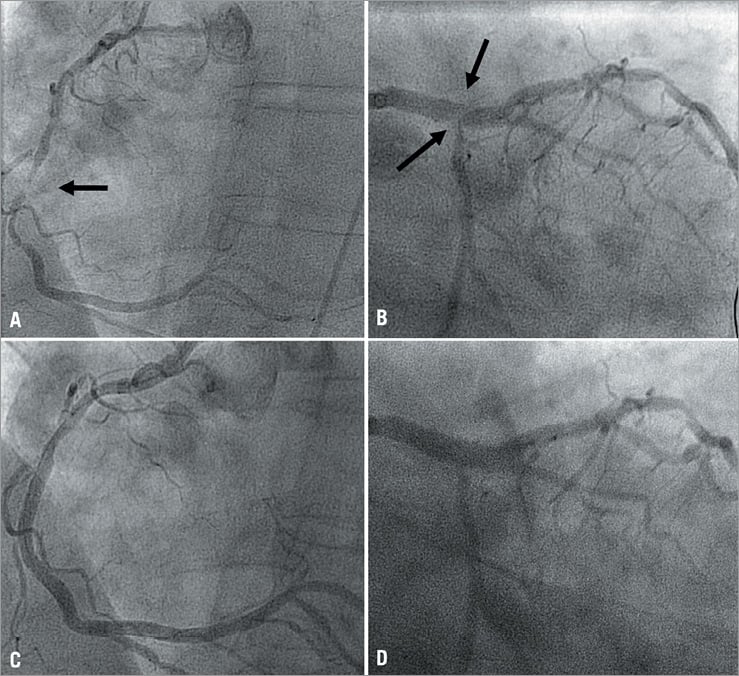
Figure 1. Example of patient with 3VD with low rSYNTAX score. A 69-year-old man presented as an emergency with inferior STEMI and a history of peripheral vascular disease, coeliac disease and cystic renal disease. The baseline SYNTAX score (panels A and B), with lesions in RCA and LMS, was 15. After treatment of all the lesions, the rSYNTAX score (panels C and D) was 0.
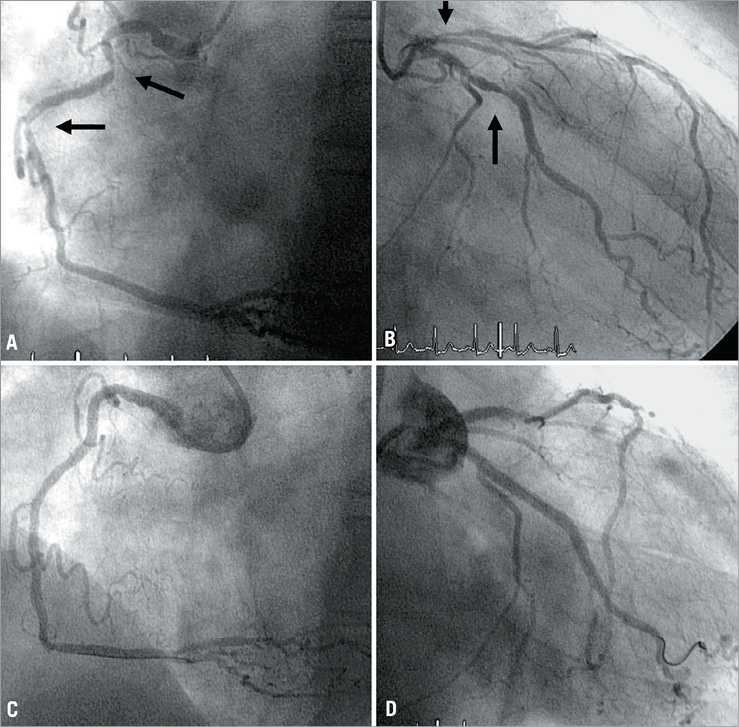
Figure 2. Example of a patient with 3VD with low rSYNTAX score. A 79-year-old man presented with NSTEMI (8 mm anterolateral ST-segment depression) five days after orthopaedic surgery. He had a history of chronic stable angina. He was anaemic. The baseline SYNTAX score (panels A and B), with lesions in RCA, LAD and Cx, was 19. After treatment of all the lesions (panels C and D), the rSYNTAX score was 0.
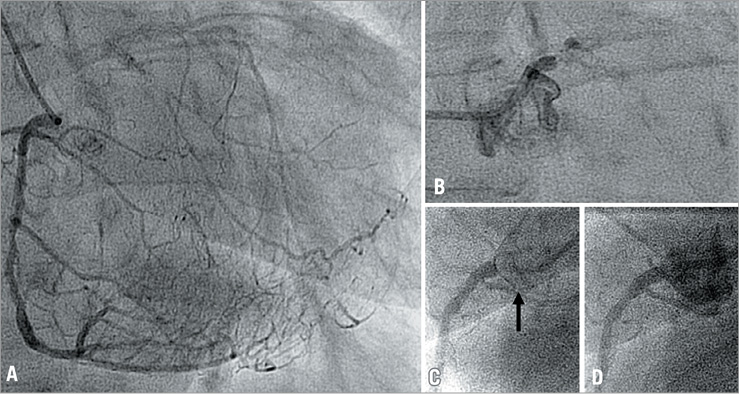
Figure 3. Example of patient with 3VD with high rSYNTAX score. An 89-year-old woman presented with NSTEMI, having had five acute coronary syndromes, including one episode of cardiogenic shock (managed medically), two transient cerebral ischaemic episodes and peripheral vascular disease. The baseline SYNTAX score (panels A, B, and C), with a chronically occluded LMS (B) and a high-grade stenosis of the ostial RCA (C), was 37. After treatment of just the RCA (D), the rSYNTAX score was 32.
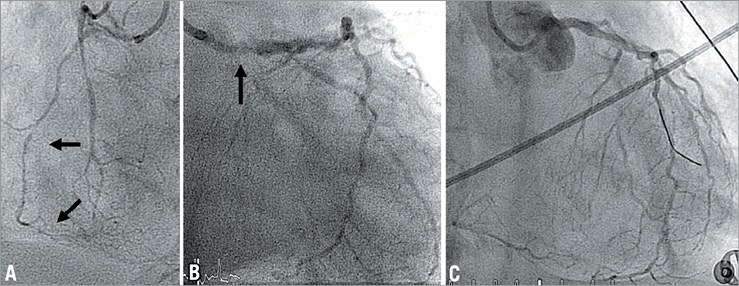
Figure 4. Example of a patient with 3VD with high rSYNTAX score. A 79-year-old woman being ventilated for pneumonia presented with gross ST-segment depression. The baseline SYNTAX score (panels A and B), with a chronic occlusion of the RCA and stenoses of the LMS, LAD and Cx, was 32. After treatment of just the ostial LMS (C), the rSYNTAX score was 21.
OUTCOMES
Mortality data were obtained from the UK Office for National Statistics and calculated at 30 days, one year and at most recent follow-up.
STATISTICS
All descriptive data were tested for conformity to a normal distribution with the Kolmogorov-Smirnov test. Data were expressed as mean (SD) with percentages for normally distributed parameters or median (interquartile ranges) for non-parametric parameters. Variables were compared with unpaired t-tests or Mann-Whitney rank sum tests, as appropriate. Bivariate correlation of parametric data was performed with Pearson’s correlation coefficient (rP). Categorical data were analysed using a chi-squared statistic (χ2) or Fisher’s exact test for 2x2 comparisons. The performance of SYNTAX, rSYNTAX and ΔSYNTAX for determining mortality was calculated by constructing receiver operator curves (ROC) and the c-statistic, calibration being assessed by the Hosmer-Lemeshow goodness of fit test. Survival curves were constructed using Cox proportional hazard statistics, with hazard ratios for death given with 95% confidence intervals where appropriate. Initially an unadjusted survival curve was constructed and baseline parameters were then introduced sequentially to the hazard model to control for baseline confounding. The influence of adding rSYNTAX and SYNTAX to this multivariable analysis was also explored. Further analysis on the impact of incomplete revascularisation was explored with tertile analysis of rSYNTAX upon survival, and the relationship of rSYNTAX to the number of vessels successfully treated by PCI. Binary logistic regression was used to explore the reasons for failing to achieve full revascularisation. The model included all major comorbidities, baseline characteristics and type of presentation. Statistical significance was sought at the 95% level. All analyses were performed with SPSS version 14.5 (SPSS Inc., Chicago, IL, USA).
Results
PATIENT AND LESION CHARACTERISTICS
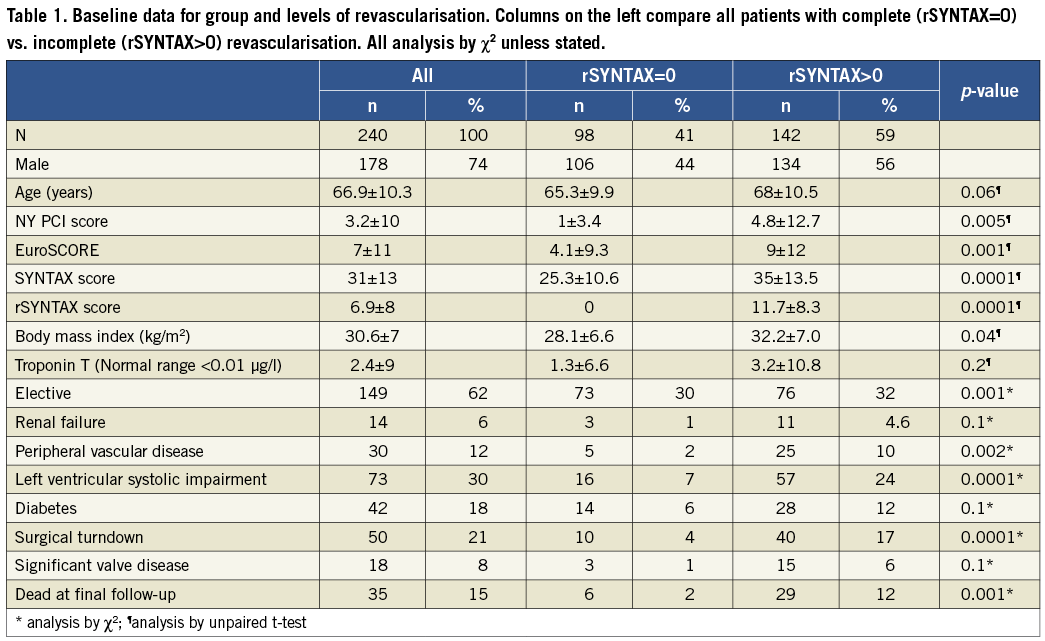
Two hundred and forty consecutive patients with 3VD undergoing PCI were entered into our registry between 2003 and 2008. Principal baseline data are presented in Table 1. The median EuroSCORE was 2.6 (1.5-7), New York PCI risk score 0.23 (0.12-0.81) and SYNTAX score 29 (22-38). Successful PCI to three vessels was performed in 135 patients, two vessels in 84 and one vessel in 21. The baseline SYNTAX score correlated positively with age (rP=0.3, p=0.001), and SYNTAX scores >32 were significantly associated with diabetes (52% vs. 30%), left ventricular impairment (58.9% vs. 30%), peripheral vascular disease (63% vs. 34%), surgical rejection (52% vs. 32.8%), and emergency presentation (71.4% vs. 28.6%); all p<0.01.
REASONS FOR INCOMPLETE REVASCULARISATION
The reasons for failing to achieve CR were technical failure (15%), planned decision not to attempt certain lesions (e.g., long chronic total occlusions or diffuse distal disease [21%]), operator opinion that further efforts were inappropriate during a procedure (e.g., high contrast load [25%]), and others (e.g., unexpected complications [39%]).
OUTCOMES
The overall mortality at 30 days was 5% (12/240), at one year 10% (26/240) and at final follow-up at 2.6 (1.7-3.8) years 14.5% (35/240). In multivariate analyses, the only parameters consistently associated with outcome were EuroSCORE, left ventricular impairment, acuity of presentation and age. These factors were used for all subsequent multivariate analyses and to assess the discrimination of SYNTAX, rSYNTAX and ΔSYNTAX.
EFFECT OF COMPLETE VS. INCOMPLETE REVASCULARISATION
Successful complete revascularisation (rSYNTAX=0) was achieved in 98 patients (40%). The distribution of baseline SYNTAX scores was parametric, whereas the distribution of rSYNTAX score was skewed towards low values (Figure 5). The median (IQR) rSYNTAX score was 3.5 (0-10.9). Of the 135 patients who had successful PCI to all three vessels, 65% attained rSYNTAX of 0 and 69% attained rSYNTAX below the median for the whole group (3.5). At final follow-up there was lower mortality in patients attaining rSYNTAX of 0 vs. others (2.5% vs. 12%, p=0.003), and in those attaining rSYNTAX < median vs. > median (3% vs. 11%, p=0.003). At 30 days, the mortality of the lowest, middle and highest tertiles of rSYNTAX were: 0%, 5% and, 10% and at one year: 2.5%, 12.5% and 22.5%, respectively (p<0.01; Figure 6). A summary of univariate and multivariate predictors of complete revascularisation and death is shown in Table 2. As a single variable, rSYNTAX was consistently associated with death in both univariate and multivariate analyses.
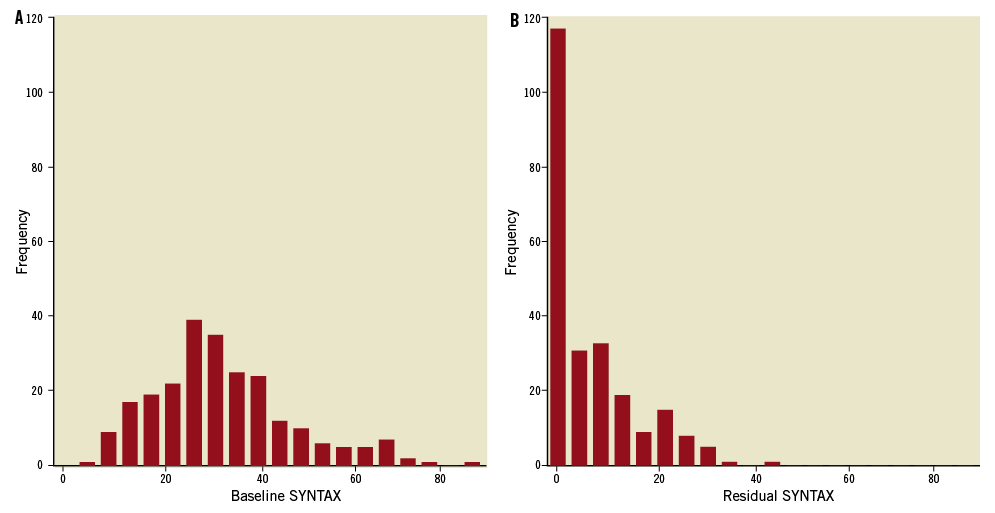
Figure 5. Histograms demonstrating the distribution of baseline SYNTAX (A) and rSYNTAX (B) scores.
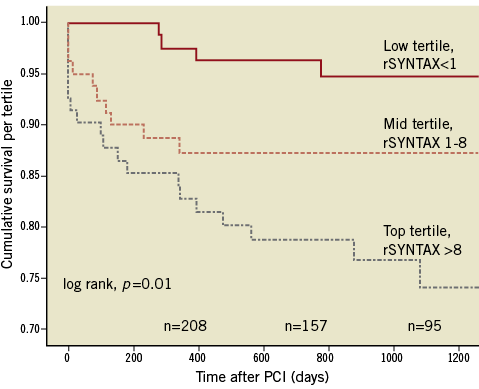
Figure 6. Actuarial survival according to tertile of rSYNTAX.
Numbers below the curve indicate patients at risk at yearly time points.
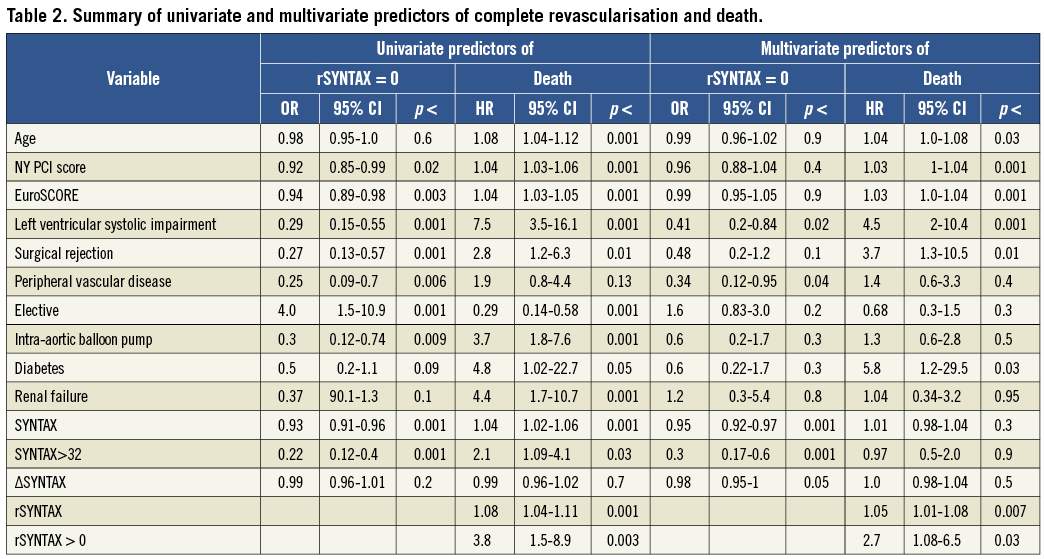
SYNTAX, RSYNTAX AND ΔSYNTAX AS PREDICTORS OF OUTCOME
All three scores were discriminators of outcome in univariate analyses. The c-statistics for discrimination of mortality were 0.66 for baseline SYNTAX, 0.71 for rSYNTAX and 0.52 for ΔSYNTAX (Figure 7). In multivariate analyses, only rSYNTAX was independently predictive of survival, and generated a highly discriminative model (c-statistic 0.92, calibration 0.61). Neither baseline SYNTAX score nor ΔSYNTAX was an independent predictor of survival after adjustment.
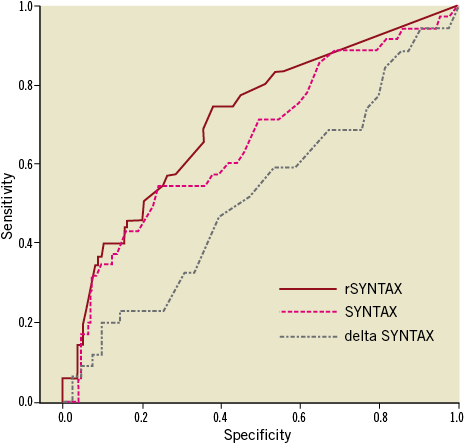
Figure 7. Receiver operator curves for discrimination of mortality (univariate analysis). The red line is rSYNTAX (c-statistic 0.71, calibration 0.94); the pink line baseline SYNTAX (c-statistic 0.66, calibration 0.56); and the grey line is ΔSYNTAX (c-statistic 0.52, calibration 0.78).
Discussion
In the present study, we have described a novel quantitative method of recording the completeness of revascularisation at PCI. Incomplete revascularisation, using the concept of rSYNTAX, was found to be associated with worse outcome than complete revascularisation. This finding is in accordance with other studies but, for the first time, this was accurately quantified, and its importance assessed, relative to the overall clinical picture. Until now, the level of revascularisation in clinical trials of PCI has been relatively poorly described. In the SYNTAX study, for example, complete revascularisation was achieved in 56.7% in the PCI arm, but the degree of incomplete revascularisation was not quantified. Other studies have generally reported the number of untreated or unsuccessfully treated vessels as an indicator of revascularisation. For example, 135 of our patients received successful PCI to three coronary vessels (135/240=56%) and might be deemed completely revascularised by standard criteria, yet only 40% achieved rSYNTAX of 0.
The present study found the purely angiographic SYNTAX score to be poorly predictive of survival. This finding is broadly in agreement with the literature, with most reports suggesting SYNTAX is moderately predictive of short-term and intermediate composite outcome23-27, although at least three studies did not find a relationship with SYNTAX score and mortality1,28,29. In contrast, clinical risk scores incorporating simple, but powerful, clinical characteristics, such as advanced age, acuity of presentation and the presence of haemodynamic instability, may have greater power to determine mortality than lesion-based scoring systems, even incorporating (as SYNTAX scoring does) a jeopardy “weight” according to the site of the lesion. The literature is consistent in reporting that incorporation of clinical data with baseline SYNTAX score substantially improves discrimination and prediction of survival30-35. The present data have shown the novel rSYNTAX score described here (but not, perhaps surprisingly, ΔSYNTAX) was associated with worse survival both with and without multivariable adjustment. We have shown that mortality after PCI is dependent, at least partly, upon the inability to revascularise completely. Furthermore, post hoc tertile analysis suggests increasingly adverse outcome with higher degrees of incomplete revascularisation. In this regard our data are also consistent with the literature. Intermediate follow-up of the SYNTAX study data reported incomplete revascularisation in 43.3% of PCI patients and increased composite outcome (although not mortality) in this group36. Two very recent studies have calculated residual SYNTAX scores in a similar fashion to the present data. The Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) investigators recently examined a cohort of NSTE-ACS patients (with predominantly low baseline SYNTAX) and reported residual SYNTAX scores to be an independent predictor of all-cause mortality at one year37. An analysis of an Italian unprotected left main PCI cohort examined the impact of baseline SYNTAX and residual SYNTAX and found parameters of discrimination almost identical with the present study38.
Residual SYNTAX scores have therefore been applied to three patient groups: a registry of patients with three-vessel disease (the present study), consecutive unprotected left main PCI patients38, and NSTE-ACS patients37. In each case residual SYNTAX was associated with all-cause mortality in multivariate analyses.
Limitations
The data in this paper are taken from a consecutive series from a single operator at a single centre, and may not be widely applicable. This may be reflected in the second criticism, which is that the one-year mortality of our patients was 13.5%, compared with the equivalent figures in the SYNTAX trial PCI arm (4.4%) and PCI registry (7.3%)1. However, the excess mortality in our series represents an unselected real world population incorporating emergencies and patients unsuitable for surgery with a higher EuroSCORE (7±11) than either SYNTAX PCI trial (3.8±2.6) or PCI registry patients (5.8±3.1). Another weakness is the lack of universal tests of ischaemia, mostly because many patients presented acutely. In addition, mortality was the only outcome assessed, because it was not possible to capture complete data for “softer” endpoints, such as repeat revascularisation, stroke, myocardial infarction, bleeding, and contrast nephropathy. Finally, because our analyses were retrospective, and rSYNTAX is an entirely novel concept, our conclusions should be regarded as hypothesis-generating rather than definitive.
Conclusions
We have developed a novel method of quantifying completeness of revascularisation, the rSYNTAX score. This score was an independent predictor of survival after PCI for unselected patients with three-vessel disease in multivariate analyses. Complete revascularisation seems to be a legitimate aim for patients with multivessel disease treated by PCI, whenever it can be safely achieved. Our findings develop the recent reports suggesting that prediction of the anticipated rSYNTAX score may be a more useful exercise than simply calculating the baseline SYNTAX score, at least in assessing the long-term mortality risk following PCI.
Conflict of interest statement
The authors have no conflicts of interest to declare.

