Abstract
Aims: The purpose of the study was to investigate whether the favourable outcomes of state-of-the-art PCI in the SYNTAX II trial, demonstrated at one year, were maintained at two-year follow-up.
Methods and results: The SYNTAX II study was a multicentre, single-arm study that investigated the impact of a contemporary PCI strategy on clinical outcomes in 454 patients with de novo three-vessel coronary artery disease, without left main disease. Clinical outcomes in SYNTAX II were compared to the predefined PCI (SYNTAX-I PCI) and coronary artery bypass graft (SYNTAX-I CABG) cohorts from the landmark SYNTAX trial (SYNTAX-I), selected on the basis of equipoise for long-term (four-year) mortality utilising the SYNTAX score II. At two years, major adverse cardiac and cerebrovascular events (MACCE: a composite of all-cause death, any stroke, myocardial infarction, or revascularisation) in SYNTAX II were significantly lower compared to SYNTAX-I PCI (13.2% vs. 21.9%, p=0.001). Furthermore, similar two-year outcomes for MACCE were evident between SYNTAX II PCI and SYNTAX-I CABG (13.2% vs. 15.1%, p=0.42).
Conclusions: At two years, clinical outcomes with the SYNTAX II strategy remained superior to the predefined SYNTAX-I PCI cohort, and similar to the predefined SYNTAX-I CABG cohort.
Introduction
With the introduction of drug-eluting stents (DES), the efficacy of percutaneous coronary intervention (PCI) has improved compared to bare metal stents1. Despite this, five-year follow-up of the landmark SYNTAX-I (SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery) trial demonstrated that PCI with first-generation DES was inferior to coronary artery bypass graft (CABG) surgery, being associated with a higher incidence of a composite of all-cause death, any stroke, or myocardial infarction (MI) (PCI 20.8% vs. CABG 16.7%, p=0.03)2.
In the de novo three-vessel disease (3VD) cohort of SYNTAX-I, patients with a low anatomical complexity (anatomic SYNTAX score ≤22) were shown to have similar outcomes between CABG and PCI at five years. Conversely, in patients with more anatomically complex coronary artery disease (anatomic SYNTAX score >22), CABG was demonstrated to have superior clinical outcomes. As a reflection of these findings, 3VD with low anatomic SYNTAX score (≤22) is now given a class Ia recommendation for PCI, with more complex coronary artery disease (>22) given a class III recommendation for PCI, and patients recommended to undergo CABG3. Furthermore, due to the results of a recent patient-level meta-analysis3,4, guidelines downgrade patients with 3VD with a low SYNTAX score and diabetes mellitus to a class IIb recommendation for PCI, and class Ia for CABG.
Since the completion of the SYNTAX-I trial, major technical and procedural advances influencing PCI outcomes have taken place. The SYNTAX II trial investigated the impact of a contemporary PCI strategy (SYNTAX II strategy) on clinical outcomes in patients with de novo 3VD, compared to a pre-specified and matched population of the SYNTAX-I trial, utilising the SYNTAX score II to identify patients with equipoise for long-term mortality between CABG and PCI.
At one year, the SYNTAX II strategy was superior to predefined SYNTAX-I PCI with respect to major adverse cardiac and cerebrovascular events (MACCE: a composite of all-cause death, any stroke, MI, or revascularisation, 10.6% vs. 17.4%, p=0.006). Furthermore, the non-inferiority of the SYNTAX II strategy compared to SYNTAX-I CABG was demonstrated, with respect to one-year MACCE (10.6% vs. 11.2%, p for non-inferiority <0.001)5. In terms of a composite of all-cause death, any stroke, or MI, the SYNTAX II strategy was similar to predefined SYNTAX-I CABG (4.0% vs. 5.9%, p=0.20). The long-term clinical outcomes of contemporary PCI remain to be proven.
The purpose of this paper was to investigate whether the favourable outcomes of state-of-the-art PCI in the SYNTAX II trial at one year were maintained at two-year follow-up.
Methods
STUDY DESIGN
The design for this trial has been described previously5,6. The clinical outcomes in SYNTAX II were compared with predefined PCI (SYNTAX-I PCI) and CABG (SYNTAX-I CABG) cohorts from SYNTAX-I. These patients were selected on the basis of equipoise for long-term four-year mortality between CABG and PCI utilising the SYNTAX score II.
Following the selection of patients utilising the SYNTAX score II, consensus of the Heart Team (cardiac surgeons and interventional cardiologists) – that equivalent anatomical revascularisation was achievable – was mandated. Only then was the patient eligible for recruitment in SYNTAX II. Coronary lesions agreed by the Heart Team as requiring revascularisation were identified as “target lesions”. Coronary lesions agreed by the Heart Team as not requiring revascularisation were identified as “non-target lesions”.
Target lesions for revascularisation in SYNTAX II were assessed with a hybrid instantaneous wave-free ratio (iFR)/fractional flow reserve (FFR) approach. Physiologically significant lesions were treated with the SYNERGY™ DES (Boston Scientific, Marlborough, MA, USA). Post-PCI intravascular ultrasound assessment was mandatory to optimise stent expansion and apposition, with a recommendation to use the modified MUSIC criteria7. In addition, contemporary chronic total occlusion revascularisation techniques8 by dedicated operators, and guideline-directed medical therapy, including antiplatelet therapy and high-intensity statin therapy3,9, were recommended. The patient’s clinical status was assessed at discharge, and at one- and two-year follow-up. Extended yearly follow-up is planned up to five years.
The local ethics committee approved the study in all participating sites. All patients provided written informed consent before enrolment.
ENDPOINTS
MACCE was defined as a composite of all-cause death, any stroke, MI, or revascularisation.
The primary analysis was two-year MACCE in the SYNTAX II compared with the SYNTAX-I PCI cohort. Spontaneous MI was defined as new Q-waves or one plasma level of creatine kinase myocardial band (CK-MB) 5x ULN (or troponin ≥35 ULN if CK-MB not available)10 in the context of clinical syndrome consistent with acute coronary syndrome11. Secondary endpoints included the individual components of MACCE and definite stent thrombosis (ST) according to Academic Research Consortium (ARC) definitions at two-year follow-up12.
By the SYNTAX II trial design, non-target vessel revascularisation (non-TVR) at follow-up was classified as:
1. occurring in a non-target lesion, anatomically assessed by visual inspection at the time of screening by the Heart Team and agreed as not for revascularisation;
2. occurring in a deferred coronary lesion based on iFR/FFR at the index procedure.
As an additional exploratory analysis, two-year MACCE was compared with the predefined SYNTAX-I CABG cohort of the original SYNTAX-I trial. Adverse events were adjudicated by an independent clinical events committee.
STATISTICAL ANALYSIS
The statistical analysis for this trial has been described previously5,6 and is summarised in Supplementary Appendix 1.
Results
BASELINE AND PROCEDURAL CHARACTERISTICS
Between February 2014 and November 2015, 454 patients out of 708 screened patients were enrolled in SYNTAX II13. In SYNTAX-I, 643 (58.8%) patients with 3VD without left main disease had an equipoise recommendation for CABG or PCI based on the SYNTAX score II and were used as the comparator. Baseline and procedural characteristics and achievement of SYNTAX II strategy are shown in Supplementary Table 1-Supplementary Table 3. In SYNTAX II, the distribution of the anatomic SYNTAX score was as follows: low (≤22) 298 patients (65.6%); intermediate (23–32) 140 patients (30.8%), high (>32) 16 patients (3.5%).
In SYNTAX II, statins were used in 97.3% and 92.3% of patients at discharge and two-year follow-up, respectively. Dual antiplatelet therapy use involved 6.8% of patients at two-year follow-up.
TWO-YEAR MACCE AND COMPONENTS
At two years in SYNTAX II, five patients withdrew their consent and six patients were lost to follow-up, resulting in complete two-year follow-up in 97.6% (n=434). Comparatively, in SYNTAX-I PCI, six patients were lost to follow-up, resulting in complete two-year follow-up in 98.0% (n=309); in SYNTAX-I CABG, 25 patients were lost to follow-up, resulting in complete two-year follow-up in 92.5% (n=309).
Table 1 and Figure 1 show MACCE and its components at two-year follow-up. The incidence of MACCE was significantly lower in SYNTAX II compared to SYNTAX-I PCI (13.2% vs. 21.9%; hazard ratio [HR] 0.57, 95% confidence interval [CI]: 0.40-0.81], p=0.001). This difference was driven by a reduction of 66% in any MI and 38% in any revascularisation. We found a trend towards lower incidences of all-cause death and stroke in SYNTAX II compared to SYNTAX-I PCI (2.7% vs. 5.5%, p=0.055, 0.4% vs. 2.0%, p=0.07, respectively).
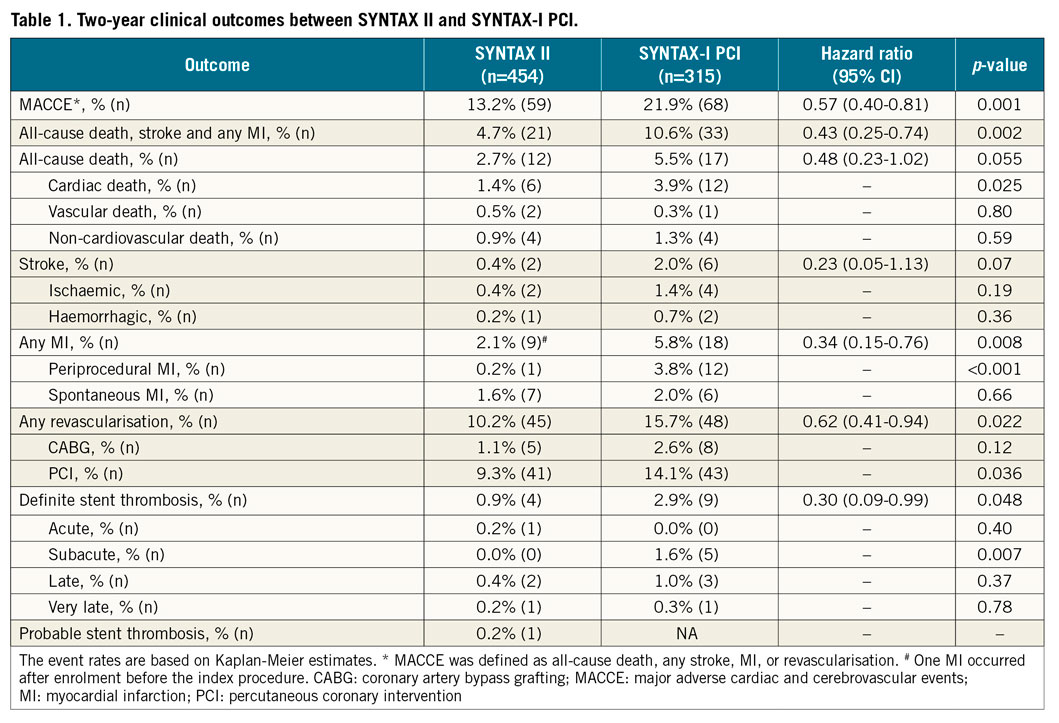
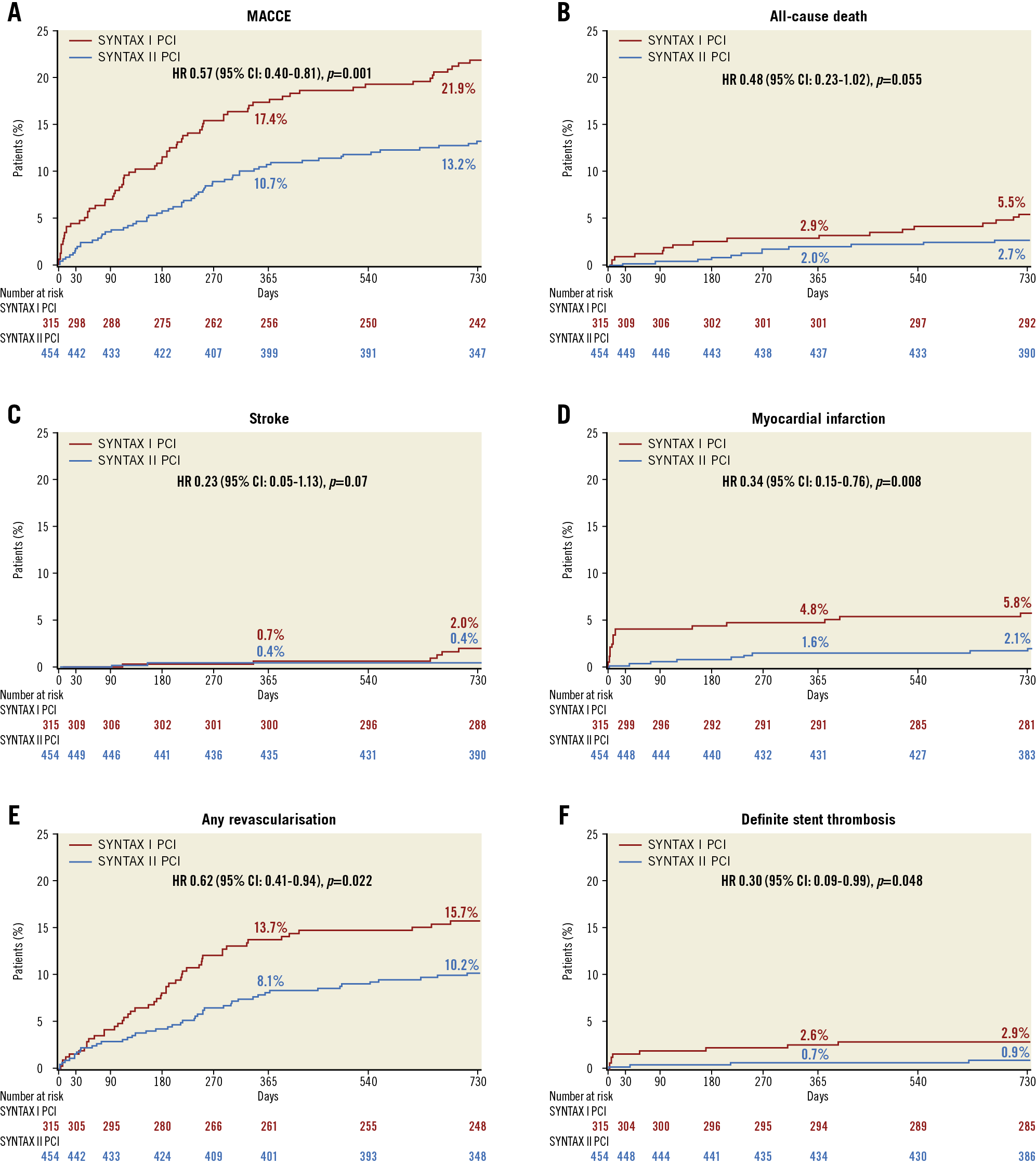
Figure 1. Two-year clinical outcomes among the study patients, compared with the SYNTAX-I PCI cohort. Kaplan-Meier curves are shown for SYNTAX II (blue) and SYNTAX-I PCI (red) for the composite endpoint of major adverse cardiac or cerebrovascular events (MACCE) (A), all-cause death (B), stroke (C), any myocardial infarction (D), any revascularisation (E), and definite stent thrombosis (F). MACCE was defined as all-cause death, any stroke, MI, or revascularisation.
There was no difference in MACCE between SYNTAX II patients with low (≤22) vs. intermediate or high (>22) anatomical SYNTAX score (12.3% vs. 15.0%, p=0.439) (Figure 2), patients with vs. without any diabetes mellitus (15.0% vs. 12.5%, p=0.50), or patients with diabetes mellitus treated with insulin vs. without insulin (18.4% vs. 13.4%, p=0.46) (Supplementary Figure 1, Supplementary Figure 2).
Figure 2. Kaplan-Meier cumulative incidence for major adverse cardiac or cerebrovascular events in SYNTAX II patients stratified by anatomic SYNTAX score ≤22 (blue) and >22 (red).
In multivariate analysis, chronic obstructive pulmonary disease (HR 2.90, 95% CI: 1.30-6.44), peripheral vascular disease (HR 3.38, 95% CI: 1.32-8.62), and anatomical SYNTAX score per unit of score (HR 1.05, 95% CI: 1.002-1.101) were significant (Supplementary Table 4).
REPEAT REVASCULARISATION BETWEEN ONE-YEAR AND TWO-YEAR FOLLOW-UP
The description of the revascularisation procedures in SYNTAX II is presented in Supplementary Table 5. Between one-year and two-year follow-up, 22 revascularisations occurred in 20 out of 1,559 lesions and two lesions were treated twice. Four lesions had already experienced a first event up to one year. The majority of revascularisations occurred in the initially stented lesions (77%, n=17 events), whereas there were few events in the initially deferred lesions (14%, n=3 events) (Figure 3). No MI in the territory of the initially deferred lesions occurred.
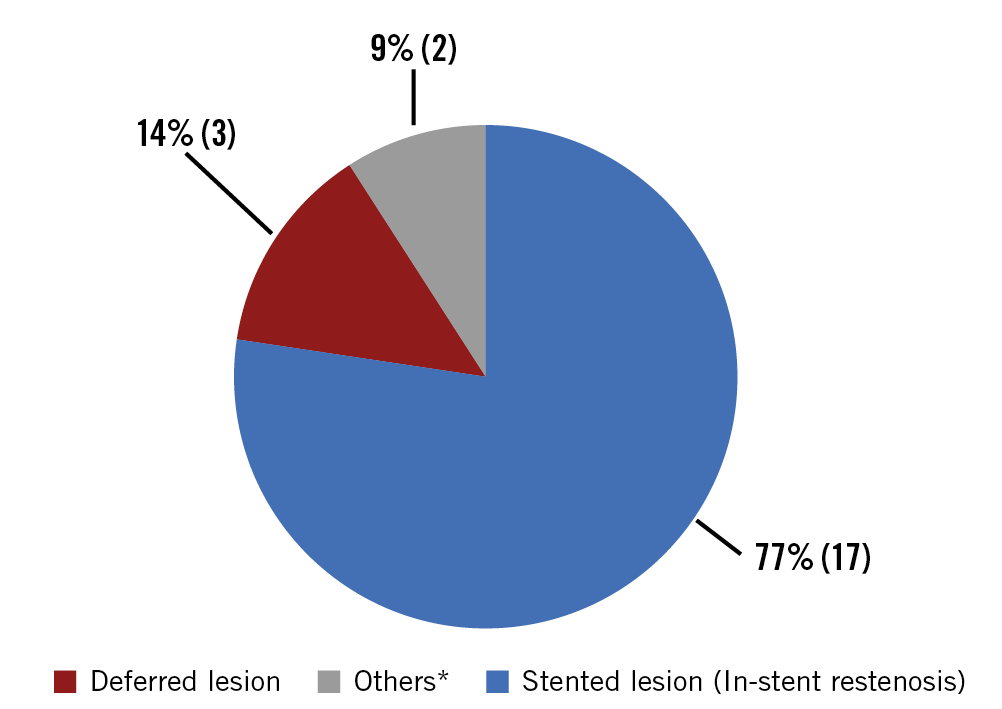
Figure 3. Distribution of baseline lesion type that caused revascularisation from one-year to two-year follow-up. In a total of 22 revascularisations, the majority of revascularisations occurred in the initially stented lesions (77%, n=17 events, blue), whereas there were few events in the initially deferred lesions (14%, n=3 events, red). *One revascularisation occurred in a distal lesion far from the initially stented lesion. In addition, one revascularisation of a CTO lesion was staged and not treated at the index procedure (9%, n=2 events, grey).
STENT THROMBOSIS
The incidence of definite ST in SYNTAX II was significantly lower compared to SYNTAX-I PCI (0.9% vs. 2.9%; HR 0.30, 95% CI: 0.09-0.99, p=0.048] (Table 1, Figure 1). No difference was found in the incidence of late (between 30 days and one year) and very late ST (after one year) between groups. Between one- and two-year follow-up, only one ST occurred as MI in SYNTAX II.
EXPLORATORY COMPARISON WITH SYNTAX-I CABG
The exploratory comparison with the predefined SYNTAX-I CABG demonstrated a similar` incidence of MACCE at two years (SYNTAX II 13.2% vs. SYNTAX-I CABG 15.1%; HR 0.85, 95% CI: 0.58-1.25, p=0.42) (Table 2, Figure 4). The incidence of stroke was significantly lower in SYNTAX II compared to SYNTAX-I CABG (0.4% vs. 2.2%, p=0.045). The incidence of all-cause revascularisation was similar (10.2% vs. 8.4%, p=0.41). We found a trend towards a higher incidence of non-TVR in SYNTAX II compared with SYNTAX-I CABG (2.0% [9/454] vs. 0.6% [2/334], p=0.12).
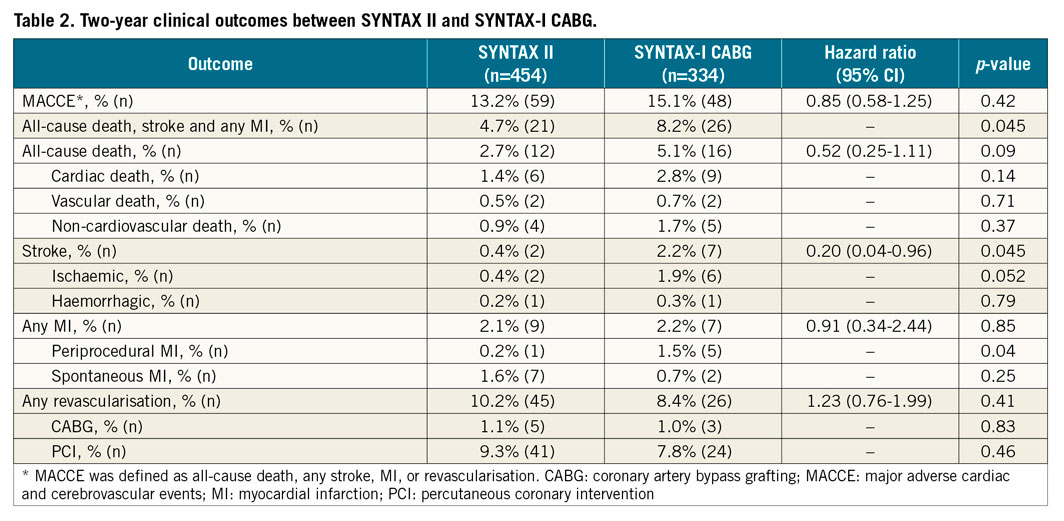
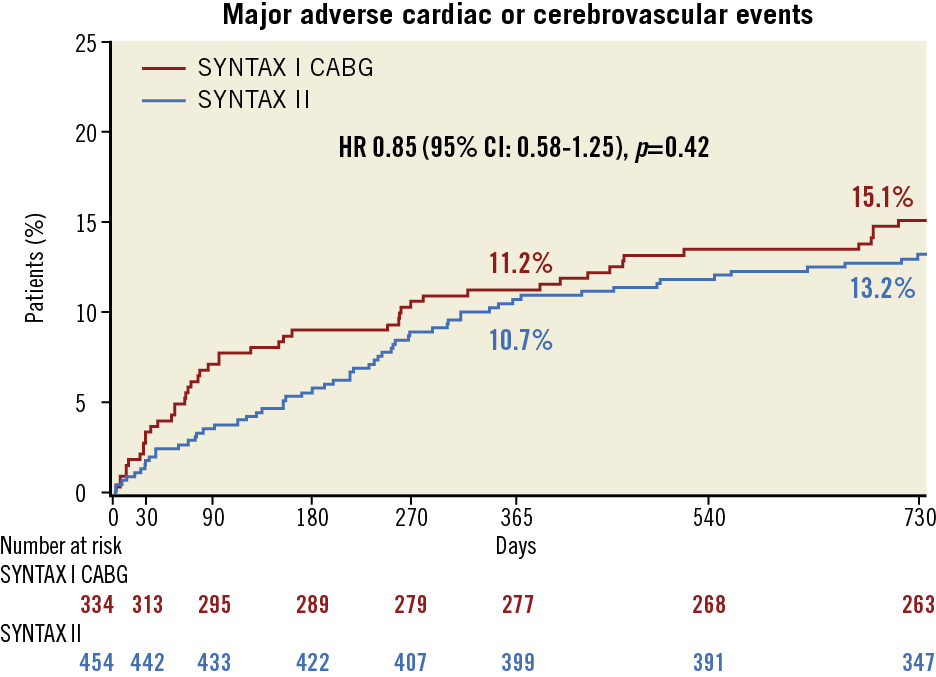
Figure 4. Two-year major adverse cardiac or cerebrovascular events among the study patients, compared with the SYNTAX-I CABG cohort. Kaplan-Meier curves are shown for SYNTAX II (blue) and SYNTAX-I CABG (red) for the exploratory composite endpoint of major adverse cardiac or cerebrovascular events (MACCE). MACCE was defined as all-cause death, any stroke, MI, or revascularisation.
Looking at the details of nine non-TVR in SYNTAX II, seven non-TVR occurred in initially deferred lesions based on iFR/FFR at the index procedure. One non-TVR occurred in an anatomically non-target lesion at the index procedure. The second patient developed unstable angina before a planned staged procedure at day 2.
At the time of revascularisation (day 544 and day 303, respectively), one lesion was justified with FFR of 0.76, and one lesion had become a total occlusion.
Discussion
The main findings of the study are the following: 1) PCI undertaken with the SYNTAX II strategy was associated with superior outcomes compared with the predefined SYNTAX-I PCI cohort, with a lower incidence of MACCE predominantly driven by a reduction in MI, all-cause revascularisation, and definite ST at two-year follow-up; 2) the two-year outcomes of patients with intermediate or high anatomical SYNTAX score (>22), treated with PCI using the SYNTAX score II risk stratification algorithm, were similar to those observed in patients with the low anatomical SYNTAX score (≤22); 3) the two-year outcome of deferred lesions on the basis of a hybrid iFR/FFR approach was benign; 4) in an exploratory analysis at two years, PCI with the SYNTAX II strategy was similar to the predefined SYNTAX-I CABG cohort, with respect to the incidence of MACCE.
Even if some of the elements of the SYNTAX II strategy were not fully applied (Supplementary Table 3), it is important for clinicians to realise that these results were not just the outcomes of contemporary PCI, but instead were only obtained by “best of PCI practice”, which includes adoption of the SYNTAX II strategy in a high proportion if not all 3VD cases.
As shown in the FAME trial, physiology-guided revascularisation in patients with multivessel disease resulted in a significant reduction of a composite of death or MI at two-year follow-up after the index procedure compared with angiography-guided revascularisation14. In the present study, the proportion of the initially deferred lesions revascularised between one-year and two-year follow-up was quite low (14%, 3/22 lesions). Notably, no MI in the territory of the initially deferred lesions occurred. While recent trial data have revealed excellent outcomes of revascularisation deferral based on either iFR or FFR in low- and intermediate-risk populations15, the findings in the SYNTAX II trial demonstrate that safe decision making can also be performed in the high-risk 3VD patients who have been selected on the basis of equipoise for long-term mortality between CABG and PCI utilising the SYNTAX score II. Furthermore, as the decision to perform or defer revascularisation was based on iFR in more than 75% of interrogated stenoses, the SYNTAX II study provides indirect support to the safety of resting pressure-derived indices to decide revascularisation in this complex patient subset.
In the exploratory comparison with the predefined SYNTAX-I CABG cohort, no significant differences were shown in the incidence of MACCE between groups. The similar outcomes were maintained from one-year to two-year follow-up. Comparatively, the BEST trial, in which second-generation everolimus-eluting stents were used to treat multivessel disease, demonstrated that CABG was associated with a lower incidence of MACCE at five years, driven by a reduction in the incidence of MI and repeat revascularisation16. In the present study, the incidence of MI and repeat revascularisation in the SYNTAX II group remained similar to the SYNTAX-I CABG cohort at two years.
In addition, the incidence of definite ST at two years in SYNTAX II (0.9%) was comparable with current all-comers trials with newer-generation DES (BIOSCIENCE: 0.8 to 1.1%, BIO-RESORT: 0.6 to 1.0%, DESSOLVE III: 0.6 to 1.0%)17,18,19, and was lower than in the ARTS II trial (2.0%)20.
The favourable outcomes of the SYNTAX II strategy are exemplified by the absence of convergence and crossing over of endpoints at two years (Figure 4) which was evident in ARTS I and II. The incidence of non-TVR in SYNTAX II was numerically higher compared to SYNTAX-I CABG (2.0% [9/454] vs. 0.6% [2/334], p=0.12). In SYNTAX II, the majority of non-TVR occurred in initially deferred lesions at the index procedure with negative iFR/FFR values (7/9, 77.8%). In addition, two patients (2/9, 22.2%) at follow-up were justified by either anatomical character (total occlusion) or reduced FFR.
Study limitations
Firstly, this is a single-arm study comparing a contemporary PCI strategy with an historical control group (SYNTAX-I). Secondly, because of the observed advantage of CABG in females and young patients in the landmark SYNTAX trial, the SYNTAX score II resulted in a low proportion of these subgroups of patients in the present study. Thirdly, there is a nine-year lapse of time between the enrolment periods of SYNTAX I and II; with recent improvements in surgical techniques and concomitant medication, it is possible that the clinical results of a randomised trial could be at variance with the results of this present observational study21,22. Fourthly, although the use of coronary physiology was mandatory in lesions intended to be treated, mild stenoses not included in the anatomic SYNTAX score (i.e., <50%) may potentially be associated with physiological significance and were not systematically assessed by iFR/FFR. Finally, these data cannot be extrapolated to patients with left main disease and to 3VD patients without SYNTAX score II equipoise.
Conclusions
At two years, the SYNTAX II strategy was associated with improved clinical outcomes compared with the PCI performed in patients with 3VD without left main disease matched by the SYNTAX score II from the original SYNTAX-I trial. At two years, clinical outcomes of the SYNTAX II strategy compared favourably with the SYNTAX-I CABG cohort. Later follow-up is warranted, in addition to a randomised trial (with five to 10 years of follow-up) which will be mandatory to shed light on the respective values of contemporary and future surgical or percutaneous revascularisation treatments.
|
Impact on daily practice This study offers an attractive option of a revascularisation strategy in predefined patients with de novo 3VD (SYNTAX score II inclusion) even if the patients have moderate to severe anatomical complexity (anatomic SYNTAX score >22). |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Funding
The SYNTAX II trial was an investigator-initiated study, sponsored by the European Cardiovascular Research Institute (ECRI, Rotterdam, the Netherlands) with unrestricted research grants from Volcano and Boston Scientific. The grant givers were not involved in the study design, data collection, data interpretation or writing of the manuscript.
Conflict of interest statement
P.W. Serruys reports being a consultant for Volcano and a member of the advisory board of Abbott Vascular. J. Piek reports being a consultant for Philips/Volcano and being a member of the advisory board of Abbott Vascular. J. Escaned reports being a consultant for Abbott, Philips/Volcano, and Boston Scientific. A. Banning reports receiving lecture fees from Abbott Vascular, Medtronic, and Boston Scientific, and grant support from Boston Scientific. Y. Onuma reports being a member of the advisory board of Abbott Vascular. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.