Abstract
Aims: Incomplete revascularisation is common after percutaneous coronary intervention (PCI). While the absolute amount of residual coronary artery disease (CAD) after PCI has been shown to be associated with worse outcomes, whether the proportion of treated CAD is prognostically important remains to be determined. We sought to quantify the proportion of CAD burden treated by PCI and to evaluate its impact on outcomes using a new prognostic instrument - the SYNTAX Revascularisation Index (SRI).
Methods and results: The baseline SYNTAX score (bSS) and residual SYNTAX score (rSS) were determined from 2,618 angiograms of patients enrolled in the prospective ACUITY trial. The SRI was then calculated for each patient using the following formula: SRI=(1–[rSS/bSS])×100. Outcomes were examined according to three SRI groups (SRI=100% [complete revascularisation], 50-99%, and <50%). The median bSS was nine (IQR 5, 16), and after PCI the median rSS was one (IQR 0, 6). The median SRI was 85% (IQR 50, 100), and was 100% in 1,079 patients (41.2%), 50-99% in 907 patients (34.6%), and <50% in 632 patients (24.1%). One-year adverse outcomes, including death, were inversely proportional to the SRI. An SRI cut-off of <80% (present in 1,189 [45.4%] patients after PCI) had the best prognostic accuracy for prediction of death (area under the curve 0.60, 95% confidence interval [CI]: 0.53-0.67, p<0.0001). By multivariable analysis, SRI was an independent predictor of one-year mortality (hazard ratio [HR] 2.17, 95% CI: 1.05-4.35, p=0.03). However, when compared to other scores, the rSS showed superior accuracy and predictive capability for one-year mortality.
Conclusions: The SRI is a newly described method for quantifying the proportion of CAD burden treated by PCI. Given its correlation with mortality, and pending external validation, the SRI may be useful in assessing the degree of revascularisation after PCI, with SRI ≥80% representing a reasonable goal. However, the rSS showed superior predictive capability for one-year mortality.
Introduction
Achievement of complete revascularisation is intuitively desirable in patients with coronary artery disease (CAD) undergoing percutaneous coronary intervention (PCI). However, despite major advances in PCI technology and technique, complete revascularisation is often not achieved (e.g., diffuse disease in small vessels, complex calcified lesions, chronic total occlusions), and whether it is always necessary is a matter of considerable debate1-5. Indeed, whereas incomplete revascularisation may be unavoidable and detrimental in patients with complex coronary artery disease5-7, in other cases (e.g., low CAD burden) the long-term prognosis may be reasonable with optimal medical therapy8. Among patients treated by PCI in the SYNTAX (SYNergy Between PCI With TAXUS and Cardiac Surgery) and ACUITY (Acute Catheterization and Urgent Intervention Triage StrategY) trials, approximately 40-60% achieved complete revascularisation1,2,9. Recently, we proposed a novel approach to characterise and quantify the completeness of revascularisation better –the residual SYNTAX score (rSS)1. This score has subsequently been validated by other groups and been shown to have good prognostic accuracy for adverse ischaemic outcomes after PCI2,10-12. Undetermined, however, is whether a threshold level exists for a reasonable degree of incomplete revascularisation. In the current report, we propose a novel index, the SYNTAX Revascularisation Index (SRI), which takes into account the severity and extent of baseline CAD (as assessed by the baseline SYNTAX score [bSS]) and the residual CAD after PCI (as assessed by the rSS) in determining the proportion of CAD that has been treated. We sought to determine the prognostic utility of the SRI among patients undergoing PCI from the large, prospective, randomised ACUITY trial.
Methods
STUDY PROTOCOL
The ACUITY trial design has previously been described in detail13. Briefly, ACUITY was a multicentre, prospective, randomised trial in which 13,819 patients were enrolled with moderate and high-risk non-ST-segment elevation acute coronary syndromes (NSTE-ACS) undergoing an early invasive strategy. Prior to coronary angiography, patients were randomly assigned to heparin (unfractionated or low-molecular-weight) plus a glycoprotein IIb/IIIa inhibitor, bivalirudin plus a glycoprotein IIb/IIIa inhibitor, or bivalirudin monotherapy. Angiography was performed within 72 hours of randomisation, after which patients were triaged to PCI, coronary artery bypass graft (CABG) surgery, or medical therapy. For patients who underwent PCI, stent type (bare metal or drug-eluting) was per operator discretion. Dual antiplatelet therapy with aspirin and clopidogrel was recommended for at least one year. An independent clinical events committee, blinded to treatment assignment, adjudicated all major adverse events. The institutional review board/ethics committee at each participating centre approved the study, and all patients provided written informed consent.
OBJECTIVES, PATIENT POPULATION, AND ANGIOGRAPHIC ANALYSIS
Our primary objective was to quantify the disease burden treated by PCI using the SRI and to evaluate its impact on adverse ischaemic outcomes, including all-cause death, cardiac death, myocardial infarction (MI), and unplanned repeat revascularisation for ischaemia. The present study was limited to patients undergoing PCI in whom quantitative coronary angiography was performed as part of a formal substudy by experienced core laboratory technicians blinded to randomisation and clinical outcomes (Cardiovascular Research Foundation, New York, NY, USA)14,15. Patients with prior CABG were excluded as the SYNTAX score (SS) had not been validated in this cohort at the time of analysis16.
SYNTAX REVASCULARISATION INDEX
For the present study, three experienced interventional cardiologists (PG, TP, and AC) blinded to randomisation and clinical outcomes assessed the bSS17,18 and rSS1 for each angiogram (www.SYNTAXscore.org). The Fleiss κstatistic19 (tertile partitioning), determined from 50 independently read films, was 0.57 for bSS signifying a moderate level of interobserver agreement20. The SRI, representing the proportion of CAD burden treated by PCI, was calculated using the following formula: SRI=(1–[rSS/bSS])×100. Patients were stratified into three groups and compared: SRI=100% (complete revascularisation), 50-99%, and <50%. Adverse ischaemic outcomes between groups were compared at one year.
ENDPOINT DEFINITIONS AND STATISTICAL ANALYSIS
Composite major adverse cardiovascular events (MACE) were defined as death from any cause, MI, or unplanned revascularisation for ischaemia. Definitions of the components of the MACE endpoint have been previously detailed15. All MACE endpoints were adjudicated by an independent committee blinded to randomisation.
Continuous data are presented as mean±SD or median (interquartile range; IQR) and were compared using the ANOVA or Kruskal-Wallis test as appropriate. Categorical variables were compared using the χ2 test. Correlation (Spearman) between rSS and SRI was examined. Comparisons of one-year outcomes were performed (Kaplan-Meier curves) with the log-rank test between the three groups of SRI. Major subgroup analyses were examined for potential interaction. Receiver operating characteristic (ROC) curves for SRI were determined to assess the relative predictive accuracy for one-year all-cause mortality. Area under the curve for the SRI was computed to identify the Youden index (best cut-off) for one-year all-cause death. Differences in discrimination power between scores were evaluated using the χ2 test. Stepwise Cox multivariable regression analysis was performed to ascertain variables independently associated with one-year mortality, with variable entry/stay criteria of 0.1/0.1. In addition to the SRI, variables historically known to be associated with these adverse events were included in the models, with the number carefully chosen to avoid overfitting1. The following variables were included in the model: SRI, age, insulin-treated diabetes, renal insufficiency, baseline white blood cell count, and baseline cardiac biomarker elevation or ST-segment deviation. A p-value <0.05 was considered statistically significant for all analyses. Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA).
Results
PATIENT AND BASELINE CHARACTERISTICS
Of 6,921 patients included in the angiographic substudy of ACUITY, 3,826 underwent PCI. After excluding patients with a history of CABG (n=862) and those in whom the bSS or rSS could not be calculated due to technical reasons (n=346), 2,618 patients remained, comprising the current study population. No significant differences in baseline characteristics or one-year adverse outcomes were observed between the 346 excluded patients and the study cohort (data not shown). The SYNTAX score ranged from one to 59, with a median of nine (IQR 5, 16). After PCI, the median of rSS was one (IQR 0, 6) ranging from zero to 47.5. The calculated SRI thus ranged from 0% to 100%, with a median of 85% (IQR 50, 100). The SRI was 100% in 1,079 patients (41.2%), 50-99% in 907 patients (34.6%), and <50% in 632 patients (24.1%).
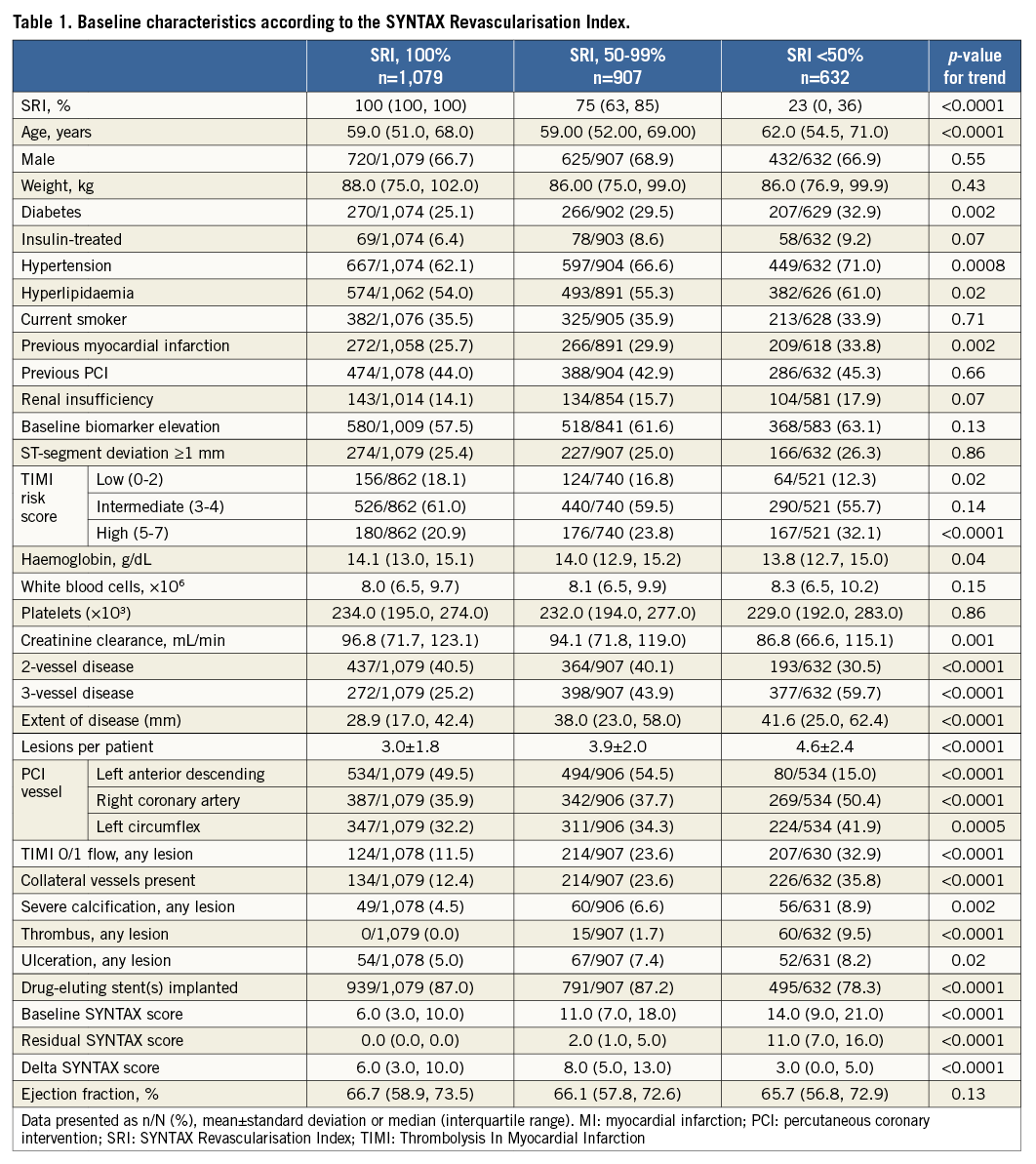
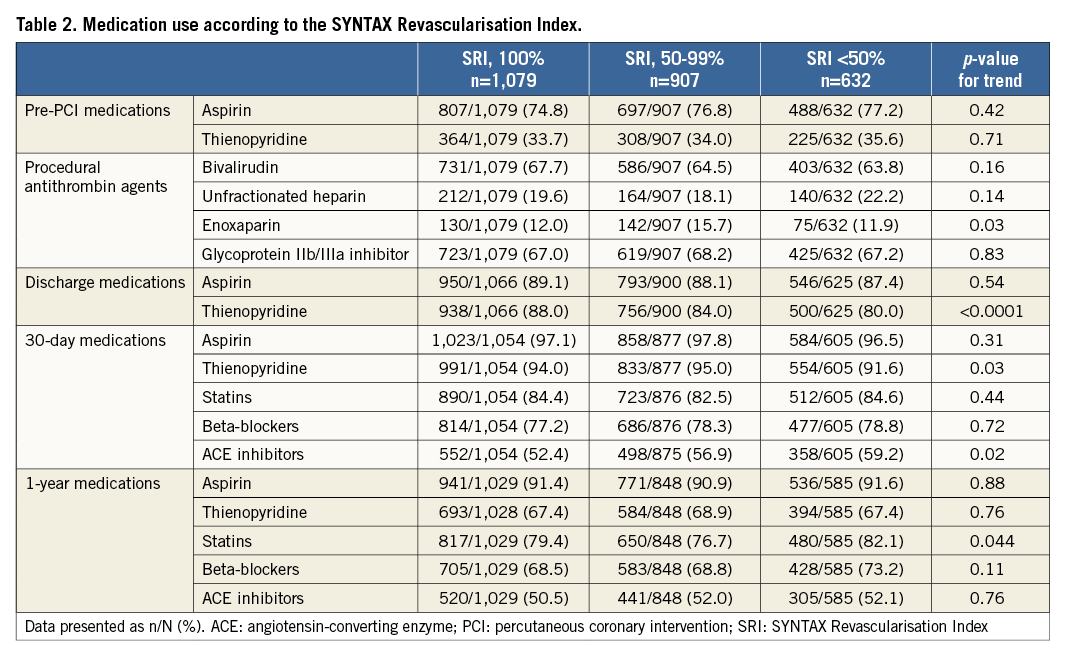
Table 1 and Table 2 present clinical characteristics and angiographic findings, stratified by SRI. Patients with lower SRI were older and had a higher prevalence of diabetes, hyperlipidaemia, and hypertension. They were also more likely to have a history of prior MI and reduced baseline haemoglobin levels and creatinine clearance. Angiographically, patients with lower SRI were more likely to have multivessel disease, a greater number of lesions, and more extensive disease. They were also more likely to have baseline TIMI 0/1 flow, collaterals, and lesions with severe calcification or thrombus. Thienopyridines were less frequently used in the patients in the lowest SRI group at discharge and at 30-day follow-up, but not at one year.
The correlations between rSS and SRI are shown in Figure 1. There was a moderate significant negative correlation between rSS and SRI.
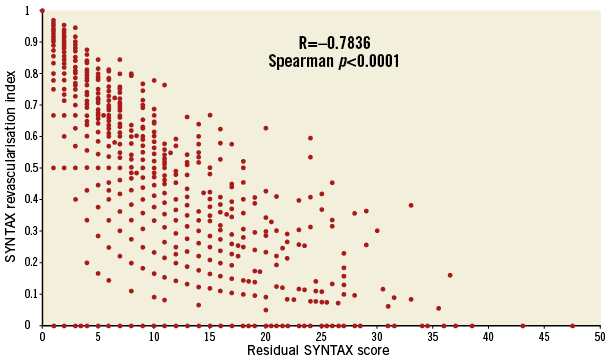
Figure 1. Correlation between the residual SYNTAX score and the SYNTAX Revascularisation Index. Scatter plot graph showing a significant moderate negative correlation between rSS and SRI (lower rSS is associated with higher SRI). One dot represents more than one patient. rSS: residual SYNTAX score; SRI: SYNTAX Revascularisation Index.
CLINICAL OUTCOMES
The one-year rates of MACE were inversely correlated with SRI, with the lowest MACE rates in the group with complete revascularisation and the highest MACE rate in the group with SRI <50%. Similar findings were seen for death, cardiac death, and MI, with non-significant trends for higher rates of unplanned revascularisation and definite/probable stent thrombosis in patients with the greatest degree of incomplete revascularisation (Table 3, Figure 2). By multivariable analysis, lower SRI was a strong independent predictor of one-year mortality (along with insulin-treated diabetes and advanced age) (Table 4).
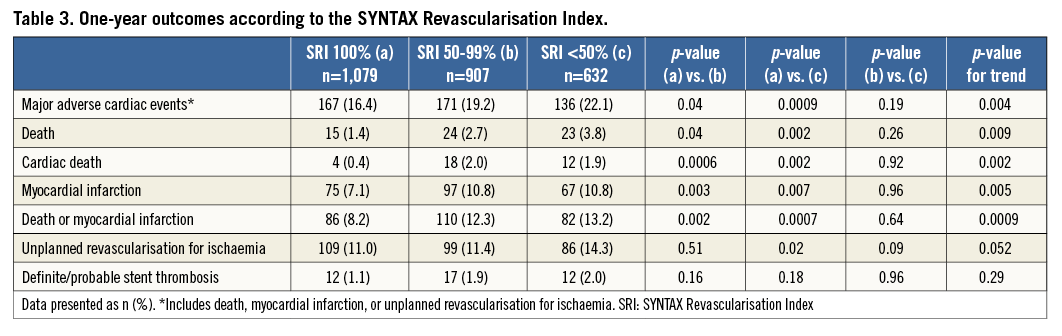
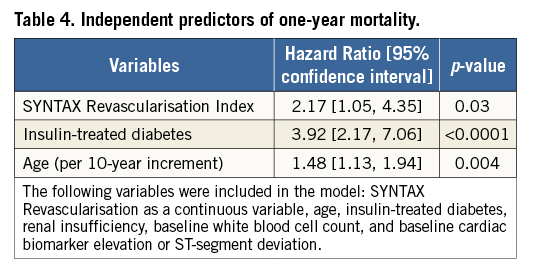
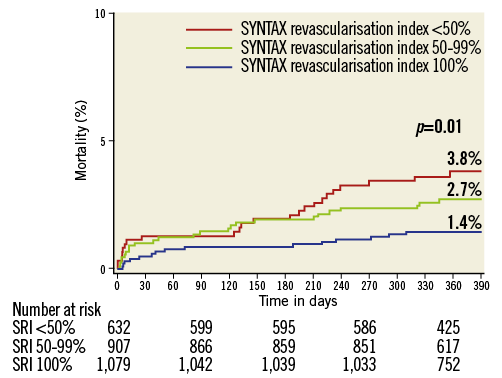
Figure 2. Kaplan-Meier curves showing cumulative mortality rates through one year. The rate of death significantly increased with less complete revascularisation as assessed by SRI.
ROC CURVE ANALYSIS
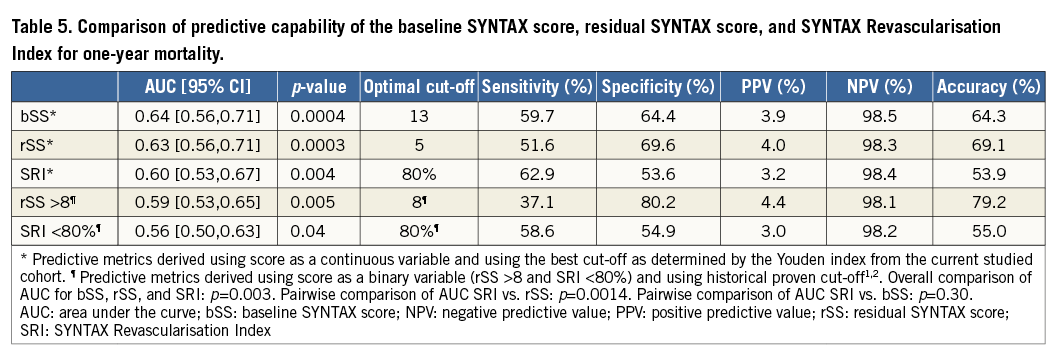
ROC curve analysis demonstrated a significant association between the SRI and one-year all-cause mortality. An SRI cut-off of 80% had the best prognostic accuracy for risk prediction of death (area under the curve [AUC] 0.60, 95% CI: 0.53-0.67, p<0.0001). When compared with the bSS and the rSS, the SRI demonstrated a slightly better sensitivity compared to the bSS and rSS (Table 5); however, the rSS, especially an rSS >8, demonstrated the best specificity and accuracy for one-year mortality when compared to other scores.
SUBGROUP ANALYSIS
The impact of SRI <80% was consistent in all subgroups examined except for sex (p-value for interaction=0.03) (Figure 3). SRI had a significant impact on one-year mortality in men, but not in women.
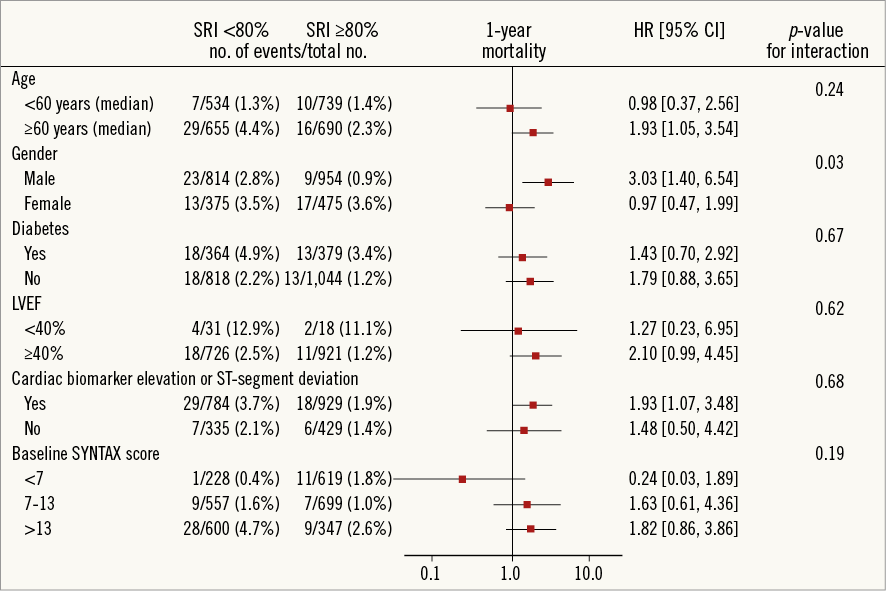
Figure 3. Major subgroup analysis and the impact of the SYNTAX Revascularisation Index on one-year mortality. The detrimental impact of incomplete revascularisation (SRI <80%) was consistent in all subgroups examined except for sex.
Discussion
The present report describes a new prognostic tool, the SRI, which may be used to quantitate the effectiveness of a revascularisation procedure in “removing” the angiographic burden of CAD. As such, the SRI may be useful to examine the extent of incomplete revascularisation which may be considered reasonable. The SRI was developed and studied in a cohort of 2,618 patients with moderate and high-risk NSTE-ACS who underwent PCI. The principal findings of the present study are as follows. (1) The SRI was associated with one-year adverse ischaemic outcomes, with mortality, MI, and MACE being inversely correlated with SRI. (2) The SRI was a strong and independent predictor of one-year mortality. (3) In this regard, achievement of an SRI ≥80% may be considered a reasonable goal for PCI. (4) However, among our low-risk population, the rSS had better predictive capability for one-year mortality when compared to SRI.
Achieving complete revascularisation is not always possible, and whether it is necessary for favourable outcomes is still a matter of debate. Using a different definition of incomplete revascularisation, ~40% of PCI patients in the SYNTAX trial had incomplete revascularisation, underlining the difficulty of achieving complete revascularisation with PCI in some patients with extensive CAD2,5,21. As such, the construct of “reasonably incomplete revascularisation” has been proposed22-24. However, the extent of jeopardised myocardium which must be treated by PCI to improve prognosis has never been examined. It is well accepted that the amount of myocardium at risk at baseline and the complexity and extent of CAD are directly correlated with the occurrence of adverse events after revascularisation17,25,26. Several studies have now shown that the amount of residual CAD after revascularisation is prognostically important, with an rSS >8 after PCI being associated with worse outcomes1,2,9,10. While achieving an rSS <8 after PCI might thus be seen as a reasonable goal, for patients with extensive CAD (e.g., bSS >32), characterisation of the proportion of CAD treated (SRI) may be more appropriate and informative when considering revascularisation options and for procedural planning.
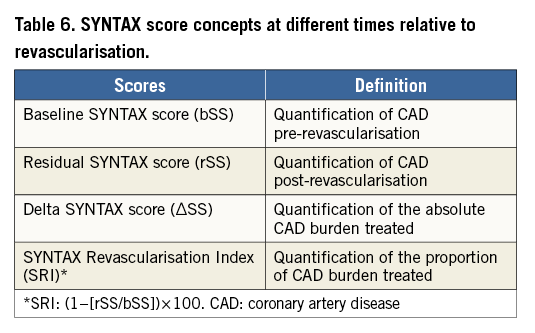
The SRI represents a novel and complementary tool developed to characterise better the proportion of CAD treated by PCI and to describe the completeness of revascularisation better. Given its strong association with mortality, an SRI ≥80% could be seen as a reasonable goal when achieving incomplete revascularisation after PCI among patients presenting with NSTE-ACS and relatively low-risk CAD. However, the rSS, characterising the absolute amount of residual CAD after PCI, remains the most specific and accurate score for prediction of one-year mortality. That being said, the bSS, rSS and SRI have different meanings and roles during the patient assessment and clinical decision-making process, and therefore each may have utility in practice and during clinical trials (Table 6). The bSS is an important prognostic tool to assess patient outcomes prior to revascularisation and helps discriminate between the choice of PCI and CABG for individual patients. Alternatively, the rSS and the SRI not only have post-procedural prognostic utility, but can also serve as a guide for clinical decision making, depending on the expected degree of revascularisation. Unless at least a reasonable and appropriate27 level of revascularisation can be achieved, CABG may be a better alternative to PCI.
It is important to emphasise that, while an SRI of ≥80% might be used as a benchmark for “reasonably incomplete” revascularisation, the ACUITY trial represents a population with angiographically low-risk CAD (median bSS of nine). External validation of the SRI concept in a population of patients involving more complex CAD would be interesting, especially to determine the stability of its predictability among different levels of CAD complexity (as previously demonstrated by an rSS <8)2. The extent of incomplete revascularisation (SRI) in SYNTAX is not known, and would be useful both to validate the concepts presented in the present report, and to examine the extent to which more complete revascularisation after PCI might have narrowed the differences observed between PCI and CABG in that trial. That being said, the impact of incomplete revascularisation on mortality has been shown to be significantly lower with CABG when compared to PCI21,27,28, and using a different method to quantify the incompleteness of revascularisation will probably not result in different findings.
Limitations
Despite being conducted in a large cohort of patients from a randomised controlled trial with detailed angiographic core laboratory analysis, several limitations should be acknowledged. First, the ACUITY trial enrolled patients with NSTE-ACS. Whether achieving an SRI ≥80% in an external population of patients with NSTE-ACS or stable CAD has similar prognostic implications remains to be proven. Second, the baseline anatomic complexity in the ACUITY trial was low (median bSS of nine); whether the SRI cut-off of 80% is optimal in a more complex CAD population (e.g., SYNTAX trial cohort) is unknown. Third, the SYNTAX score (bSS, rSS and SRI) is based on identifying lesions with diameter stenosis ≥50% in vessels ≥1.5 mm in diameter. Using a different threshold for vessel diameter (e.g., 2 mm) and lesion severity (e.g., diameter stenosis ≥70%) would lead to different results9, although whether the prognostic accuracy would be greater is unknown. Fourth, assessment of the SYNTAX score is well known to have high variability, an issue that could be overcome by appropriate training20 or by consensus of several readers29. While the three readers involved in the current study were appropriately trained and achieved an excellent level of agreement before initiating the SYNTAX score evaluation20, each SYNTAX score was not performed by consensus of the three readers, but rather by a single reader. Given that the rSS, the delta SS, and the SRI are all derived from the bSS, different results might have been obtained if carried out by consensus29. Fifth, CABG patients were not included in our analysis, and the results of the present analysis do not apply to this group. Sixth, the relatively short follow-up (one year), the modest number of deaths (n=62), and the retrospective nature of this study preclude definitive conclusions. The findings from this study are hypothesis-generating, and await external validation from other databases. In this regard, the subgroup interaction implying that SRI may be of greater utility in men as compared to women deserves further study. Finally, the SYNTAX score concept (bSS, rSS and SRI) is based on coronary anatomy complexity only, and recent studies have demonstrated the value of an ischaemic-oriented revascularisation30 or a combination of both (angiographic and ischaemic)31. Future studies are necessary to determine whether greater prognostic accuracy can be achieved by assessing the degree of functional or ischaemic revascularisation. The ongoing ISCHEMIA (NCT01471522), EXCEL (NCT01205776) and COMPLETE (NCT01740479) trials are prospectively examining this issue in different patient populations.
Conclusion
In conclusion, derived from a population of NSTE-ACS with low complexity of CAD at baseline, the SRI is a newly described method for quantifying the proportion of CAD burden successfully treated by PCI. Pending external validation, the SRI may be useful in anticipating or assessing the degree of revascularisation in patients with CAD, with SRI ≥80% a reasonable goal. Nonetheless, the rSS remains the best metric for completeness of revascularisation, showing the best predictive capability and accuracy for one-year mortality.
| Impact on daily practice Complete revascularisation after percutaneous coronary intervention is often not achieved, especially in patients with complex multivessel coronary artery disease. Derived from the baseline and residual SYNTAX scores, the current report proposes a new index, the SYNTAX Revascularisation Index (SRI), which provides insight into what might constitute a reasonable level of complete revascularisation. The SRI, paired with the two previously developed scores, offers the full quantitative language necessary to characterise the baseline, residual, and treated burden of coronary disease appropriately at any stage of revascularisation. Anticipating the SRI after PCI may be useful for clinical decision making, when choosing between revascularisation modalities. |
Guest Editor
This paper was guest edited by Antonio Colombo, MD, San Raffaele Scientific Institute, Milan, Italy.
Conflict of interest statement
P. Généreux has received speaker fees from Abbott Vascular and Cardiovascular Systems Inc., and is a consultant for Cardiovascular Systems Inc. T. Palmerini and A. Caixeta have received speaker fees from Abbott Vascular. M. Leon is on the scientific advisory board for Medtronic, Boston Scientific Corporation and Abbott Vascular. G. Dangas and R. Mehran have received institutional research grant support from The Medicines Company, Bristol-Myers Squibb/Sanofi, Eli Lilly and Company/Daiichi-Sankyo, Regado Biosciences, and STENTYS, consulting fees from Abbott Vascular, AstraZeneca, Boston Scientific, Covidien, CSL Behring, Janssen Pharmaceuticals, Maya Medical, and Merck & Co, and are on the advisory board for Covidien, Janssen Pharmaceuticals, Merck, and Sanofi. The other authors have no conflicts of interest to report. The Guest Editor has no conflicts of interest to declare.