Abstract
Aims: Three-vessel and left main coronary artery disease (CAD) have important prognostic implications. Consequently, numerous risk scores have been developed to stratify patients with complex CAD. The aim of the present study was to compare the predictive performance of six risk scores for occurrence of four-year all-cause mortality.
Methods and results: From March 2008 to December 2012, 348 consecutive patients with complex CAD undergoing percutaneous coronary intervention (PCI) in a tertiary centre in São Paulo, Brazil, were analysed. Four-year mortality was assessed. The scores compared were: baseline SYNTAX score (SS), residual SYNTAX score (rSS), ACEF score, clinical SYNTAX score (cSS), SYNTAX revascularisation index (SRI) and SYNTAX score II (SSII). SSII had the best predictive performance, AUC 0.82, Brier score 0.10, surpassing all the other scores for long-term mortality prediction. Moreover, SSII discriminated well PCI patients in risk groups with p<0.01 for four-year all-cause mortality. The ACEF score (AUC 0.77) and the cSS (AUC 0.78) were significantly better than the SS (AUC 0.65), SRI (AUC 0.60) or the rSS (AUC 0.55).
Conclusions: For patients with complex CAD treated by PCI, the combination of baseline clinical and angiographic factors provided better risk assessment. The SSII demonstrated the most precise predictive performance for long-term mortality.
Abbreviations
ARTS I: Arterial Revascularization Therapies Study Part I
AUC: area under the curve
CABG: coronary artery bypass graft
CAD: coronary artery disease
CI: confidence interval
COPD: chronic obstructive pulmonary disease
CrCl: creatinine clearance
cSS: clinical SYNTAX score
IQR: interquartile range
LVEF: left ventricular ejection fraction
NRI: Net Reclassification Index
PCI: percutaneous coronary intervention
PVD: peripheral vascular disease
rSS: residual SYNTAX score
SRI: SYNTAX revascularisation index
SS: SYNTAX score
SSII: SYNTAX score II
ULMCA: unprotected left main coronary artery
Introduction
Left main and three-vessel coronary artery disease (CAD) have been established as markers of poor prognosis1,2. The large amount of myocardium at risk with a higher probability of events classified these conditions as complex CAD3,4. Consequently, a number of risk scores have been developed in order to scrutinise complex CAD and decide the best therapeutic option.
With regard to percutaneous coronary intervention (PCI), the severity of baseline CAD, clinical characteristics and the post-revascularisation residual atherosclerotic burden have been shown to be independently related with long-term mortality and are considered in the risk stratification of coronary atherosclerosis4-8. For quantification of the atherosclerotic burden, the SYNTAX score (SS) is a combination of the total jeopardised myocardium and anatomical complexity9. Among the clinical characteristics, it is worth mentioning that the combination of age, creatinine clearance and ejection fraction is the backbone of risk models in cardiology7,10. Moreover, the residual SYNTAX score (rSS) and the SYNTAX revascularisation index (SRI) quantify CAD post revascularisation and the proportion of CAD burden treated6,11.
Therefore, in decision making for complex CAD, the initial anatomical complexity, whether to attempt complete revascularisation or to follow a reasonable incomplete revascularisation strategy, and also clinical and demographic variables should be considered. However, the impact of each risk model on long-term prognosis in isolation has not been compared and described. The objective of the present study was to test and compare SYNTAX-derived risk models that use clinical variables, baseline and post-PCI atherosclerotic burden for four-year all-cause death in a real-world population of complex CAD.
Methods
STUDY POPULATION
The present study is a registry which enrolled consecutive, real-world patients with complex CAD treated by PCI at the Albert Einstein Hospital, São Paulo, Brazil, from March 2008 to December 2012. Patients with previous coronary artery bypass graft surgery (CABG), ST-segment elevation myocardial infarction, and single or double vessel coronary artery disease were excluded from the study. Among 1,460 patients enrolled in the registry, 589 participants had three-vessel and/or unprotected left main CAD (complex CAD). Of these, 241 met the aforementioned exclusion criteria, and 348 were included in the current analysis.
The data collection was performed in a dedicated electronic database. The follow-up was made by phone or email at 30 days, six months, and annually until five years after PCI. The local ethics committee approved the research protocol, and informed consent was obtained from all patients.
DEFINITIONS
The creatinine clearance (CrCl), a measure of estimated glomerular filtration rate, was calculated using the Cockcroft-Gault equation12. Chronic obstructive pulmonary disease (COPD) was defined as the long-term use of bronchodilators or steroids for lung disease (EuroSCORE definition)13. Peripheral vascular disease (PVD) was defined as aorta and arteries other than coronaries, with exercise-related claudication, or revascularisation surgery, or reduced or absent pulsation, or angiographic stenosis of more than 50%, or combinations of these characteristics (Arterial Revascularization Therapies Study Part I [ARTS I] definition)14. Preprocedural left ventricular ejection fraction (LVEF) was taken by transthoracic echocardiography or diagnostic left ventriculography.
RISK MODELS
The present study compared the predictive performance on long-term all-cause mortality of the following risk scores.
– SYNTAX score: for the present study, experienced interventional cardiologists blinded to clinical outcomes assessed the SS for each angiogram (www.syntaxscore.com).
– ACEF score (age, creatinine, ejection fraction) score15: the modified ACEF score (ACEFCrCl) was calculated retrospectively using the formula age/ejection fraction+1 point for every 10 mL/min reduction in CrCl below 60 mL/min per 1.73 m2 (up to a maximum of six points)16.
– Clinical SYNTAX score (cSS): the cSS was calculated retrospectively for each patient using the formula cSS=(SYNTAX score) × (modified ACEF score).
– SYNTAX score II7: this is composed of the combination of two angiographic (SS and three-vessel/left main CAD) and six clinical elements: age, gender, creatinine clearance, COPD, peripheral artery disease and LVEF. Using the actual baseline clinical and angiographic data from every screened patient in the trial, SSII (PCI model) was calculated for each patient using an electronic calculator as previously described17.
– Residual SYNTAX score11: the rSS was defined as the SS recalculated after PCI.
– SYNTAX revascularisation index18: the SRI was calculated as: 100×(1–[rSS/baseline SS]).
STATISTICAL ANALYSIS
Categorical variables are presented as numbers and percentages. Continuous variables are expressed as mean±SD or median with interquartile range (IQR) based on their distributions. To obtain four-year mortality predictions based on the risk scores, Cox logistic regression analysis was used with each score as a sole linear predictor. The performance of the risk scores was evaluated using four metrics: c-statistics, Brier score, calibration plots, and Kaplan-Meier analyses. Discrimination was studied with the c-statistics and by Kaplan-Meier analyses with focus on a four-year time horizon19. The Brier score is a proper score function that measures the accuracy of probabilistic predictions20. The Brier score is a quadratic scoring rule, where the squared differences between actual binary outcomes “Y” and predictions “p” are calculated: Y*(1–p)2+(1–Y)*p2. Therefore, the lower the Brier score, the more precise is the risk model. As not all persons had follow-up completed until four years, our reclassification was based on the expected number of case and control patients calculated by using the Kaplan-Meier estimator21. All statistical analyses were performed using SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
The present study included 348 patients with complex CAD treated by PCI. Patients’ baseline characteristics are listed in Table 1. The median age was 68.8 years (IQR 60-77), 79.3% were male, 39.7% had diabetes, and the median LVEF was 57% (IQR 49.1-64.2%). The median SYNTAX score was 30 (IQR 22.0-39.0). After four years of follow-up, the rate of all-cause death in the studied population was 17.8%.
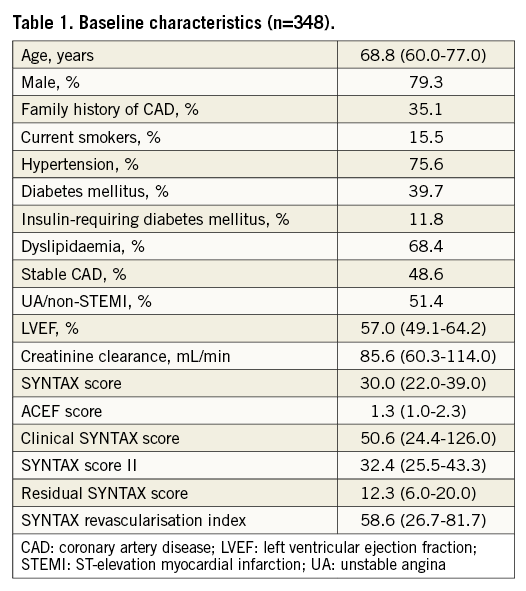
PREDICTIVE PERFORMANCE OF RISK SCORE MODELS: DISCRIMINATION
The discriminative performance of the risk scores is shown in Table 2. The SSII had the best predictive accuracy for four-year all-cause mortality (c-statistics 0.82; 95% confidence interval [CI]: 0.76-0.88). The cSS and the ACEF performed well with no significant difference between these two models (c-statistics 0.78; 95% CI: 0.71-0.83, and c-statistics 0.77; 95% CI: 0.71-0.84, respectively). The performance of purely anatomical characteristics (both baseline and residual) had significantly lower predictive accuracy. Additionally, the SS, ACEF, cSS, and SSII were able to separate low-, medium-, and high-risk tertiles (p<0.01 for all) (Figure 1), while the rSS and SRI were not.
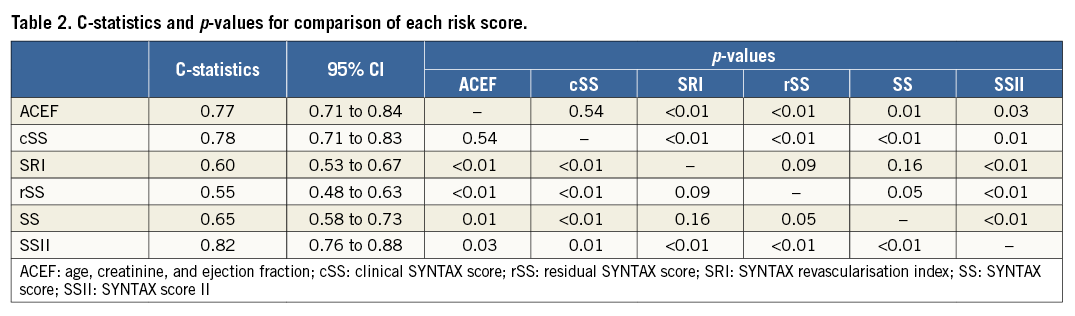
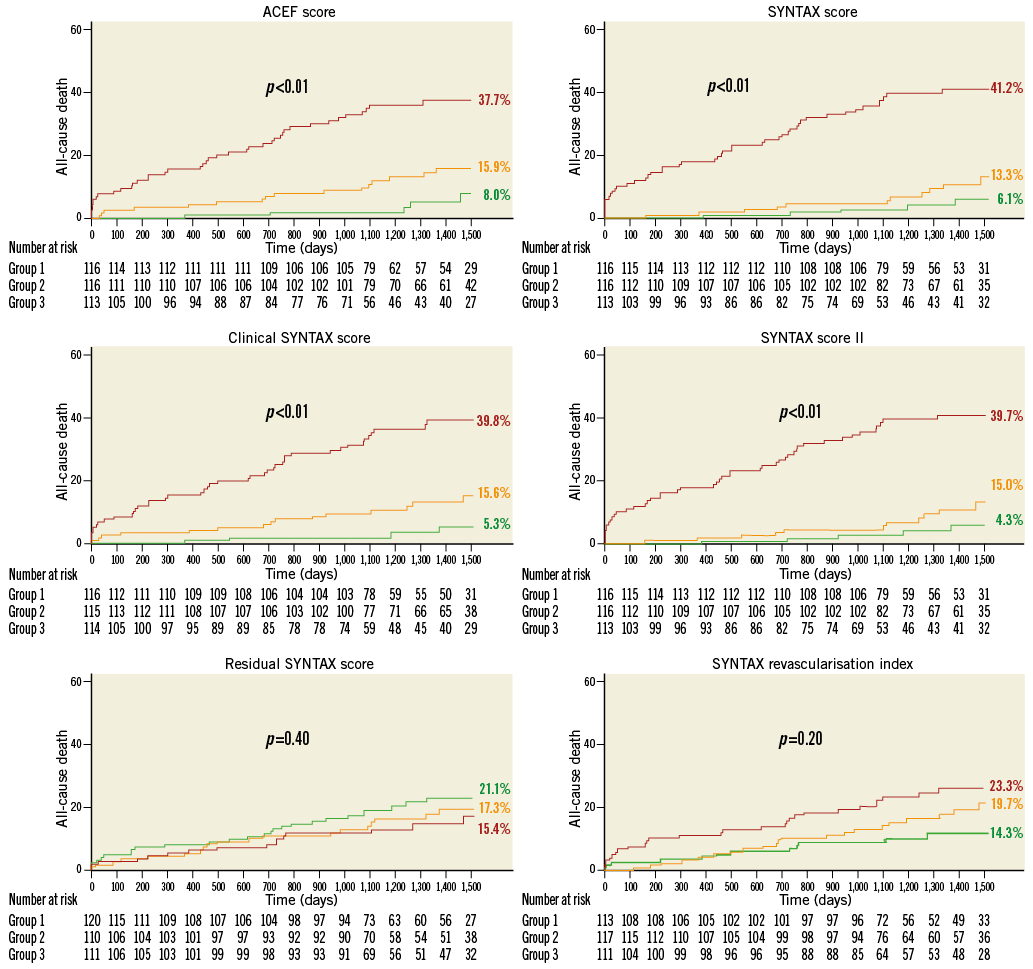
Figure 1. Kaplan-Meier curves of four-year all-cause mortality according to each risk score discrimination by terciles (p-values obtained from log-rank test). The colours of the survival curves are shown according to each score tertiles values in points: high=red; intermediate=orange; low=green.
CALIBRATION
The score with the smallest difference between the predicted and the observed four-year all-cause mortality was the SSII. Figure 2 illustrates the calibration of the scores tested in the present analysis.
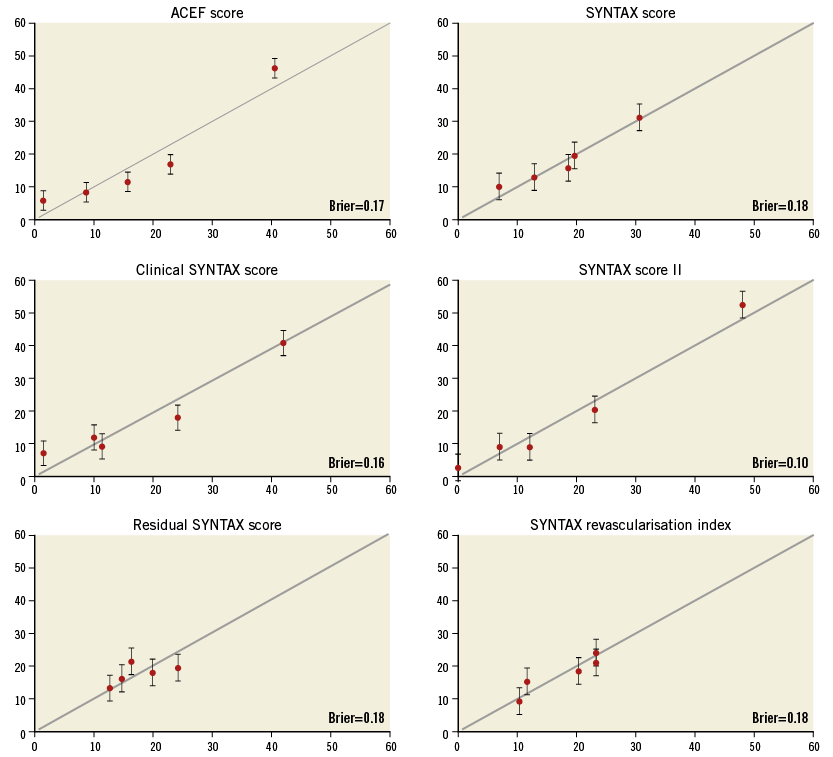
Figure 2. Calibration plot risk scores for observed and predicted mortalities. The circles demonstrate the Kaplan-Meier estimates of four-year mortality (vertical axis) by quintiles and the predicted four-year risk (horizontal axis).
Discussion
The findings of the present study can be summarised as follows: (1) the scores with baseline characteristics (both clinical and anatomical) had better performance than the assessment of complete revascularisation scores; (2) the combination of baseline clinical and anatomical characteristics improved the prediction of long-term all-cause mortality; (3) the SSII had the best overall accuracy for risk stratification of complex CAD.
The SYNTAX trial4,22 left a number of legacies for risk assessment and decision making in the treatment of complex CAD since it was an all-comers randomised trial of PCI versus CABG. The SYNTAX-based scores tell a good part of the story of the contemporary risk assessment of complex CAD. Most of these risk scores are herewith tested and compared in a “real-world” population.
The anatomical SS was developed as a tool to force the Heart Team to analyse the coronary angiogram systematically and assess the risk for anatomical revascularisation by CABG and PCI. It was first reported to be useful for decision making between CABG and PCI in the SYNTAX trial in 200922. The anatomical SS was then implemented in multiple medical guidelines and tested in numerous populations23,24. The SS had the limitation of classifying patients into categories or terciles. The expanding use of PCI has consequently increased the importance of developing a systematic approach for risk stratifying complex patients so that they might not be restricted by terciles or arbitrary cut-offs. Doctors should have individual risk estimation for an adequate dialogue with the patient and a meaningful comparison of performance between hospitals and operators16. The cSS was then developed to provide an individualised assessment of risk.
Despite major advances in PCI technology and technique, complete revascularisation is often not achieved in multivessel CAD due to technical or clinical reasons. The prognostic impact of incomplete revascularisation after PCI was inconsistent between studies because they lacked standardised definitions. The residual SS was then developed to quantify the amount of atherosclerotic burden and disease complexity that was not treated by PCI6,11. However, it is a matter of considerable debate whether complete revascularisation is always necessary. A novel index was then proposed, namely the SYNTAX revascularisation index (SRI). The SRI considers the relationship between the baseline CAD and the residual CAD after PCI, determining the proportion of CAD that has been treated11,18. For complex CAD, an rSS <8 and an SRI >70% were the best cut-off to show reduction in mortality6,8.
Another advance in terms of risk scores obtained from the SYNTAX trial was the SYNTAX score II. The SYNTAX score II (SSII) was built with the ACEF as its backbone, with the addition of risk factors that were shown to affect decision making between CABG and PCI directly7. The SSII estimates the individual four-year mortality for both revascularisations. As it provides an objective risk prediction for CABG and PCI, the SSII could be implemented in the Heart Team decision-making process between CABG and PCI17.
Last but not least, the extended model of the logistic clinical SYNTAX score has to be mentioned. It uses logistic regression analyses to explore the independent association of death with a relevant set of prognostic predictors. The logistic clinical SYNTAX score was not tested in the current work because it was originally developed for one- and three-year mortality10,25 and we used a four-year time horizon.
There were numerous reasons why all-cause death was chosen as the main outcome of the present study. It is important to mention that all-cause death is a hard, reproducible endpoint, not subject to adjudication bias or definitional variation. As was well summarised by Stephen S. Gottlieb, “Dead is dead—artificial definitions are no substitute”26. These characteristics make death a very good outcome measure in registries. Also, we would like to mention that all the scores we tested have been shown to be independent predictors of long-term mortality6,8,27-29. Therefore, all-cause death is an excellent metric to compare the performance of these scores.
The present work demonstrated using four metrics that the SSII had the most robust predictive performance. The c-statistic was 0.82 which indicates an accurate predictive score for long-term all-cause death. The SSII was able to classify patients better into low-, intermediate- and high-risk groups (Figure 1). The precision of the predictions of the SSII can also be seen in Figure 2. In a good score, the predicted risk matches the observed risk. Also, a better discriminating model has more spread between quintiles of predicted risk than a poorly discriminating model. The improved statistical performance was not obtained through additional computational complexity. Only one angiographic (left main or three-vessel disease) and three clinical (gender, PVD, COPD) variables were added to the cSS7.
The aforementioned findings reinforce the consistency of the SSII as an adjuvant tool in daily clinical practice, helping in the precise, critical and individual assessment of patients undergoing PCI17. The main limitation of the SSII is the relatively small number of external validation studies23,27,30-32. Our work validates the SSII in a Brazilian population, known to have profound miscegenation and genomic heterogeneity33.
Besides the comparison of these risk scores, it was not clear what was the best means of assessing the risk of a patient with complex CAD for long-term prognosis: the baseline clinical profile in isolation, the baseline anatomy, the combination of anatomy and clinical characteristics or the residual atherosclerotic burden. The present study quantifies with four metrics the benefits of each risk model. We showed that the combination of baseline clinical and angiographic factors provided the best score on this matter. Interestingly, both rSS and SRI did not perform well. Previously, these scores have been shown to be independent predictors of mortality6,8,18. Actually, in the study of Capodanno et al, the rSS had better performance than the SS. This discrepancy may have been affected by the presence or not of ischaemia in the unrevascularised territories34.
Limitations
The present study has the inherent limitations of a single-centre retrospective analysis. The ultimate goal of the SYNTAX score II is to assist the Heart Team in the decision-making process between CABG and PCI. Thus, a prospective study would be needed to achieve a true validation of the SYNTAX score II, where the decision between CABG and PCI is randomised30. We did not have detailed data of a CABG group to propose a validation of the SSII also in a group treated by surgery.
Conclusions
In patients with complex CAD treated by PCI, the combination of baseline clinical and angiographic factors provided better risk assessment than either factor alone or post-PCI atherosclerotic burden. The SSII provided the most precise predictive performance for long-term mortality.
| Impact on daily practice Numerous risk scores have been developed to assess the long-term risk of patients with complex CAD. The present work provided a detailed comparison of each component (baseline angiography, clinical factors, residual atherosclerotic burden) of SYNTAX-derived risk scores. The SSII substantially enhances the prediction of four-year mortality after PCI compared with the other scores, and allows an accurate personalised assessment of patient risk. |
Conflict of interest statement
The authors have no conflicts of interest to declare.