Abstract
Background: The SYNTAX score (SXscore) has been shown to be an effective predictor of clinical outcomes in patients undergoing percutaneous coronary intervention (PCI).
Methods and results: The SXscore was prospectively collected in 1,397 of the 1,707 patients enrolled in the “all-comers” LEADERS trial (patients post-surgical revascularisation were excluded). Post hoc analysis was performed by stratifying clinical outcomes at two-year follow-up, according to one of three SXscore tertiles: SXlow ≤8 (n=464), 8
Conclusions: The SXscore when applied to an “all-comers” patient population allows for prospective risk stratification of patients undergoing PCI up to two years follow-up. In addition, the SXscore appears to separate the performance of devices in high risk patient groups.
Introduction
The SYNTAX score (SXscore) is a comprehensive angiographic scoring system derived from the coronary anatomy and lesion characteristics1-3, which was initially designed to quantify coronary lesion complexity. Additional analyses have subsequently demonstrated its ability to predict major adverse cardiac events (MACE) following percutaneous coronary intervention (PCI) in patients with multivessel coronary artery disease at follow-up ranging from one to five years4-6. At one-year follow-up in the ARTS-II study, patients with a SXscore in the highest tertile had a significantly higher rate of MACE compared with patients in the lower tertiles (HR 3.5; CI 1.7-7.4; p=0.0001), while a multivariate analysis demonstrated that the SXscore independently predicted a fourfold increase in the risk of MACE. Furthermore, the SX score also showed a better discrimination ability than the AHA/ACC modified lesion classification (c-statistic 0.67 vs. 0.58; p<0.001).
The SXscore has not only been assessed in patients with complex coronary artery disease4-6 and left main disease7-8, but it has also been demonstrated to be a predictor of periprocedural myocardial infarction (MI) amongst patients undergoing elective PCI for long lesions and bifurcation lesions7. Most recently our group has evaluated its value for risk assessment in the setting of a randomised trial with an “all-comers”population. In the substudy of the LEADERS trial (Limus Eluted from A Durable versus ERodable Stent coating), where the SXscore was collected prospectively in 1,397 “all-comer” patients, we reported its prognostic value for MACE events at one-year follow-up8. In the current substudy we assess the value of the SXscore at two-year follow-up and also assess its ability to discriminate between the performance of two stainless steel drug-eluting stents, one eluting biolimus from a biodegradable polymer and one sirolimus from a durable polymer, in the highest risk patient group.
Methods
Study population
LEADERS was a multicentre European non-inferiority trial that compared the safety and efficacy of the BioMatrix™ Flex biolimus-eluting stent (BES) (Biosensors, Morges, Switzerland) to the Cypher® sirolimus-eluting stent (SES) (Cordis, Warren, NJ, USA) in 1,707 “all-comers” patients. Patients over the age of 18 with chronic stable coronary artery disease or acute coronary syndromes including ST-elevation myocardial infarction were eligible if they had at least one lesion with ≥50% diameter stenosis and reference vessel diameter 2.25 to 3.5 mm. The aim was for the patient population to reflect real world clinical practice and thus no limits were set on the number or complexity of the lesions stented. The only exclusion criteria were: known allergy to acetylsalicylic acid, clopidogrel, heparin, stainless steel, sirolimus, biolimus or contrast material that cannot be pre-medicated; planned surgery within six months of percutaneous coronary intervention unless the dual antiplatelet therapy could be maintained throughout the perisurgical period; pregnancy; participation in another trial before reaching the primary endpoint; and lastly, inability to give informed consent. The study complied with the Declaration of Helsinki and was approved by all institutional ethics committees. All patients provided written, informed consent for participation in the trial.
SYNTAX SCORE and angiographic analysis
From the baseline diagnostic angiogram, each coronary lesion producing ≥50% diameter stenosis in vessels ≥1.5 mm was scored separately and added together to provide the overall SXscore, which was calculated prospectively using the SXscore algorithm that is described in full elsewhere1-3. All angiographic variables
pertinent to SXscore calculation were computed by independent core laboratory analysts (Cardialysis B.V., Rotterdam, The Netherlands).
The initial description of the SXscore did not report a methodology for calculating the SXscore in patients presenting with an ST-elevation MI or those with in-stent restenosis lesions. Nevertheless, in the present study core lab analysts were blinded to all clinical data and therefore patients presenting with an ST-elevation MI had their occluded infarct-related artery scored as an occlusion of unknown duration in the same manner as any chronically occluded artery; amethodology that has subsequently been confirmed as the most appropriate method of SXscoring these patients9. No validation of calculating the SXscore has been performed in patients with in-stent restenotic lesions, and they were therefore scored in the same manner as if the lesion was a de novo lesion.
Limitations
The methods employed for scoring in-stent restenosed arteries has not been validated, and does not take into account some of the potentially different lesion characteristics of an acutely occluded artery or a restenosed lesion compared to a de novo lesion. However, these methods do allow the weighted score of the anatomical segment to be recorded, and do allow some of the lesion characteristics to be scored (e.g., lesion length, tortuosity, calcification, etc.).
Randomisation and procedures
Randomisation was done centrally after diagnostic cardiac catheterisation and before percutaneous coronary intervention (PCI) by use of a telephone allocation service (Limburgia Telefonische Antwoord Service BV, Rotterdam, The Netherlands). The allocation sequence was computer-generated, stratified according to centre, and blocked with block sizes of 8 and 16, which varied randomly. Patients were randomly allocated on a 1:1 basis to treatment with BES or SES, and to active angiographic follow-up at nine months or clinical follow-up only on a 1:3 basis with a factorial design.
BES were available in diameters of 2.25, 2.5, 3.0 and 3.5 mm and in lengths of 8, 11, 14, 18, 24 and 28 mm. SES were available in diameters of 2.25, 2.5, 2.75, 3.0 and 3.5 mm and in lengths of 8, 13, 18, 23, 28 and 33 mm. Balloon angioplasty and stent implantation were performed according to standard technique and direct stenting was allowed. No mixture of drug-eluting stents was permitted within a given patient, unless the operator was unable to insert the study stent, in which case crossover to another device of the operator’s choice was possible. Before or at the time of the procedure, patients were given at least 75 mg of acetylsalicylic acid, 300-600mg loading dose of clopidogrel, and unfractionated heparin at a dose at least 5,000 I or 70-100 IU/kg. After the procedure, all patients were advised to take aspirin indefinitely and clopidogrel for at least 12 months. In case of inter-current revascularisation procedures requiring stent implantation, treating cardiologists were encouraged to use the study stent. For other details please refer to the primary endpoint manuscript10.
Follow-up
Adverse events were assessed in the hospital and at 1, 6, 9, 12 and 24 months. One in four patients was asked to return for angiographic follow-up at nine months.
Study endpoints
Definitions of all endpoints are provided elsewhere10. The primary endpoint of this substudy was MACE, defined as the composite of cardiac death, MI, and clinically-indicated target vessel revascularisation (TVR) within 24 months. Secondary endpoints were any target lesion revascularisation (TLR) (both clinically and non-clinically indicated), which was defined as repeat revascularisation due to a stenosis within the stent or within a 5 mm border proximal or distal to the stent, any TVR, cardiac death, death from any cause, myocardial infarction, stent thrombosis (defined according to the Academic Research Consortium11), device success (defined as achievement of a final residual diameter stenosis of less than 50% during the initial procedure), and lesion success (achievement of less than 50% stenosis with any approach for PCI).
The pre-specified principal outcome of the angiographic substudy was in-stent percent diameter stenosis. Secondary angiographic outcomes were in-segment percent diameter stenosis, minimal lumen diameter, late lumen loss, and binary restenosis. Angiographic measurements were obtained within the stented segment (in-stent) and over the entire segment consisting of the stent and 5 mm proximal and distal margins (in segment). Percent diameter stenosis was defined as ([reference vessel diameter-minimal luminal diameter]/reference vessel diameter) × 100%; late lumen loss was defined as the difference between minimal lumen diameter after the procedure and minimal lumen diameter at follow-up; and binary restenosis was defined as a percentage diameter stenosis of 50% or greater in the target lesion.
A blinded independent clinical events committee adjudicated all endpoints, and independent study monitors (D-Target, Montagny-pres-Yverdon, Switzerland) verified all case reports from data on-site. Data were store in a database (KIKA Medical, Paris, France), which was maintained by a contract research organisation (Cardialysis, Rotterdam, The Netherlands) in collaboration with an academic clinical trials unit (CTU Bern, Bern University Hospital, Bern, Switzerland). The operators were by necessity aware of the assigned study stent during PCI and angiographic follow-up, but patients and staff involved in follow-up assessment were blinded to the allocated stent type. Angiographic films were centrally assessed at one angiographic core laboratory (Cardialysis, Rotterdam, The Netherlands) with assessors unaware of the allocated stent.
Statistical analysis
A stratified post hoc analysis of clinical and angiographic outcomes, which was specified after completion of patient recruitment, was performed according to the tertiles of SYNTAX score. The methodology used was similar to that used previously by Valgimigli et al in the ARTS-II study, and by Serruys et al in the SYNTAX trial4,5, as well as by Wykrzykowska et al8. Dedicated software and visual coronary angiography served to determine the SXscore as previously described1,2. All randomised patients without prior surgical revascularisation, in whom the SXscore was collected prospectively (1,397/1,707), were included in the analysis of primary and secondary clinical endpoints according to tertiles of SYNTAX score. Analyses of the angiographic substudy were restricted to lesions from patients who attended follow-up angiography. Angiographic outcomes were analysed using SAS v8 Proc Mixed for continuous and Proc Genmod for binominal outcomes, taking into account the within-patient correlation structure of these data. We used a Cox proportional hazards model to compare clinical outcomes between the groups. All analyses were performed using SAS 8.02 (SAS Institute Inc, Cary, NC, USA) by a dedicated statistician. All p-values and CIs were two-sided.
Results
SYNTAX SCORE and baseline characteristics
The SXscore was collected prospectively in 1,397 of the 1,707 patients (81.8%) enrolled in the LEADERS trial. The predominant reason for not calculating the score was a history of prior surgical revascularisation. In this post hoc analysis, the 1,397 patients were divided according to their SXscore into tertiles defined as: SXlow ≤8 (n=467), 8
The baseline clinical and angiographic data according to the three SXscore tertiles has been previously reported and is included in Tables 1 and 28. Briefly, the SXscore ranged from 1 to 49, with a mean ±SD of 13.5±8.7, and a median of 12 (inter-quartile range of 12; 7 to 19). Overall, at one year patients in the highest SXscore tertile had a significantly higher rate of death, TVR, MACE and a trend for high rates of MI.
Two-year clinical outcomes for the overall study population
At two-year follow-up the MACE rate was 18.4% in the SXhigh tertile, 12.0% in the SXmid and 9.4% in the SXlow tertile (HR 1.45; CI 1.21-1.74; p<0.01) (Figure 1A). In addition, there was a significantly higher rate of cardiac death in patients in the highest SXscore tertile (SXhigh 7.0% versus SXmid 2.4% versus SXlow 1.8%; HR 2.22; CI 1.5-3.27; p<0.001) (Figure 1B). Myocardial infarction was higher in patients in the SXhigh and SXmid groups (6.2%) than in patients with SXlow group (4.3%), but this difference was not statistically significant (HR 1.18; CI 0.89-1.56; p=0.24) (Figure 1E). Clinically driven TVR was 10.2% in the SXhigh group versus 6.9% and 5.2% in the SXmid and SXlow groups (HR 1.45; CI 1.14-1.85; p=0.003). (Figure 1C)
Secondary endpoint of clinically driven TLR was 10.6% in the SXhigh group versus 7.5% and 5.7% in the SXmid and SXlow groups, respectively (HR 1.38; CI 1.09-1.76; p=0.007) (Figure 1 D).
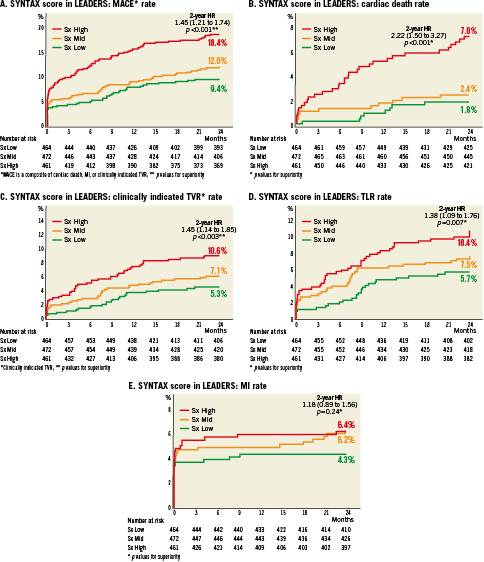
Figure 1. SYNTAX score in leaders. A) MACE rate; B) Cardiac death rate; C) Clinically indicated TVR rate; D) TLR rate; E) MI rate.
Differential performance of the BES and SES in the HIGH SYNTAX SCORE group
The analysis of outcomes in patients treated with BES versus SES was performed in all three tertiles of the SXscore, however, differences between the two devices were only apparent in the SXhigh group (highest risk) and are reported here (Figure 2). Baseline clinical and angiographic characteristics, and angiographic outcomes for the SXhigh group treated with BES versus SES are reported in Tables 3-5. There were no significant differences between BES- and SES-treated group in terms of baseline characteristics and there was an equal distribution of the two devices between the SXscore tertiles (Table 2).
Overall MACE rate was 15.3% in the SXhigh group treated with BES versus 21.8% in the SXhigh group treated with SES (HR 0.68; CI 0.44-1.04; p=0.08) (Figure 2A). Within the SXhigh tertile the rate of cardiac death was significantly lower in patients treated with BES (4.7%) than SES (9.6%) (HR 0.48; CI 0.23-0.99; p=0.046) (Figure 2B). Interaction between SXscore tertile and stent type in a five-covariate model was statistically significant (HR=0.37; p=0.036) and in a three-covariate model showed a trend towards statistical significance (HR 0.5; p=0.08), which may imply that the effect is due to chance alone given the low patient numbers analysed. TLR and TVR rates also tended to be lower in the BES-treated group (8.7% versus 12.7% for clinically driven TVR; HR 0.65; CI 0.36-1.15; p=0.14; 8.3% versus 13.1% for TLR; HR 0.59; CI 0.33-1.05; p=0.07) (Figure 2 C and D). The rate of MI remained numerically higher with BES, which was driven by early events occurring within the first nine months of stent implantation. Of note, there were no additional MIs with BES between one- and two-year follow-up compared with an increase in MI rate from 4.6% to 5.1% between year one and two in the SES-treated group (Figure 2E).
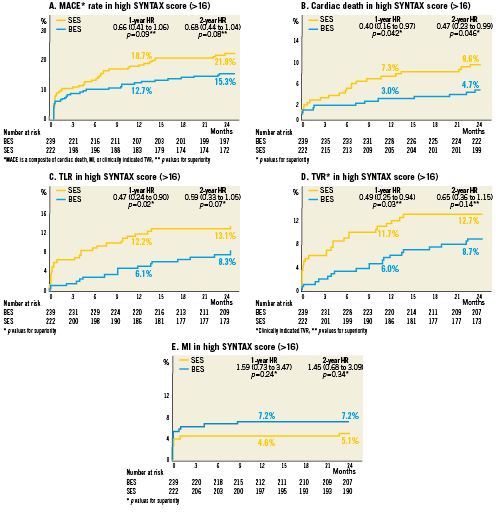
Figure 2. Two-year clinical outcomes for patients with the high SYNTAX score (>16) treated with BES versus SES.
Stent thrombosis rates for the HIGH SYNTAX SCORE group at two-year follow-up
Definite stent thrombosis rates were 2.6% in the BES-treated group and 5.1% in the SES-treated group within the SXhigh tertile at two years (HR 0.5; CI 0.18-1.34; p=0.17) (Figure 3A). Notably, there were no further definite stent thrombosis events in the BES-treated group between year one and two. In contrast, the definite stent thrombosis rate increased from 4.6% to 5.1% in the SES-treated group. Combined definite and probable stent thrombosis rates were 3.8% (n=9) for BES and 5.5% (n=12) for SES (HR 0.68; CI 0.29-1.62; p=0.39) (Figure 3B and Figure 3B’). Most of the events occurred early after stent implantation (Figure 3B’). Possible stent thrombosis was 2.6% in the BES group versus 4.8% in the SES group (HR 0.54; CI 0.2-1.49; p=0.23) (Figure 3C). The rate of overall stent thrombosis in the SXhigh group was 6.0% (n=14) in patients treated with BES and 9.8% (n=21) in patients treated with SES (HR 0.6; CI 0.31-1.18; p=0.14) (Figure 3D). The increase in stent thrombosis in SXhigh group between year one and two was 0.9% for patients treated with BES and 2.4% for patients treated with SES. When curves for cardiac death rate and overall stent thrombosis rate were superimposed, most of the cardiac death events could be accounted for by stent thrombosis events, implying that reduced thrombosis rate may be the mechanism responsible for the reduced cardiac mortality rate in patients treated with BES in the SXhigh tertile (Figure 3E), although this remains speculative.
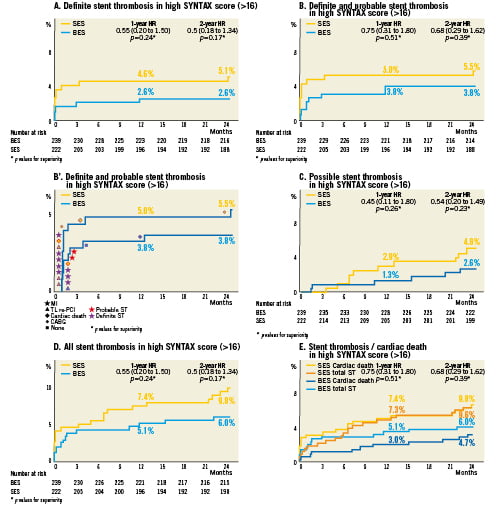
Figure 3. Stent thrombosis at 2-year follow-up.
Discussion
The SXscore has previously been applied in both the SYNTAX trial and the ARTS-II study, both of which demonstrated the good predictive value of the SXscore in patients with multivessel disease, with those patients in the highest tertile group having significantly more MACE events during short-4,5 and long-term follow-up6. More recently we reported the utility of the SXscore as a predictor of MACE, including cardiac death, in an ‘all-comers’ population of the LEADERS trial at one-year follow-up8. Patients with a high SXscore (SXscore>16) had a 50% higher chance of a MACE event, and a 154% higher chance of cardiac death at one year. A high SX score conferred a 2.5-fold increase in cardiac death, which remained true even after adjustment for other risk factors for cardiac death such as diabetes, presentation with acute coronary syndrome, beta-blocker use and stent type. Here we report that the predictive value of SXscore remains robust at two-year follow-up in this “all-comers” patient population.
The major finding of our study is that the SXscore may be an appropriate tool to stratify risk in all patients undergoing PCI out to medium-term follow-up. The second finding in this study is that SXscore appears to be able to discriminate between the performances of different types of stents in high risk lesions. Patients with high SXscores treated with BES had a lower risk of MACE and cardiac death at two-year follow-up compared with patients treated with SES. These results suggest that the SXscore may be a useful tool in future clinical trials of new stent devices, particularly those with an “all-comers” design.
The mechanism of this superior performance with BES compared to SES in the high risk lesions and patient populations remains to be established. It remains a possibility that the differences in outcome may be a play of chance considering the small number of patients in the high SXscore tertile. While the interaction between stent type and SYNTAX score tertile is significant in the five-variable model, it only shows trend toward significance in the three-variable model. Furthermore the effect is non-uniform across the SYNTAX tertiles, as BES reduces risk in the high SYNTAX score population but appears to have comparable risk in the middle tertile and higher risk in the low SYNTAX score tertile. These effects may be due to under-powering of the subgroup analysis. Speculatively, the stent thrombosis data presented here, and the previously reported optical coherence tomography data12 (Figure 4), suggest that the reduction in mortality rate by treatment with BES may be explained by the better stent strut coverage, and less acquired malapposition seen in patients treated with BES compared with SES.
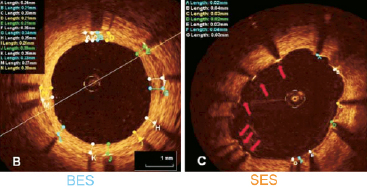
Figure 4. OCT images of strut coverage (from Barlis et al12 with kind permission from Oxford University Press).
Overall the superior performance of BES compared to SES in these complex patients provides additional data to support the concepts behind the newer generation drug-eluting stents, which were primarily designed to improve overall safety following the concerns raised with first generation devices13. In comparison to the permanent polymer present on SES, which remains exposed to the coronary artery environment long after its useful function has been served, the polymer on the biolimus-eluting stent completely biodegrades within 6-9 months of stent implantation, leaving a bare stainless steel stent. Although the lower stent thrombosis rates, and cardiac mortality observed in this study are encouraging, additional, larger-powered studies are required before definitive conclusions can be reached.
Limitations
This analysis is subject to inherent limitations of all subgroup analyses such as statistical under-powering. The interaction of the stent and SYNTAX score effects is only statistically significantly in the five-variable model and appears to be heterogeneous throughout the three SYNTAX score tertiles. As such it can only be viewed as hypothesis-generating. Patients with prior coronary artery bypass surgery have not been included in the current analysis as the SXscore algorithm is only currently available for patients with denovo disease. Modifications to the SXscore that will allow for risk stratification in patients post-CABG are being developed by our group. While the SXscore was collected prospectively, the analysis of outcomes was performed post hoc. In addition, while SXscore has not been validated in patients post-PCI and with acute myocardial infarction, these patients have been included in this analysis. The multivariate analysis was not performed utilising multiple covariates as the number of adverse events was too low to incorporate more than five, and in some instances three, variables.
Conclusion
This study demonstrates that the prognostic value of the SYNTAX score is valid for all patients with de novo coronary artery disease undergoing percutaneous revascularisation out to two-years of follow-up. A potential new application of the SYNTAX score in future clinical trials is its ability to discriminate between the performance of novel versus first-generation stents in high risk lesions. The analysis is limited, however, due to under-powering and must be considered only as hypothesis-generating.
Conflict of interest statement
The authors report no conflicts of interest as pertaining to this publication other than the following:. Funding for the paper was obtained from Biosensors Europe SA, Morges, Switzerland. S.Windecker is a consultant to Abbott, Biosensors, Boston Scientific, Cordis and Medtronic. A. Linke is a consultant to Medtronic. C.Di Mario’s institution has received a research grant from Biosensors. Dr.F.Eberli is a consultant to Cordis and has received research grants from Biosensors, Medtronic and Abbott.

