Abstract
Aims: This study aimed to assess the prognostic capacity of the residual SYNTAX score (rSS) in a large cohort of patients undergoing percutaneous coronary intervention (PCI) in clinical practice.
Methods and results: Ten thousand three hundred and forty-four (10,344) consecutive patients were prospectively enrolled. Complete revascularisation (CR; rSS=0), reasonable incomplete revascularisation (RICR; 0
Conclusions: Despite an increase in revascularisation, RICR was associated with a similar mortality and myocardial infarction to CR patients. rSS is a prognostic indicator after PCI in daily practice, and may be used to determine a reasonable level of revascularisation.
Abbreviations
CR: complete revascularisation
CTO: chronic total occlusion
ICR: incomplete revascularisation
MACCE: major adverse cardiovascular and cerebrovascular events
MI: myocardial infarction
PCI: percutaneous coronary intervention
RICR: reasonable incomplete revascularisation
rSS: residual SYNTAX score
SS: SYNTAX score
Introduction
For patients with multivessel coronary disease, percutaneous coronary intervention (PCI) frequently involves incomplete revascularisation (ICR) because of coronary anatomy complexity or co-existing serious medical conditions1,2. The prognostic impact of ICR after PCI remains inconsistent among studies3-6, which may relate to the lack of consensus on the definition of incomplete revascularisation (ICR)7.
Recently, the residual SYNTAX score (rSS), which is calculated by subtracting the value of the lesions treated during PCI from the pre-revascularisation SYNTAX score (SS), was developed to quantify and describe the extent of ICR more accurately8-17. rSS was reported to increase the prognostic capacity after PCI in different population cohorts8-17, and an rSS≥8 was identified as a level of ICR strongly associated with increased mortality and adverse ischaemic events8,9. However, the utility of rSS among unselected real-world PCI patients remains unclear. Therefore, in the present study we assessed the prognostic capacity of rSS in a large cohort of patients undergoing PCI in daily clinical practice.
Methods
STUDY POPULATION
From January 2013 to December 2013, 10,724 consecutive patients who underwent PCI were enrolled at Fu Wai Hospital, National Center for Cardiovascular Diseases, Beijing, China. After excluding patients with a history of previous coronary artery bypass grafting, 10,344 patients were finally analysed in this study. The rSS8 was assessed by two of the three experienced cardiologists in an independent angiographic core laboratory, who were blinded to clinical outcomes. In case of disagreement, the opinion of the third observer was obtained and the final decision was made by consensus. The intraobserver variability for calculation of the rSS (tertile partitioning), based on re-analysing 50 cases at a three-month interval, indicated a high level of agreement (κ statistic=0.879; 95% confidence interval [CI]: 0.81-0.94; p<0.001)18,19. The Institutional Review Board approved the study protocol, and all patients provided written informed consent before the intervention.
PROCEDURE AND MEDICATIONS
The decision on PCI strategy and stent type was left to the discretion of the treating physician. If patients were not taking long-term aspirin or P2Y12 inhibitors, they received oral aspirin (300 mg) and clopidogrel (300 mg loading dose) or ticagrelor (180 mg loading dose) at least 24 hours before the procedure. Patients with acute coronary syndrome (ACS) scheduled for PCI received the same dose of aspirin and ticagrelor or clopidogrel (300 mg or 600 mg loading dose) as soon as possible. During the procedure, unfractionated heparin (100 U/kg) was administered to all patients, and use of glycoprotein IIb/IIIa inhibitors was per the operator’s judgement. After the procedure, aspirin was prescribed at a dose of 100 mg daily indefinitely, while clopidogrel (75 mg daily) or ticagrelor (90 mg twice daily) was advised for at least one year after PCI.
PATIENT FOLLOW-UP
All patients were evaluated by clinical visit or by phone at one, three, six, and 12 months, and annually thereafter. Patients were advised to return for coronary angiography if clinically indicated by symptoms or documentation of myocardial ischaemia.
ENDPOINTS AND DEFINITIONS
Death that could not be attributed to a non-cardiac aetiology was considered cardiac death. Myocardial infarction (MI) was defined by the reported third universal definition of myocardial infarction20. Revascularisation was defined as repeat revascularisation for ischaemic symptoms and events driven by PCI or surgery of any vessel. Stent thrombosis was defined as definite or probable based on Academic Research Consortium definitions according to the level of certainty21. Major adverse cardiovascular and cerebrovascular events (MACCE) were defined as the occurrence of death, MI, revascularisation, stent thrombosis and stroke during follow-up. Procedural success was defined as residual stenosis <50% and without in-hospital MACCE. All endpoints were assessed centrally by two independent cardiologists, and disagreement was resolved by consensus.
STATISTICAL ANALYSIS
Continuous variables are reported as mean (±standard deviation), while categorical variables are reported as counts or percentage. All variables were stratified according to rSS (three groups). For the baseline characteristics, generalised linear models were used to compare continuous variables across rSS groups with rSS class as a covariable, while the Cochran-Armitage test for trends was used for categorical data. Clinical outcomes were determined using Kaplan-Meier methodology. To test for potential associations of rSS with rates of long-term mortality, a stepwise Cox multivariable regression analysis was used, with variable entry/stay criteria of 0.1/0.15. In addition, variables historically associated with long-term mortality were included in the model. The proportional hazard assumption was verified for each endpoint using the supremum test. A p-value <0.05 was considered statistically significant. Statistical analyses were performed using two statistical software packages (SPSS, Version 23; IBM Corp., Armonk, NY, USA; SAS v9.2; SAS Institute, Cary, NC, USA).
Results
PATIENT AND BASELINE CHARACTERISTICS
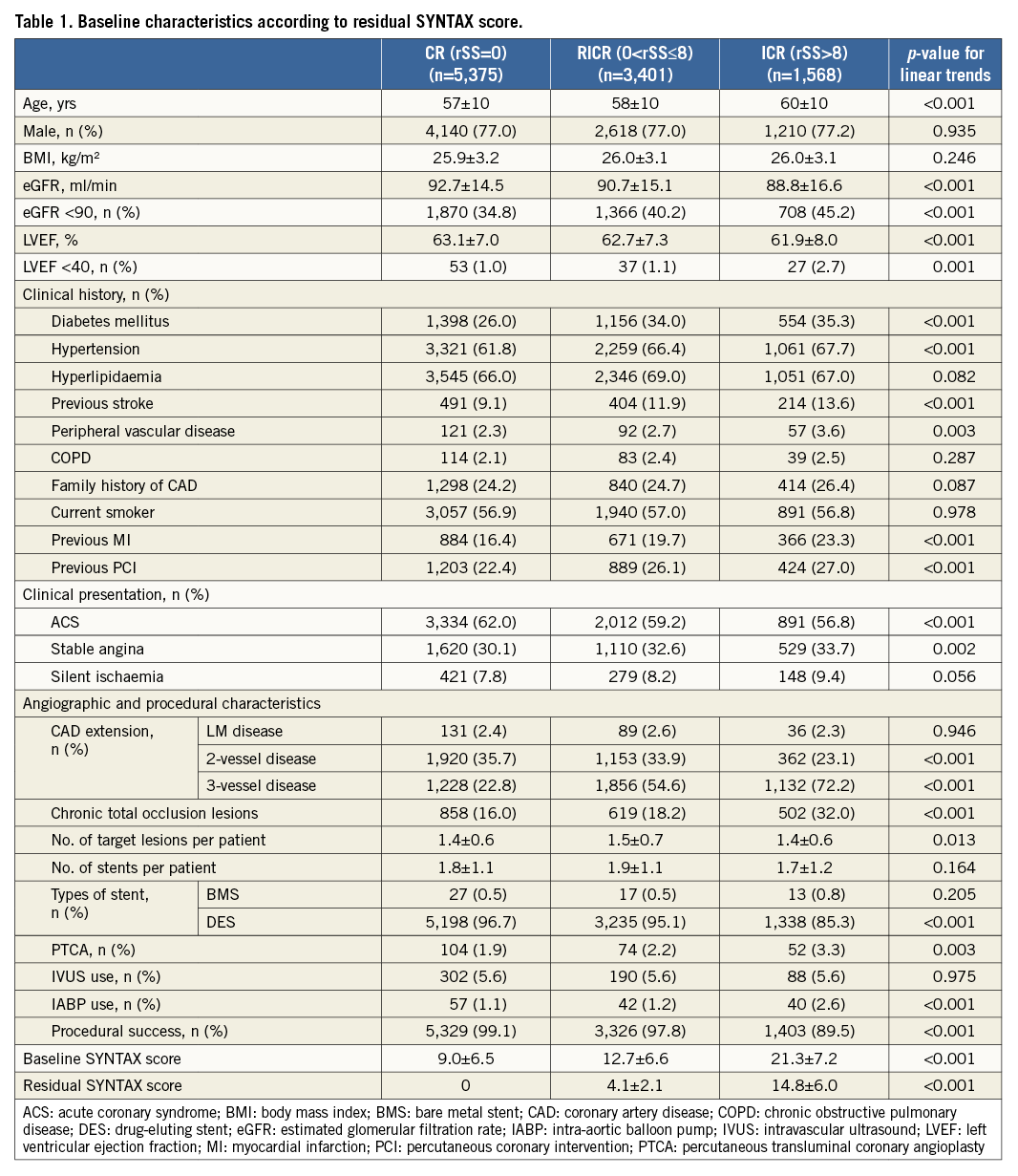
The mean baseline SS was 13.6±9.1 (range 1.0-58.0). The correlation (Spearman coefficient 0.597; p<0.001) and distribution of the baseline and residual SYNTAX score are shown in Figure 1. The CR (rSS=0), reasonable ICR (RICR) (0
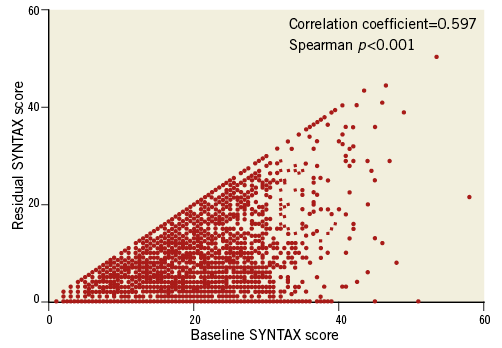
Figure 1. Correlation between the baseline and residual SYNTAX score. Relationship between the baseline (x-axis) and residual (y-axis) SYNTAX score for individual patients.

Figure 2. Distribution of complete, reasonable complete, and incomplete revascularisation of the baseline SYNTAX score.
Patients in higher rSS levels were associated with increasing clinical comorbidities, including older age (p<0.001), decreased renal function (p<0.001), lower left ventricular ejection fraction (p<0.001), diabetes mellitus (p<0.001), hypertension (p<0.001), previous stroke history (p<0.001), peripheral vascular disease (p=0.003), previous MI history (p<0.001), and previous PCI history (p<0.001). Similarly, higher rSS was associated with increasing higher baseline SS (p<0.001), three-vessel disease (p<0.001), chronic total occlusion (CTO) lesions (p<0.001), and intra-aortic balloon pump use (p<0.001) in procedures (Table 1).
CLINICAL OUTCOMES
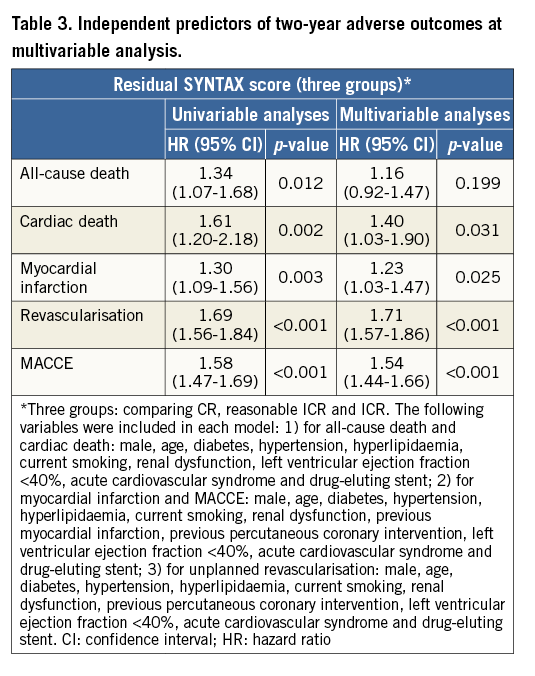
The two-year follow-up was completed for 10,287 (99.4%) patients. There were significant differences between the rates of all-cause death, cardiac death, MI, repeat revascularisation and MACCE among different rSS groups (p<0.001) (Table 2, Figure 3); ICR patients had the highest incidence of adverse clinical events (MACCE: 20.0% vs. 13.6% vs. 8.7%; p<0.001). When only comparing RICR with CR patients, the incidences of all-cause death (1.2% vs. 1.0%; p=0.45), cardiac death (0.6% vs. 0.5%; p=0.31), and MI (2.2% vs. 1.6%; p=0.07) were similar between the groups, while the MACCE rate remained significantly higher in RICR patients (13.6% vs. 8.7%; p<0.001), mainly driven by the increased risk of repeat revascularisation (9.8% vs. 5.8%; p<0.001) (Table 2). After multivariate analysis, rSS was an independent predictor of two-year cardiac death, MI, revascularisation and MACCE (p<0.05), but was not an independent predictor of two-year all-cause death (p>0.05) (Table 3).
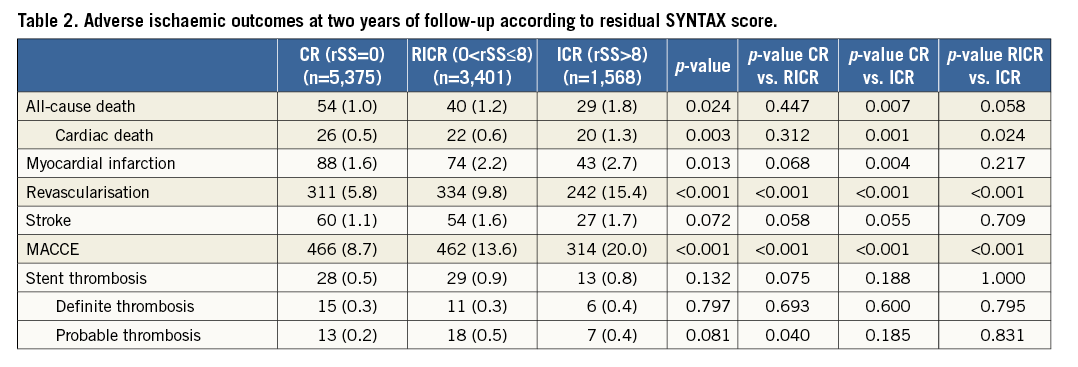
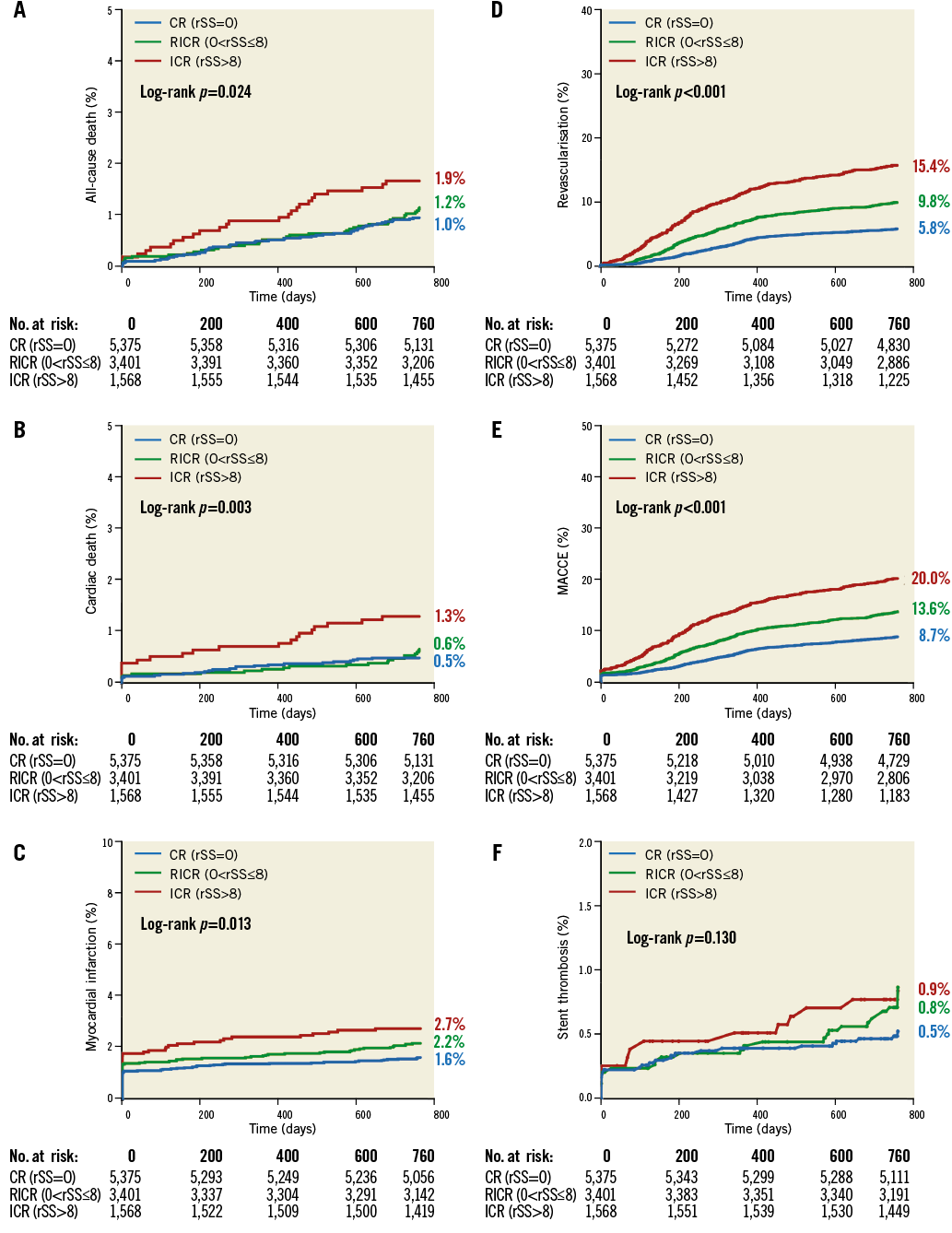
Figure 3. Kaplan-Meier curves showing event rates stratified by the residual SYNTAX score over two years. A) All-cause death. B) Cardiac death. C) Myocardial infarction. D) Revascularisation. E) Major adverse cardiovascular and cerebrovascular events (MACCE). F) Stent thrombosis. CR: complete revascularisation; ICR: incomplete revascularisation; RICR: reasonable incomplete revascularisation
SUBGROUP ANALYSIS
Overall, RICR had a similar effect on cardiac death compared with CR (0.6% vs. 0.5%, hazard ratio [HR] 1.30, 95% CI: 0.74-2.30; p=0.37), which was also observed in a subgroup of patients with impaired left ventricular function (left ventricular ejection fraction <50%, n=525/10,344 [5.1%], p=0.80 for interaction; diabetes mellitus, n=3,108/10,344 [30.0%], p=0.83 for interaction; three-vessel disease, n=4,216/10,344 [40.7%], p=0.37 for interaction; CTO disease, n=1,979/10,344 [19.1%], p=0.60 for interaction). In the meantime, except for the CTO subgroup, ICR had a higher risk of two-year cardiac death in impaired left ventricular function, diabetes mellitus, and three-vessel disease patients. The risk of MACCE was higher in RICR patients compared with CR patients in the whole population, as well as in the subgroup of impaired left ventricular function, diabetes mellitus, three-vessel disease, and CTO, which was predominantly a result of revascularisation (Figure 4).
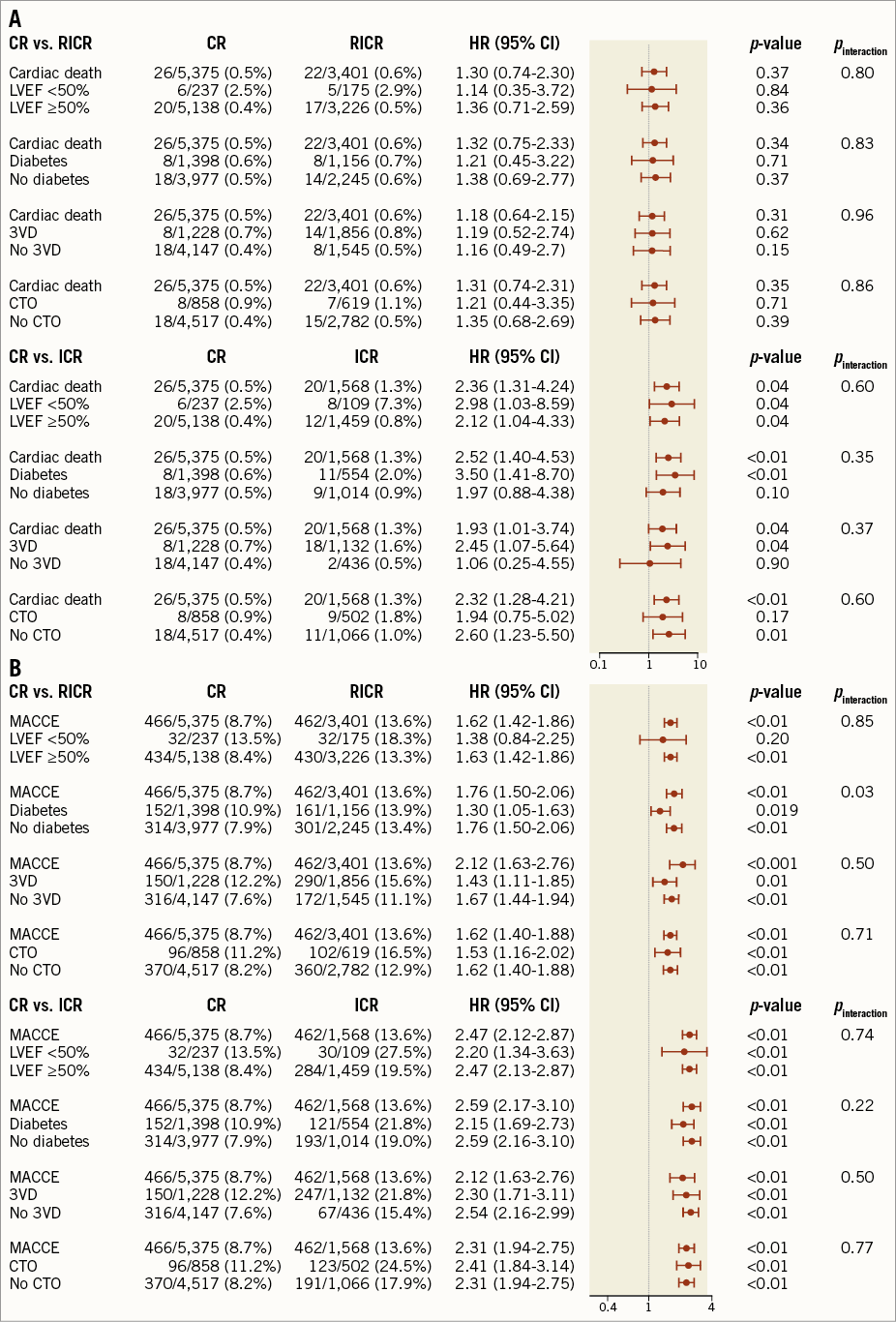
Figure 4. Subgroup analysis of all-cause death and MACCE. A) Subgroup analysis of all-cause death. B) Subgroup analysis of MACCE. CTO: chronic total occlusion; LVEF: left ventricular ejection fraction
Discussion
In the present study, we assessed the effects of rSS on clinical outcomes in a large registry cohort of real-world patients undergoing contemporary PCI treatment. The major findings of this study were as follows: 1) rSS was able to risk-stratify patients and predict two-year composite adverse cardiac events after PCI (patients with a higher rSS had a higher incidence of adverse clinical events); 2) compared with CR patients, RICR (0 Complete revascularisation was achieved in 51.9% of patients in our cohort, which was higher than that previously reported8,17. We found that patients with greater residual coronary lesions after PCI, as quantified by the rSS, had higher clinical risks including older age, decreased renal function, lower left ventricular ejection fraction, more comorbidities, and higher baseline SS. These associations reflected a clinical phenomenon whereby clinicians tended to perform ICR treatment when patients had high baseline clinical risks, as previously reported8,17. Patients in our all-comers cohort with high rSS after PCI were at significantly greater risk of MACCE, while patients with RICR (0 There is only one prior report of rSS validated in one all-comers population, where the population came from the multicentre EXCELLENT registry that enrolled 5,159 patients from 29 centres in Korea between April 2008 and May 201017. In that study, rSS was an independent predictor of clinical outcomes at one year, while there was no further benefit after lowering the rSS to <7 in patients with higher baseline SS. By comparison, our study used a larger sample size of 10,344 patients from one-centre data (this reduces the potential confounder of operator experience). Both studies demonstrated that the rSS, an index for quantifying the remaining coronary lesions after PCI, is a useful tool to evaluate patient prognosis after PCI. Further, we demonstrated that RICR was associated with similar mortality and MI compared with CR, despite an increase in revascularisation. Thus, measuring the completeness of revascularisation by rSS can be used to ensure revascularisation in daily clinical practice. Importantly, this outcome was also observed in different subgroups of patients, including those with impaired left ventricular function, diabetes mellitus, and three-vessel disease. In the CTO subgroup, ICR was associated with a modest effect on cardiac death (HR 1.94, 95% CI: 0.75-5.02; p=0.17), compared with a significant effect in no CTO patients (HR 2.60, 95% CI: 1.23-5.50, p=0.010), as previously reported9. Hannan et al22 also reported that patients with successful CTO revascularisation in conjunction with ICR of other diseased lesions had a similar risk to patients with CR of all diseased lesions, suggesting that RICR may be a treatment target for high-risk CTO patients. Moreover, preprocedural assessment such as myocardial viability testing was required to ensure revascularisation in CTO patients. Study limitations There are a number of limitations in our study. First, the non-randomised design using unmeasured confounders may preclude any definitive conclusion. Second, the two-year follow-up duration was comparatively short for evaluating long-term outcomes. Third, patients enrolled in this study had lower levels of complex coronary artery disease and incidence of mortality compared with the SYNTAX trial. Fourth, rSS is based on angiographic interpretation that has inherent limitations23, and our findings may have varied if the SS had been assessed by less well-trained readers. However, rSS was assessed by an independent angiographic core laboratory in this study, with good reproducibility for rSS evaluation15. Finally, the patients in this study only included those receiving PCI treatment. Thus, use of rSS should also be validated in patients receiving coronary artery bypass graft therapy. Conclusions In this large cohort of real-world patients receiving PCI, RICR was associated with similar mortality and MI compared with CR, despite an increase in revascularisation. Thus, RICR may be a treatment target for high-risk patients. rSS was a prognostic indicator after PCI in daily practice, and may be useful for determining a reasonable level of revascularisation. Impact on daily practice The utility of rSS in real-world PCI patients is unclear. In this study, rSS was able to risk-stratify patients and predict two-year composite adverse cardiac events after PCI. ICR patients (rSS>8) had a higher incidence of adverse clinical events compared with CR patients (rSS=0), while RICR patients (0 Acknowledgements The authors thank staff in the Department of Cardiology and Catheterization Laboratory, Fu Wai Hospital, for their research contributions. Funding This study was funded by The National Key Research and Development Program of China (2016YFC1301301). Conflict of interest statement The authors have no conflicts of interest to declare.