Abstract
Aims: The aim of this study was to explore the utility of baseline SYNTAX score (bSS) and residual SYNTAX score (rSS) in predicting 12-month outcomes after primary percutaneous coronary intervention (PPCI).
Methods and results: Five hundred and ninety all-comers with acute STEMI presenting for PPCI over a two-year period were identified. Of these, 173 were excluded because of unsuitability for SYNTAX score calculation for this study. Two experienced observers calculated the bSS and rSS. Mortality data were sourced from the government registry. Logistic regression was used to assess the predictive power of bSS and rSS for mortality. Sensitivity analysis and a Cox proportional hazards model were used to evaluate the best cut-off for increased mortality. Of the 417 patients analysed (mean age 59 years), 81% were male and 18% were known diabetics. At 12 months, the overall mortality rate was 5.5% (23/417). An rSS of >12 was associated with a 13.95% mortality rate. The hazard ratio for mortality was 3.88 (95% CI: 1.49-10.09, p=0.005) for rSS of >12 and 3.01 (95% CI: 1.18-7.64, p=0.02) for bSS >12. The odds ratio (OR) for mortality was 1.06 (95% CI: 1.02-1.11, p=0.009) for rSS and 1.05 (95% CI: 1.02-1.1, p=0.007) for bSS.
Conclusions: In STEMI patients undergoing PPCI, both bSS and rSS can predict mortality at 12 months. Every point on the rSS confers an additional 6% mortality risk. Calculation of the rSS after culprit lesion intervention may help guide management of non-culprit lesions.
Introduction
Mortality after acute ST-elevation myocardial infarction (STEMI) has been greatly lowered by recognition of primary percutaneous coronary intervention (PPCI) as the standard of care and the development of efficient PCI laboratory activation systems1. The maturation of this clinical therapy and process has sparked renewed interest in the issue of non-culprit vessel intervention during the PPCI procedure2,3. Up to 65% of patients with STEMI have multivessel disease4. Current guidelines, however, recommend intervention on only the infarct-related artery during the PPCI procedure, except when there is ongoing ischaemia, haemodynamic instability or cardiogenic shock5. Whereas a decade ago multivessel PCI for STEMI might have been regarded as reckless, currently it is reasonable to consider that complete revascularisation during the index procedure or admission might reduce the ischaemic burden, promote clinical recovery and even improve prognosis. To address the question of the timing of non-culprit vessel PCI in those with multivessel disease, scoring systems already in clinical use may be utilised. The SYNTAX score (SS), initially proposed to risk stratify multivessel and left main coronary disease from a revascularisation perspective6, reliably predicts long-term outcomes after PCI even up to five years7,8. The residual SYNTAX score (rSS), which quantifies the extent and complexity of the residual burden of disease following PCI, has also been shown to predict outcomes in patients with multivessel disease undergoing intervention for non-ST-elevation acute coronary syndromes (NSTEACS)9. To the best of our knowledge, no randomised trials have assessed the utility of the SS or rSS in STEMI. This study examines their correlation with clinical outcome in STEMI patients undergoing PPCI and analyses the utility of the rSS in predicting mortality by 12 months.
Methods
STUDY POPULATION
The study was part of a PCI quality assurance programme that received institutional review board approval. Our centre performs round-the-clock PCI for acute STEMI with ambulance activation of the PCI laboratory in most cases. In this observational study, we included all PPCI patients presenting to the cardiac catheter laboratory at our tertiary cardiac centre from January 2012 to December 2013. We excluded patients who had failed fibrinolysis and who underwent rescue PCI (n=78), incipient or established cardiogenic shock necessitating multivessel PCI (n=68), patients with an ST-elevation pattern on ECG who did not require PPCI because of minimal stenosis, or who actually had pericarditis or stress cardiomyopathy (n=12), those with symptom onset >12 hrs prior to presentation (n=9) and patients with previous coronary artery bypass grafting (n=6). All patients proceeding to PPCI received a loading dose of 300 mg aspirin plus 600 mg clopidogrel and 70 U/kg of intravenous heparin. Dual antiplatelet therapy was continued for at least 12 months following the index event. Glycoprotein IIb/IIIa inhibitor and aspiration thrombectomy use were at the operator’s discretion.
DATA COLLECTION
Data regarding patient characteristics, procedural details and repeat angiography were obtained from patient records and a prospective statewide database that allows review of all angiograms and PCI procedures performed in the state. Mortality data were obtained from the government registry of births, deaths and marriages.
Two experienced observers reviewed the angiograms included for final analysis. The inter-observer variability between these two observers was tested before the commencement of this study and was within acceptable limits. The observers were blinded to the mortality and re-angiography data. Using the online version 2.11 (www.SYNTAXscore.com), the baseline SYNTAX score (bSS) was calculated from the diagnostic images and the residual SYNTAX score (rSS) was determined from images acquired after the culprit vessel PCI. Coronary artery branches smaller than 2.0 mm or those with less than 50% stenosis were not included in the SYNTAX score calculation.
ENDPOINTS AND STATISTICAL ANALYSIS
Our pre-specified hypothesis was that a higher rSS after PPCI translates to a higher risk of death. The primary endpoint was all-cause mortality at 12 months. The secondary endpoint was a composite of death and unplanned re-angiography by 12 months.
Logistic regression analysis was used to estimate the predictive power of bSS and rSS for the primary and secondary endpoints. Receiver operating characteristic (ROC) curves were plotted to compare the predictive ability of bSS and rSS. The best rSS cut-off was identified by sensitivity analysis and tested by the Cox proportional hazards model. Kaplan-Meier curves were generated to estimate the survival function of the study population stratified by the best cut-off of rSS >12; the difference in survival was compared using the log-rank test.
Results
There were 590 all-comer PCI lab activations over the two-year study period. Of these, 29% (173/590) were excluded from the final analysis as previously explained. Of 417 patients analysed, the mean age was 59 years (±12), 81% (340/417) were male and 18% (76/417) were known to have diabetes mellitus at presentation (Table 1). All procedures were performed using the femoral access. Follow-up was complete and censored at 12 months for the entire cohort.
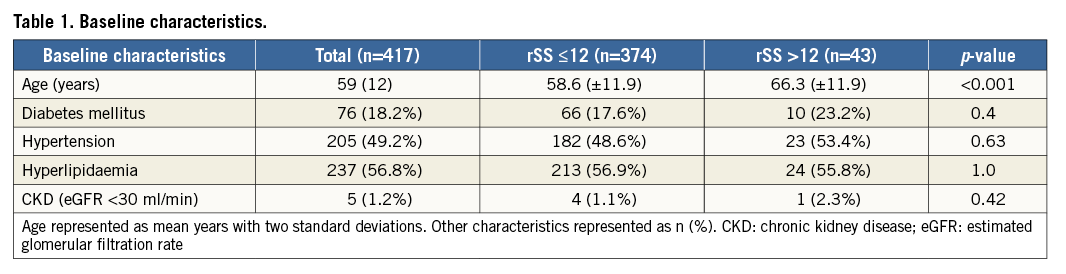
The median bSS was 14 (IQR=8-19.5). After PPCI, the median rSS was 2 (IQR=0-7); 43.6% (182/417) had rSS >2 and only seven patients had rSS between 27 and 37. Culprit vessel PCI resulted in complete revascularisation in 173/417 (41.5%) of patients. Multivessel PCI was performed in 18 cases (4.3%), leaving no significant residual disease. There was a not unexpected correlation between bSS and rSS (r2=0.63, p<0.01). The primary endpoint of all-cause mortality occurred in 5.5% (23/417). Both bSS and rSS predicted mortality. The rSS had only a marginally higher correlation with mortality (OR 1.06, 95% CI: 1.02-1.11, p=0.009) than bSS (OR 1.05, 95% CI: 1.02-1.1, p=0.007). After adjusting for age and baseline variables of diabetes, hypertension, hyperlipidaemia and chronic kidney disease, both rSS (OR 1.061, 95% CI: 1.011-1.113, p=0.017) and bSS (OR 1.063, 95% CI: 1.017-1.111, p=0.007) retained significant correlation with mortality. This, however, should be interpreted with caution, the small number of patients with the primary endpoint allowing statistical correction for only two variables10.
When tested for the secondary composite endpoint, the odds ratio was 1.04 (95% CI: 1.0-1.08, p=0.015) for bSS and 1.03 (95% CI: 0.99-1.08, p=0.12) for rSS. A non-parametric ROC analysis for predicting the primary endpoint revealed the area under the curve (AUC) to be similar (Figure 1): 0.65 for rSS and 0.66 for bSS (x2=0.01, p=0.94)11. Sensitivity analysis showed an rSS of >12 to classify 87.06% of the cohort correctly, with a 90.86% specificity and 26.09% sensitivity for predicting death (LR+=2.78, LR-=0.81) (Figure 2). Patients with an rSS >12 were older but were otherwise well matched in baseline risk factors with those in whom the rSS was ≤12 (Table 1). The two groups were also similar in the use of glycoprotein IIb/IIIa inhibitors (p=0.1) and aspiration thrombectomy (p=0.26).
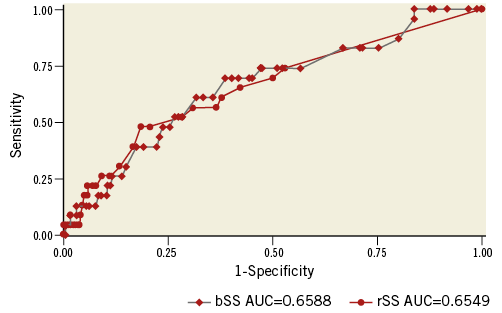
Figure 1. The ROC curves reveal no significant difference between baseline and residual SYNTAX score for predicting death. chi²=0.01, p=0.94; AUC: area under the curve; bSS: baseline SYNTAX score; rSS: residual SYNTAX score
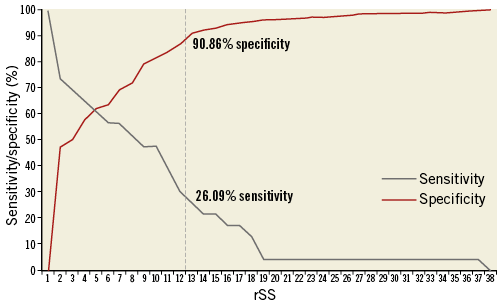
Figure 2. Sensitivity and specificity for mortality over the range of rSS. A score of 12 has a clinically useful trade-off between specificity and sensitivity to suggest a prognostic role for pre-emptive PCI. rSS: residual SYNTAX score
Most deaths (74%, 17/23) occurred in the first 30 days after the PPCI procedure (Figure 3). There were 16 cardiac deaths, six deaths from neurologic events and one death from sepsis. There was no significant difference in the cause of death between the two rSS groups when compared with a Fisher’s exact test (p=0.25). The absolute mortality was 13.95% (6/43) in those with an rSS >12 and 4.55% (17/374) in those with an rSS ≤12. When dichotomised by rSS, a Cox proportional hazards model indicated a hazard ratio for mortality of 3.88 (95% CI: 1.49-10.09, p=0.005) for an rSS of >12. For bSS, the hazard ratio for mortality was 3.01 (95% CI: 1.18-7.64, p=0.02). A log-rank test showed a significant difference between the survival function of the two rSS groups (p=0.006).
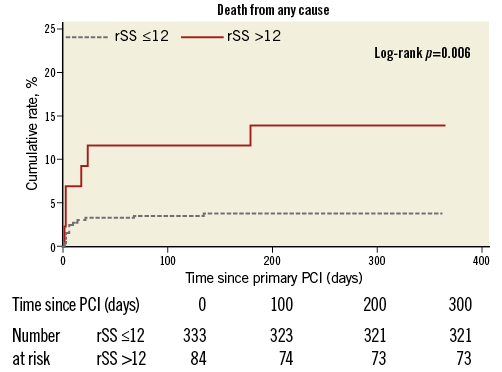
Figure 3. The majority of the deaths occurred in the first 30 days after the primary PCI procedure. rSS: residual SYNTAX score
Discussion
Patients with multivessel disease and STEMI do worse than those with only a single culprit lesion12,13, yet the need for and timing of PCI for bystander lesions in STEMI remain contentious. Studies on which current guidelines were based indicated that intervention on only the culprit lesion during the index procedure was safer than complete revascularisation14-16. A recent large observational study also reported worse outcomes with bystander lesion intervention during PPCI17. In contrast, several smaller studies and a meta-analysis had suggested benefit from non-infarct artery PCI during the primary procedure18-21. Two recent randomised trials also suggest that pre-emptive non-culprit lesion intervention (i.e., during PPCI or the same admission) can reduce major adverse cardiac events in the short to medium term2,3, such that future guidelines might be expected to reflect the new evidence more strongly. Our study lends support to the option of pre-emptive prognosis-modifying revascularisation by providing some insight based on residual disease burden and complexity.
A higher rSS is associated with worse short- and long-term outcomes in those with NSTEACS22. It also predicts mortality in non-ACS patients undergoing PCI and can be used as a tool to define complete revascularisation23,24. Our study shows that the rSS can also predict outcomes in the STEMI population undergoing PPCI. A higher score portends a higher mortality over 12 months (Figure 4). Our data indicate that a residual score of >12 was 90% specific in predicting death by 12 months after PPCI. By comparison, after PCI in non-emergent situations, previous studies have suggested that an rSS >8 is associated with worse long-term outcomes9,22. A typical example where the rSS is >12 is a patient with a treated culprit right coronary artery and normal circumflex but significant bystander proximal and mid LAD lesions >20 mm in length. Although an rSS >12 had a sensitivity of only 26% in our population, this has the potential effect of minimising unnecessary or inappropriate procedures in our busy centre. We acknowledge however that each centre or operator may work under different clinical circumstances and so Figure 2 is useful in providing some guidance on the clinical management of the individual case. For instance, an rSS >8 has a sensitivity of almost 50% with a concomitant reduction in specificity to 80% (Figure 2), which might be appropriate to an individual clinical scenario.
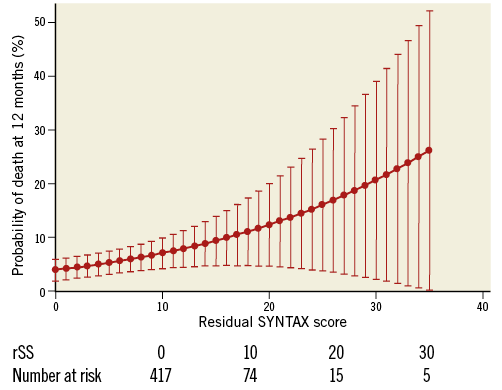
Figure 4. A higher residual SYNTAX score portends worse long-term outcomes. rSS: residual SYNTAX score
The practice in our centre has traditionally leant towards guideline adherence5, intervention being performed on only the infarct-related artery during the index PPCI, followed by the staged treatment of any non-culprit lesions, as determined by the operator, usually within four to six weeks of the index procedure. Other patient factors that are not measurable but impact on decision making (e.g., proximity to an interventional centre, compliance with medications) may also have influenced outcomes. Our data however are representative of real-world practice. We found that every additional point on the rSS imparts a 6% greater risk of death at 12 months (Figure 4). One in seven patients with an rSS of >12 had died by 12 months. Most deaths occurred in the first 30 days following PPCI. We therefore propose a quick and pragmatic calculation of the rSS after treatment of the culprit vessel during PPCI and performing further revascularisation during the same admission if possible but certainly within 30 days in those with an rSS >12 for whom such proactive management is clinically appropriate. These conclusions pertain specifically to the STEMI PPCI population and are not applicable to stable patients with a high SYNTAX score.
This small hypothesis-generating study in a single high-volume tertiary centre highlights the desirability of larger or randomised studies to confirm the usefulness of the rSS in managing residual disease in the general STEMI population undergoing PPCI. The process of randomising the acute STEMI patient for a clinical PPCI trial is fraught with difficulty and no small measure of controversy.
Limitations
Although our study was by design a retrospective analysis of hard endpoints from a period before clinical practice could potentially be influenced by the results of PRAMI and CvLPRIT2,3, selection bias in the decision making might still have impacted on observed outcomes after PPCI. We acknowledge that our then usual timing of staging any further angioplasty four to six weeks following the index procedure might have influenced medium-term outcomes, and that it remains unproven that earlier PCI may pre-empt early cardiac mortality. Also, we have not extended follow-up beyond 12 months. Undoubtedly, a larger cohort of patients might have revealed a stronger association between rSS and 12-month mortality. Notwithstanding these limitations, the rSS still appeared to have some predictive utility in the short to medium term.
Conclusions
In conclusion, for STEMI patients undergoing PPCI, both bSS and rSS can predict mortality at 12 months. The rSS, as an easy to calculate index of residual coronary disease severity, is intuitively more meaningful to apply in this setting. Pending further definitive trials, we suggest that it may usefully be factored into proactive decision making about the need for and timing of any pre-emptive revascularisation of significant residual disease.
| Impact on daily practice The results of this study indicate that primary PCI patients with significant residual disease do worse than those with less severe disease. This calls for a rethink of strategies to deal with treatable residual disease. The residual SYNTAX score has promising utility in identifying those who might benefit from pre-emptive non-infarct artery intervention during the primary PCI procedure or soon after. |
Acknowledgements
The authors thank Dr Lucinda Hogan from The University of Queensland/King’s College London School of Medicine for help with data management.
Conflict of interest statement
The authors have no conflicts of interest to declare.