Abstract
Aims: The SYNTAX score is a tool to quantify the complexity of coronary artery disease. We investigated the relation between the SYNTAX score and the occurrence of a periprocedural myocardial infarction (PMI) according to the historical definition of the World Health Organization (WHO) and the recently updated universal definition of MI.
Methods and results: The SYNTAX score was calculated in 1,243 patients enrolled in TWENTE, a randomised trial which assessed second-generation drug-eluting stents. PMI was defined by the WHO definition and the third universal definition of MI. Patients were divided into tertiles of the SYNTAX score: ≤7 (n=430); >7 and <15 (n=390); ≥15 (n=423). PMI according to the WHO definition occurred more frequently in patients in the highest SYNTAX score tertile (7.3% vs. 3.1% vs. 1.6%, p<0.001) compared to the mid and lowest tertile. Similar findings were seen for universal PMI (9.9% vs. 7.7% vs. 3.7%, p<0.01). After multivariate analysis, SYNTAX score was a significant independent correlate of PMI for both definitions: the highest SYNTAX score tertile had an almost five times higher risk for WHO PMI, and a three times higher risk for universal PMI.
Conclusions: In a broad patient population treated with second-generation DES, the SYNTAX score was able to stratify the risk of PMI.
Abbreviations
CABG: coronary artery bypass grafting
CK: creatine kinase
CK-MB: creatine kinase-MB
DES: drug-eluting stents
MI: myocardial infarction
PCI: percutaneous coronary intervention
PMI: periprocedural myocardial infarction
STEMI: ST-elevation myocardial infarction
WHO: World Health Organization
Introduction
The SYNTAX score is a tool for the assessment of the degree and complexity of atherosclerotic disease burden of coronary arteries. It incorporates several pre-existing scoring systems such as the Leaman classification, American Heart Association/American College of Cardiology, modified BARI classification, and chronic total occlusion and bifurcation scores1.
Currently, the SYNTAX score is used mainly as a tool to evaluate the suitability of patients with multivessel disease to undergo coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI)2. In addition to this application, the SYNTAX score may also be useful to stratify the risk of periprocedural complications. Myocardial infarction after a percutaneous coronary intervention (PCI) is the most common procedural complication and is an important endpoint in coronary stent trials3. There is controversy about the clinical impact of periprocedural myocardial infarction (PMI); however, several studies have shown a relation between PMI and increased mortality4-6. So far, there are no established risk models for the prediction of PMI.
Therefore, in 1,243 real-world PCI patients from the randomised TWENTE trial7,8, treated with second-generation drug-eluting stents (DES), we assessed the relation between SYNTAX score and the occurrence of PMI, as defined by the extended historical WHO definition as well as the recently updated third universal definition of MI.
Methods
STUDY DESIGN AND PATIENT POPULATION
The randomised TWENTE trial (ClinicalTrials.gov NCT01066650) has previously been described and reported7,8. In brief, TWENTE was an investigator-initiated, patient-blinded, randomised, comparative DES trial with limited exclusion criteria in 1,391 “real-world” PCI patients with a majority of complex lesions and off-label indications for DES. The study was performed between June 2008 and August 2010 at Thoraxcentrum Twente, Enschede, The Netherlands. Patients capable of providing informed consent with an indication for PCI with DES were randomised for treatment with Resolute™ (Medtronic, Santa Rosa, CA, USA) or XIENCE V® stents (Abbott Vascular, Santa Clara, CA, USA) in a 1:1 ratio. There were no angiographic exclusion criteria such as a mandatory lesion length, reference vessel size, and number of target lesions or vessels. The main exclusion criterion was a recent ST-elevation myocardial infarction (STEMI). More than 81% of the eligible patients were enrolled in this trial9.
In all trial participants, except for 148 patients with a history of CABG, SYNTAX score was prospectively assessed by analysts of the angiographic core laboratory at the Thoraxcentrum, Twente. The study was approved by the institutional ethics committee and complied with the Declaration of Helsinki. All patients provided written informed consent.
DEFINITION AND ASSESSMENT OF PMI
PMI was defined by the extended historical WHO definition (WHO PMI; total CK >2x normal with elevated CK-MB or, in the case of ongoing MI, CK >2x normal and ≥50% above the previous level if the baseline values are elevated, in addition to symptoms) and the third universal definition of MI (troponin >5x normal or, in the case of ongoing MI, a rise of troponin values >20% if the baseline values are elevated, in addition to symptoms, ECG changes, angiographic findings or new regional wall motion abnormalities)10,11.
In all patients, cardiac biomarkers and electrocardiograms were systematically assessed before and after index PCI or staged procedure in order to identify PMI. Cardiac biomarker measurements were scheduled before PCI and six to 18 hours after PCI, with subsequent serial measurements for relevant biomarker increases or complaints, until peak increase was established. Adjudication of WHO PMI was performed by an external clinical events committee (Cardialysis, Rotterdam, The Netherlands), and adjudication of PMI according to the universal definition of MI was performed by three experienced cardiologists/research physicians.
STATISTICAL ANALYSIS
Categorical variables were assessed with the use of the χ2 or Fisher’s exact test, as appropriate, whereas continuous variables were assessed with the Wilcoxon rank-sum test or Student’s t-test, as appropriate. Means are given with standard deviation (SD) and medians with an interquartile range (IQR). Univariate and multivariate logistic regression analyses were performed to assess the relationship between the SYNTAX score and PMI. We constructed three models: Model 1 including clinical variables with a univariate association with PMI p<0.10; Model 2 being the full model with variables with a univariate association with PMI p<0.10, in addition to other clinical variables used in similar research which evaluated the SYNTAX score and its relation to clinical outcome (i.e., presentation with acute coronary syndrome, age, sex, stent type, history of MI, history of PCI, and chronic renal failure)12. In Model 3, only the SYNTAX score and the variable total stent length were entered into the model. Variables were simultaneously put into a multivariate model using the forced enter method, without exit criteria. Variables which are included in the SYNTAX score (i.e., vessel diameter, lesion length) were not included in the model to avoid collinearity. The variable left ventricular ejection fraction (LVEF) <30% was not included in this model, as data on LVEF were not available for all patients. In order to compare SYNTAX score versus the AHA/ACC lesion classification and their relation to PMI, we compared the -2 log-likelihood of the full multivariate model with SYNTAX score in it with the -2 log-likelihood of the same model but with the SYNTAX score replaced by the AHA/ACC lesion classification. A higher -2 log-likelihood suggests a better model.
Unless otherwise specified, p-values and confidence intervals (CIs) were two-sided. A p-value <0.05 was considered significant. All statistical analyses were performed with SPSS Version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
SYNTAX SCORE AND BASELINE CHARACTERISTICS
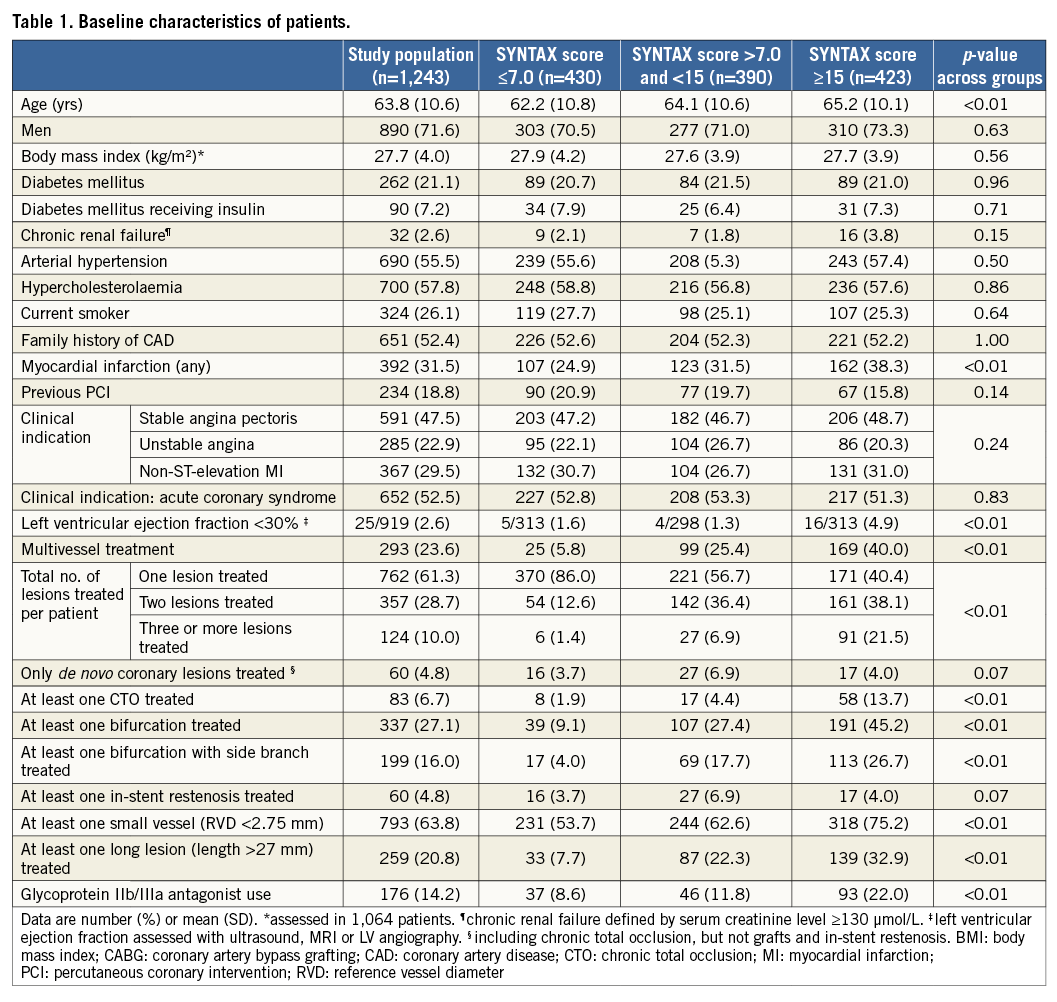
The SYNTAX score was assessed in 1,243 of the 1,391 patients (89.4%) of the TWENTE trial who had not undergone previous CABG. The mean SYNTAX score was 12.45±8.36, and the median SYNTAX score was 11.00 (IQR 6.00-24.00). Based on tertiles of the SYNTAX score, the SYNTAX score was ≤7.0 in 430 patients, >7.0 and <15.0 in 390 patients, and ≥15 in 423 patients.
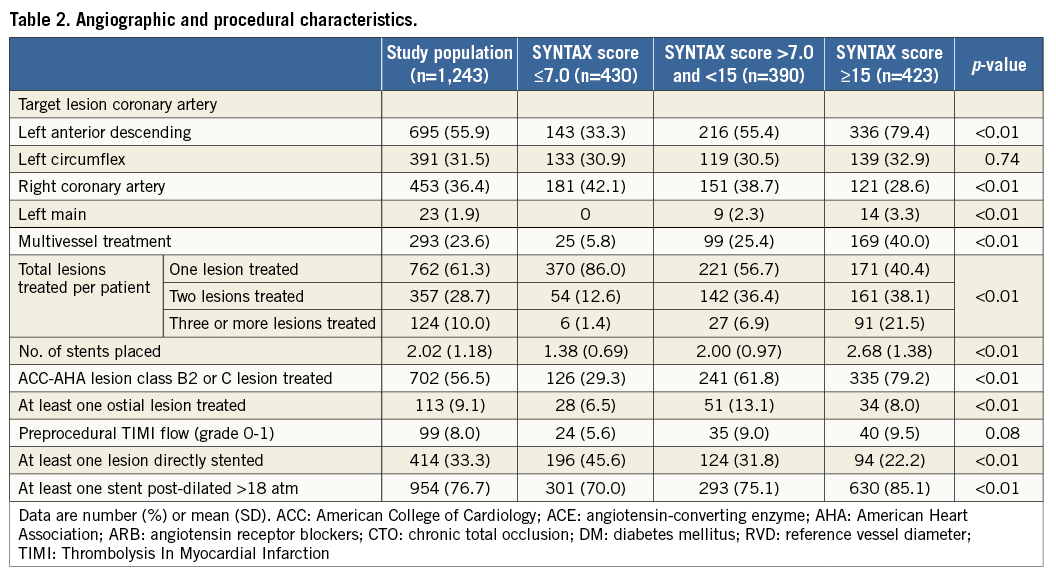
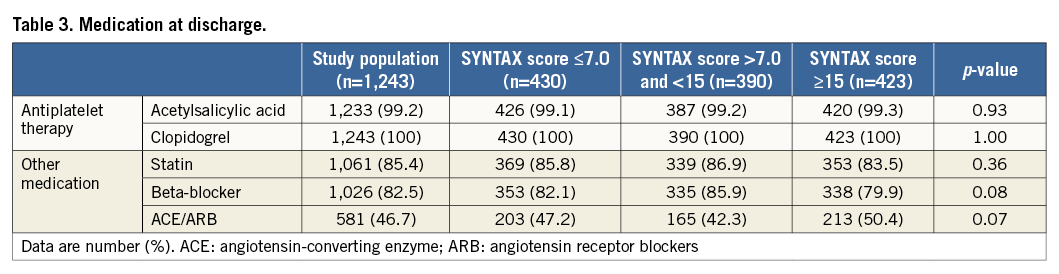
Baseline characteristics and angiographic and procedural characteristics are described in Table 1 and Table 2. Patients with the highest SYNTAX score (≥15) were older (p<0.001) and were more likely to have an LVEF <30% (p=0.008) and a previous myocardial infarction (p<0.001). Post-dilation with balloon pressures >18 atm and use of glycoprotein IIb/IIIa antagonists were more frequent in patients with a higher SYNTAX score (p<0.001). Medication at discharge did not differ between groups (Table 3).
INCIDENCE OF PMI
The incidence of PMI according to the extended historical WHO definition and universal definition, stratified for SYNTAX score, is shown in Table 4. MI according to the extended historical WHO definition occurred more frequently in patients of the highest SYNTAX score tertile (7.3% vs. 3.1% vs. 1.6%, p<0.001) as compared to the mid and lowest SYNTAX score tertiles. In addition, PMI according to the third universal definition occurred more frequently in patients of the highest SYNTAX score tertile (9.9% vs. 7.7% vs. 3.7%, p=0.002). The difference in definitions of PMI impacts on the diagnosis of PMI. This is shown in Figure 1.
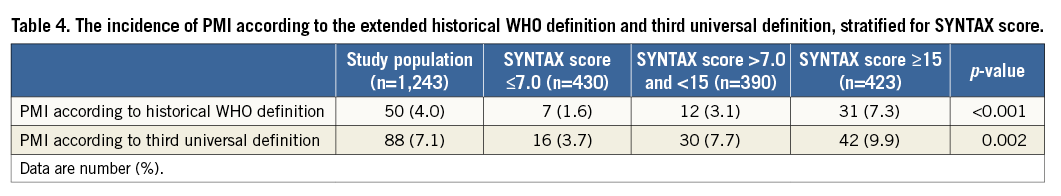
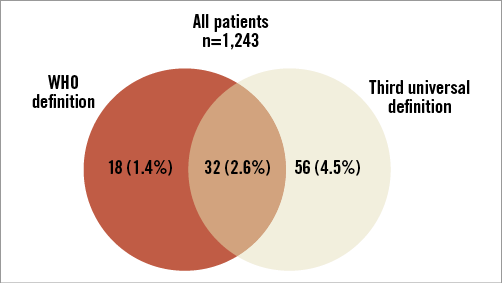
Figure 1. Venn diagram illustrating the overlap and differences of the definitions of PMI according to the WHO and third universal definition.
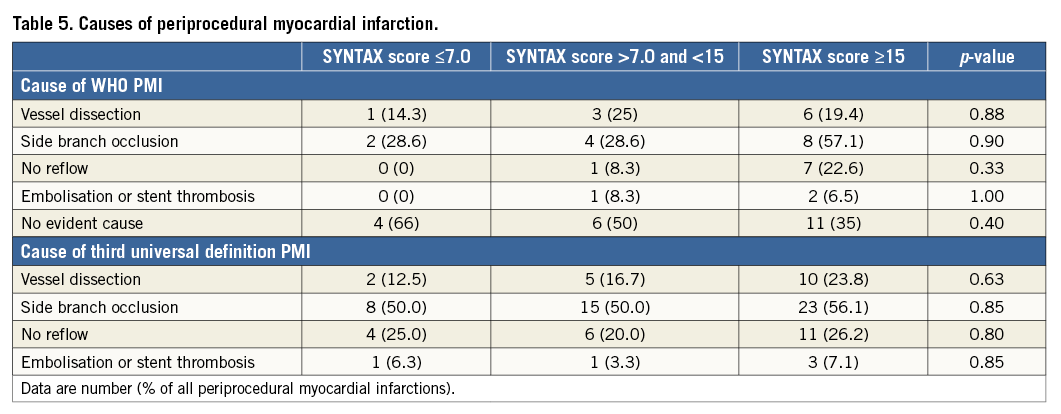
CAUSES OF PMI
The causes of PMI are shown in Table 5. According to the extended historical WHO definition, the cause of PMI was a vessel dissection in 20%, side branch occlusion in 28%, no reflow in 16%, and embolisation or stent thrombosis in 6%. In 42%, no angiographic reason was found for the occurrence of WHO PMI. For PMI according to the third universal definition, the cause of PMI was a vessel dissection in 19%, side branch occlusion in 52%, no reflow in 24% and embolisation or stent thrombosis in 6%. In 18%, no angiographic reason was found for the occurrence of PMI according to the updated third universal definition. As shown, certain causes were not statistically more prevalent in higher SYNTAX scores.
MULTIVARIATE ANALYSIS
Table 6 shows the complete results of the multivariate analysis. After multivariate analysis, adjusting for covariates, SYNTAX score was a significant independent predictor of PMI according to both definitions. Patients with the highest tertile of the SYNTAX score, compared to the lowest tertile, had an almost five times higher risk of PMI according to the historical WHO definition (adjusted odds ratio [OR] 4.95, 95% confidence interval [CI]: 2.13-11.52) and an almost three times higher risk according to the updated PMI definition (adjusted OR 2.84, 95% CI: 1.55-5.19) (Figure 2). On a continuous scale, SYNTAX score was also a significant independent predictor of PMI according to the extended historical WHO definition (adjusted OR 1.07, 95% CI: 1.04-1.10, p<0.001) and the third universal definition (adjusted OR 1.04, 95% CI: 1.01-1.06, p=0.002). When total stent length implanted was entered into the multivariate model (Model 3), there was a trend that patients with the highest tertile of the SYNTAX score, compared to the lowest tertile, had a higher risk of PMI according to the WHO definition (adjusted OR 2.51, 95% CI: 0.98-6.39, p=0.054), but not according to the third definition of MI. Total stent length implanted was also a significant correlate for both definitions of PMI.
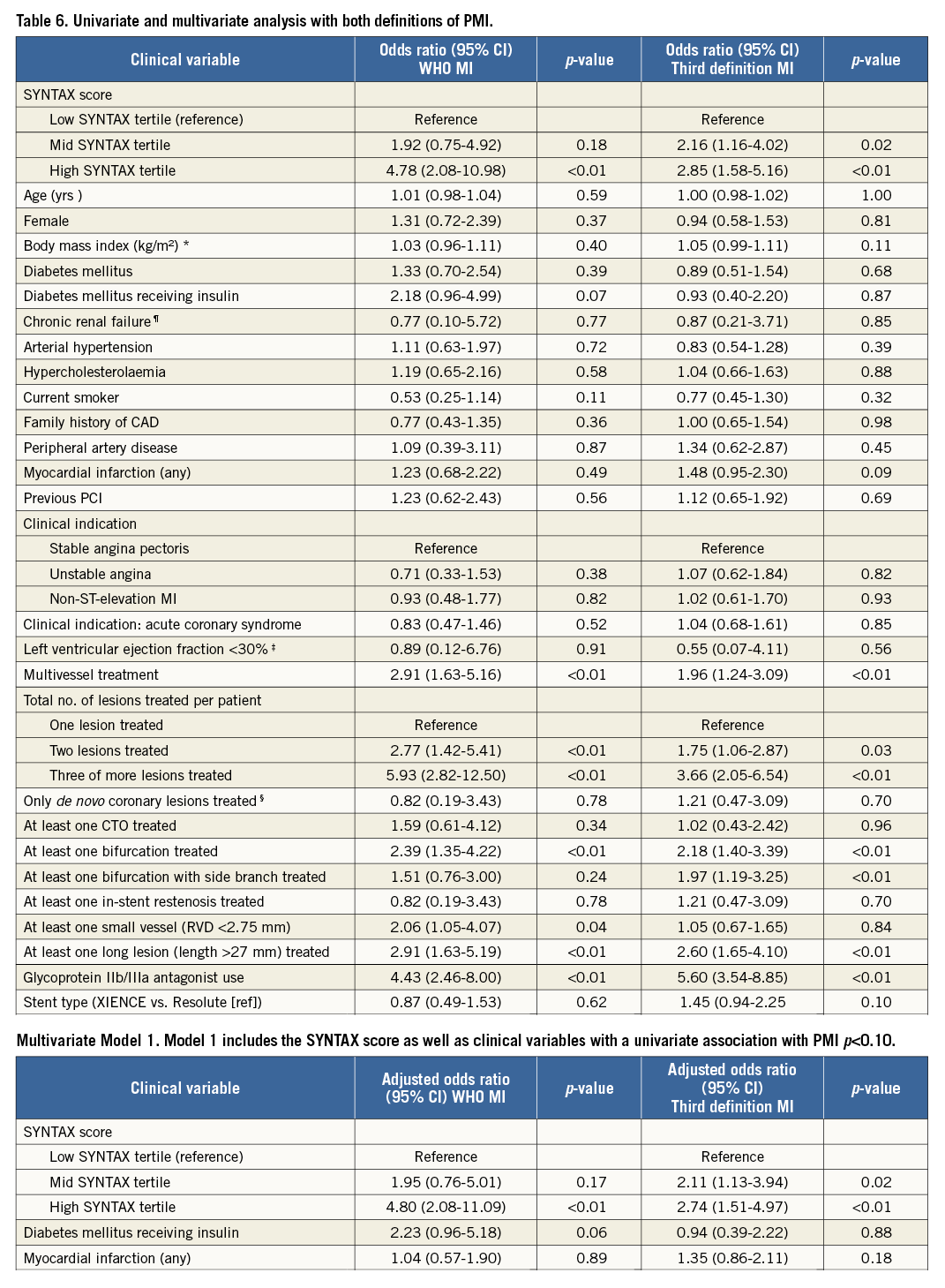
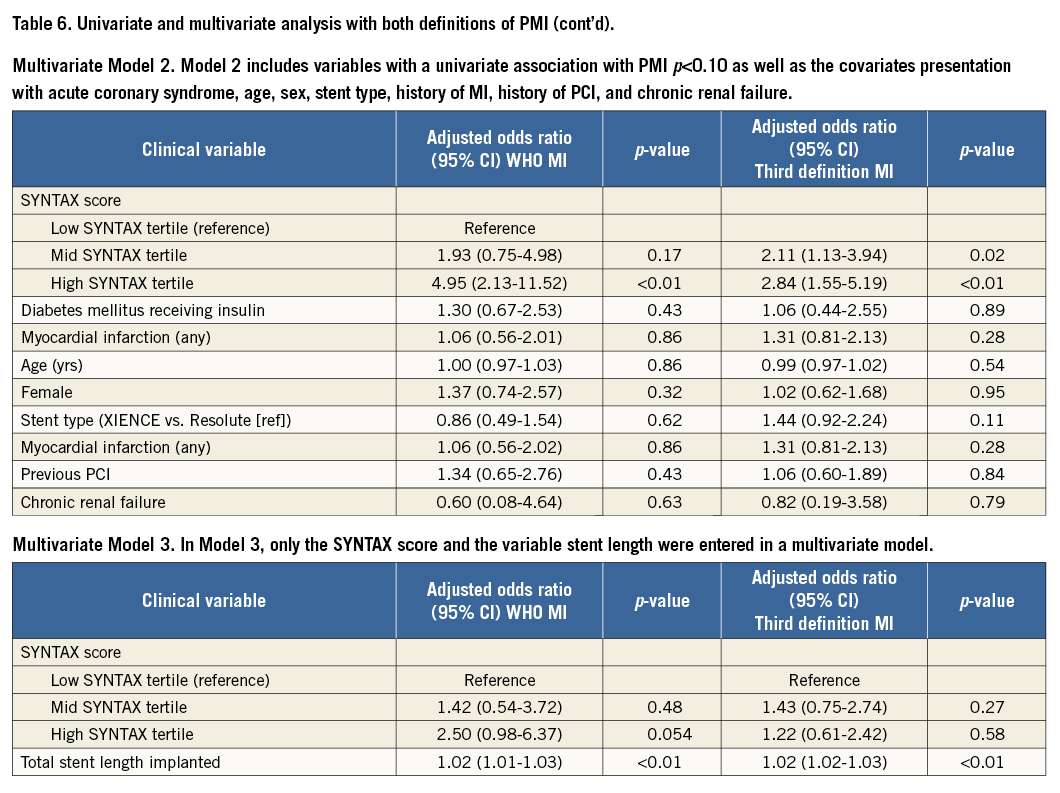
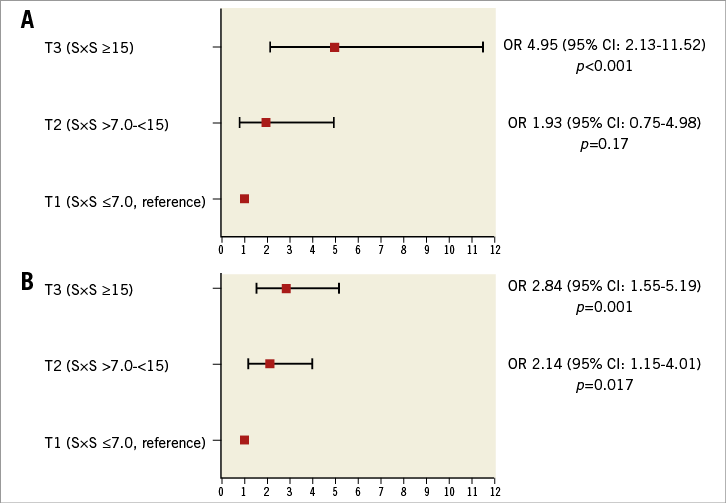
Figure 2. Multivariate adjusted odds ratios (OR) of SYNTAX score tertiles for periprocedural myocardial infarction according to the WHO definition (A), and third universal defintion of MI (B).
The full multivariate model with the SYNTAX score in it had a better correlation with PMI than the same model with the SYNTAX score being replaced by the AHA/ACC lesion classification (-2 log-likelihood of 407.6 versus 396.8). This suggests that the SYNTAX score is a better correlate of PMI.
Discussion
MAIN FINDINGS
The SYNTAX score is an independent correlate of PMI according to both the extended historical WHO definition10 and the recently updated universal definition of MI11. According to the historical WHO definition, patients with the highest tertile of the SYNTAX score, compared to the lowest tertile, had an almost five times higher risk of PMI (adjusted OR 4.95 [2.13-11.52]) and, according to the updated PMI definition, an almost three times higher risk (adjusted OR 2.84 [1.55-5.19]). Our data demonstrate that PCI patients with complex coronary artery disease have a higher PMI risk, and that the SYNTAX score correlated better to PMI than the AHA/ACC lesion classification. The present substudy of the TWENTE trial shows that the SYNTAX score independently predicts PMI in a large clinical trial with randomised data, external adjudication and core laboratory analysed data. These results are consistent with the findings from van Gaal et al who first described this relation in a registry13.
SYNTAX SCORE AND PMI
PMI is the most common adverse event after PCI and occurs in 5% to 30% of procedures, depending on patient population, local practice of post-procedural assessment of cardiac markers, and the diagnostic criteria applied14-17. Some studies have shown a relation between PMI and adverse outcome4-6.
In previous studies, the SYNTAX score has been shown to be associated with adverse long-term clinical outcome6,12,18; however, there are limited data on the value of the SYNTAX score on periprocedural complications in a broad population of patients undergoing PCI.
Van Gaal et al previously assessed 100 patients with stable coronary artery disease and suggested, based on their findings in this relatively small population, that the SYNTAX score was associated with periprocedural necrosis13. Farooq et al recently reported, in a post hoc analysis of the SYNTAX trial, that a higher SYNTAX score was associated with an increased risk of PMI in 827 patients undergoing PCI with first-generation DES (TAXUS; Boston Scientific, Marlborough, MA, USA) for severe (three-vessel or left main) coronary artery disease6.
Our study population differs significantly from both of the aforementioned studies, as 10% of our patients had a history of previous CABG, 58% presented with acute coronary syndromes, and only 24% underwent multivessel PCI19. The findings of our present study extend current knowledge by showing that, even in a broad population of contemporary PCI patients treated with second-generation DES, a higher SYNTAX score is related to an increased PMI risk.
Risk factors for PMI are associated with the burden of atherosclerotic disease (i.e., multivessel disease, calcification) and lesion complexity (i.e., thrombus formation, lesion eccentricity)20,21. These risk factors are also included in the SYNTAX score, which is a tool to assess the severity and complexity of coronary atherosclerotic disease burden. A higher SYNTAX score reflects more complex coronary artery disease, with longer lesions and/or smaller arteries which might result in higher risk for vessel dissection, side branch occlusion, no reflow or vessel occlusion causing a PMI. While numerically these causes occurred frequently in the highest SYNTAX tertile, no statistical difference was shown in the causes for PMI throughout the SYNTAX tertiles, which might have been due to the low number of events.
When the variable total stent length implanted was entered into the multivariate model, the value of the SYNTAX score as correlate for PMI was diminished, while total stent length implanted was significantly correlated with PMI. Total stent length is known to be related to lesion length, and its relation with PMI may thus be explained by the same mechanisms as previously mentioned. As the parameter lesion length is included in the SYNTAX score, collinearity may also be the reason that the value of the SYNTAX score was diminished when the variable total stent length was entered into a multivariate model.
DEFINITION OF PMI
Various clinical trials have applied different definitions of MI and PMI. In an attempt to standardise definitions, a joint European Society of Cardiology, American College of Cardiology, American Heart Association, and World Health Organization Task Force for the development of a Universal Definition of Myocardial Infarction has been established. With the development of even more sensitive assays for markers of myocardial necrosis and new insights from recent studies, the universal definition of MI has recently been updated11 to make the definition more specific. In contrast to the second universal definition of MI, higher troponin values along with supplemental clinical information are now required in order to diagnose a PMI.
In the present study, we used the extended historical WHO definition as well as the third universal definition of MI to assess a potential relation between SYNTAX score and PMI. This relation was shown for both definitions, indicating that the relation between SYNTAX score and PMI was not related to the use of one particular definition only. Nevertheless, this relation was stronger for the WHO definition of MI, which uses a higher threshold for identifying PMI.
While several previous studies have shown a relation between PMI and short-term and long-term clinical outcome6,21, there is still an ongoing discussion on this issue as other studies showed no such relation4,22,23. PMI with limited marker release may have no impact on the clinical course, which recently even triggered the suggestion of a new “clinically relevant” definition of PMI24.
IMPLICATIONS
Preprocedural assessment of the SYNTAX score could help to identify patients at an increased risk of PMI, which might then trigger preventive measures. In patients with a particularly high risk of PMI, pretreatment with drugs that have anti-inflammatory and/or antithrombotic properties might be considered, such as high-dose or early initiation of statin therapy25,26, administration of a glycoprotein IIb/IIIa antagonist27,28, and perhaps even the initiation of pharmacologic treatment for glycaemic control in patients with previously unrecognised diabetes mellitus29.
Limitations
This substudy of the TWENTE trial is limited by its post hoc nature, and the findings should be considered as hypothesis-generating only. Patients undergoing primary PCI were not included in the TWENTE trial. No data on residual SYNTAX score were available in this study.
Conclusion
In a broad population of patients treated with second-generation DES, the SYNTAX score was able to stratify the risk of periprocedural myocardial infarction according to both the WHO definition and the third universal definition of myocardial infarction.
| Impact on daily practice Several studies have shown a relation between periprocedural myocardial infarction and an unfavourable outcome. The SYNTAX score may be a useful tool for risk stratification for a periprocedural myocardial infarction, and preprocedural assessment of the SYNTAX score could help to identify patients at an increased risk of PMI, which might trigger preventive measures. |
Funding
The TWENTE trial is an investigator-initiated study, supported by equal unrestricted grants from Abbott Vascular and Medtronic. The research department of Thoraxcentrum Twente has received educational and/or research grants funded by Abbott Vascular, Biotronik, Boston Scientific, and Medtronic.
Conflict of interest statement
C. von Birgelen is a consultant to Abbott Vascular, Boston Scientific, and Medtronic; he has received a travel grant from Biotronik and lecture fees from MSD. The other authors have no conflicts of interest to declare.