Abstract
Aims: This study aimed to investigate the prognostic impact of the SYNTAX score II (SS-II) on ST-segment elevation myocardial infarction (STEMI) patients undergoing a primary percutaneous coronary intervention (pPCI).
Methods and results: This retrospective cohort study included 1,689 patients with STEMI who underwent pPCI between January 2008 and December 2016. The patients were categorised into three groups based on SS-II tertiles (SS-II low tertile <24 [n=585], SS-II intermediate tertile ≥24 and ≤34 [n=567], and SS-II high tertile >34 [n=537]). In-hospital mortality was significantly lower in patients with low and mid SS-II when compared with high SS-II (0.7% vs 0.5% vs 16.4%, p=0.001). During follow-up (median 2.35 years), a high SS-II was positively correlated with MACE (12.3% for low SS-II vs 18.3% for mid SS-II vs 43.2% for high SS-II, p=0.001), all-cause mortality (1.5% vs 3.9% vs 14.2%, p=0.001) and heart failure (0.3% vs 2.7% vs 8.2%, p=0.001). The SS-II showed additive value on top of GRACE, anatomical SYNTAX score and residual SYNTAX score.
Conclusions: The SS-II in patients with STEMI undergoing pPCI adds important prognostic information regarding midterm adverse outcomes, being an independent and powerful predictor of MACE, heart failure and all-cause mortality during follow-up.
Introduction
The SYNTAX score II (SS-II) was developed within the SYNTAX trial as a strategy to improve the ability of the anatomical (only) SYNTAX score (SS)1, by integrating relevant clinical variables (left main coronary artery disease, age, creatinine clearance, gender, left ventricular ejection fraction [LVEF], chronic obstructive pulmonary disease, and peripheral vascular disease), to identify patients with high cardiovascular risk among a population with complex artery disease, and favouring individualised decision making between coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI)2.
Patients with ST-elevation myocardial infarction (STEMI) are susceptible to significant morbidity and mortality, even when an early revascularisation strategy such as primary percutaneous coronary intervention (pPCI) is performed3. Thus, an appropriate risk stratification after pPCI is essential to estimate the short- and long-term prognosis for these patients3,4,5.
SS-II has been used as a tool for the assessment of prognostic value for outcomes of patients with stable ischaemic heart disease, multivessel or left main coronary artery disease and complex coronary artery disease, as well as for those with acute coronary syndrome with cardiogenic shock5,6,7,8,9. Nonetheless, it has not been tested in terms of long-term major adverse cardiovascular events (MACE) and all-cause mortality outcome evaluation in a population of non-selected STEMI patients undergoing pPCI.
The aim of this study was to assess the prognostic impact and clinical value of SS-II in a large cohort of real-life STEMI patients undergoing pPCI.
Methods
STUDY POPULATION
This was a single-centre, observational cohort study that enrolled consecutive patients with STEMI who underwent pPCI at the University Clinical Hospital of Santiago de Compostela between January 2008 and December 2016. A total of 1,723 patients were screened for inclusion in our study, of whom 34 were excluded, either because of unavailability of a complete coronary angiogram, or because they had a prior history of CABG or planned CABG after primary PCI, or it was not possible to follow them because they belonged to another community. Accordingly, the final cohort was composed of 1,689 patients.
Primary PCI was undertaken according to the European Society of Cardiology guidelines10,11 and operators’ routine practice.
Digitally archived diagnostic and procedural coronary angiograms were reviewed by two interventional cardiologists to calculate the anatomical SS, using an online calculator (www.syntaxscore.com).
As patients with STEMI were excluded from the SYNTAX trial12, we calculated the SS using the current algorithm, scoring the culprit lesion as a totally occluded artery (not considering the possible distal lesions), as observed before any intervention, and defined the duration of the occluded infarct artery as less than three months, as performed in studies of patients with STEMI4,13. The residual SYNTAX score (rSS) comprised the score accumulated by any untreated lesions, a value of 0 indicating complete revascularisation13.
Demographic, clinical, echocardiographic and laboratory data at admission were collected from an electronic database. Individual SS-II was calculated using the SS-II nomogram, as previously described2. To calculate SS-II, the anatomical SS was combined with the above-mentioned clinical variables2. Patients were stratified and compared according to SS-II tertiles.
DEFINITIONS
The diagnosis of STEMI was made according to current guidelines10,11. Ischaemia time was defined as the time between symptom onset and reperfusion (guidewire passage in culprit artery during pPCI). Multivessel coronary artery disease (MVD) was defined as at least one lesion in a non-infarct-related artery deemed angiographically significant (more than 50% luminal narrowing diameter). MACE during follow-up comprised all-cause mortality, myocardial infarction (MI), heart failure requiring hospitalisation and unplanned repeat revascularisation (uRR).
Heart failure (HF) was defined as the presence of signs or symptoms of congestion, mainly shortness of breath and signs of fluid retention, that are consistent with that diagnosis and led to hospitalisation. Criteria for left ventricular systolic dysfunction (LVSD) were LVEF <40% or a qualitative report of moderate or severe LVSD.
AIMS AND FOLLOW-UP
Our primary objective was to calculate the SS-II in our real-life STEMI patients who underwent pPCI and assess its clinical impact during follow-up. Additionally, we evaluated the additive prognostic value of the SS-II over control variables, SS, rSS and GRACE risk score, the latter being the preferred tool to stratify the risk of acute coronary syndrome patients and to predict their mortality.
Follow-up was carried out by consulting the electronic registries available in the autonomic community of Galicia, Spain (IANUS, the Galician Electronic Medical Record system); all medical evaluations and hospital registries were reviewed. Median follow-up was 2.35 (interquartile range 1-4.59) years.
STATISTICAL ANALYSIS
Univariate analysis of categorical variables was accomplished using the chi-square test, with results expressed as percentages, and of continuous variables using the ANOVA test, with results expressed as means±standard deviation. All variables were stratified according to the three SS-II groups. Survival curves were constructed for time-to-event variables (MACE and all-cause mortality) with Kaplan-Meier estimates.
To evaluate the additive prognostic value of SS-II (as a continuous variable), three Cox survival models were created as follows: univariate model, multivariate model using control variables that were statistically significant as predictors of events (body mass index, hypertension, diabetes, dyslipidaemia, smoking, ischaemic cardiomyopathy, ischaemia time, STEMI localisation [anterior versus other], infarct-related artery, use of drug-eluting stents, use of GP IIb/IIIa inhibitors, troponin I peak, haemoglobin, glucose, heart rate, systolic blood pressure, Killip class, CRUSADE score and medication at discharge), and multivariate models using as control variables the GRACE, SYNTAX and rSS scores separately. In order to check the robustness of the results against the temporal influence, all models were estimated considering temporal dummies. Results were also compared using the Harrell C-statistic, Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Harrell’s C-statistic is a natural extension of the receiver operating characteristic (ROC) curve which can vary between 0.5 (aleatory assignation for the different groups) and one (perfect model assignation), while AIC and BIC measure the goodness of fit and the complexity of a model (lower values translate into higher goodness of fit and lower complexity). Models with a higher Harrell C-statistic and lower AIC and BIC are preferred. To evaluate the additional prognostic value of SS-II on top of GRACE, the increase of the area under the ROC curve and the net reclassification improvement (NRI) were calculated in a logit model. NRI indicates the number of patients who are reclassified after adding SS-II to the model. All analyses were two-tailed, and differences were considered significant if the p-value was <0.05. The statistical analysis was performed using SPSS, Version 22.0 (IBM Corp., Armonk, NY, USA) and Stata 13.0 (StataCorp, College Station, TX, USA).
Results
BASELINE CHARACTERISTICS
The cohort was composed of 1,689 patients with STEMI who underwent pPCI as the invasive management strategy and was divided into three groups determined by SS-II: the low-tertile group: <24 (n=585, 34.6%), the intermediate-tertile group: ≥24 and <34 (n=567, 33.5%), and the high-tertile group: ≥34 (n=537, 31.7%). Amongst the total cohort, the mean SS-II was 30.43 and the median SS-II 28.1.
We compared the baseline characteristics according to the three SS-II groups. The results are shown in Table 1. Male gender was more frequent in the low and intermediate SS-II tertiles. Patients in the high SS-II tertile were older and had a significantly higher prevalence of hypertension, diabetes mellitus 2, history of ischaemic heart disease and MVD (p=<0.001); interestingly, however, fewer smokers were found in this group. The left anterior descending artery (LAD) was the most frequent infarct-related artery (IRA) for the high SS-II tertile group, and the left main (LM) was involved in 2.24% of patients in this group. Mean ischaemia time before PCI was 275 minutes, with no statistical difference among groups. The average number of patients in Killip class IV was 18.4% for the high-tertile group, and 1.54% for the low-tertile group. Mean glomerular filtration rate (GFR) in the high SS-II group was 57 mL/min.
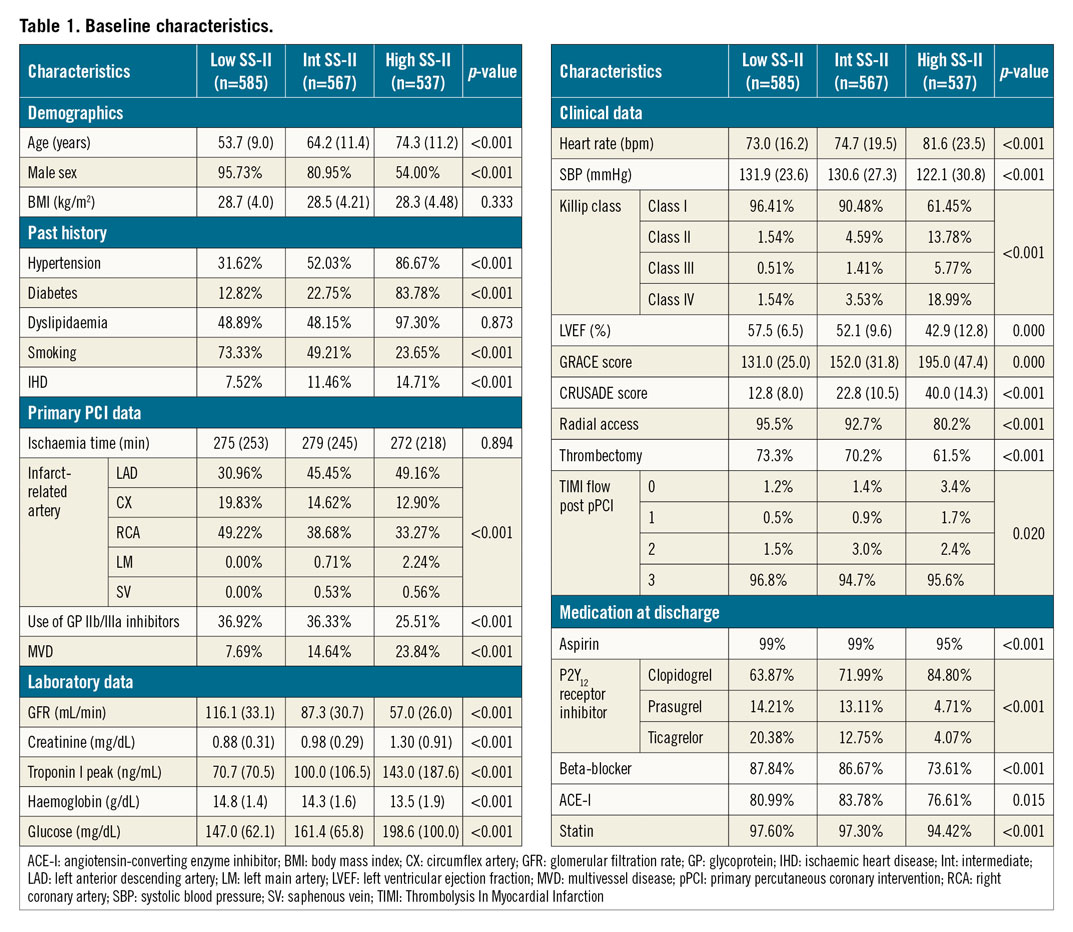
Clopidogrel was more frequently used in patients with high SS-II, whilst ticagrelor and prasugrel were more frequently used in low SS-II patients.
CLINICAL OUTCOMES
The clinical adverse events during follow-up are displayed in Table 2. In-hospital mortality was significantly higher in patients in the high SS-II tertile group when compared with the SS-II intermediate and low tertile groups (16.4% vs 0.5% vs 0.7%, p=<0.001). During follow-up, the MACE-free survival rate was positively correlated with the SS-II, with the highest MACE-free survival rate in the low SS-II tertile group and the lowest MACE-free rate in the high SS-II tertile group (87.7% vs 81.7% vs 56.8%; p=<0.001) (Figure 1). All-cause mortality was significantly higher in the high SS-II tertile group compared with the intermediate and low tertile groups (14.2% vs 3.9% vs 1.5%, p=<0.001) (Figure 2). HF during follow-up was significantly higher in the high SS-II tertile group compared to the intermediate and low tertile groups (8.2% vs 2.7% vs 0.3%, p=<0.001). Nonetheless, the rates of MI and uRR during follow-up were not different among the groups (4.5% vs 4.6% vs 3.9%, p=0.844, and 7.1% vs 6.5% vs 7.0%, p=0.923, respectively). Stent thrombosis during follow-up was also higher in the high SS-II tertile group compared with the intermediate and low tertile groups (1.2% vs 1.4% vs 3%, p<0.001).
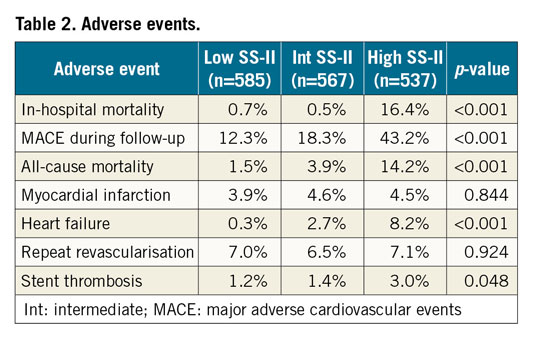
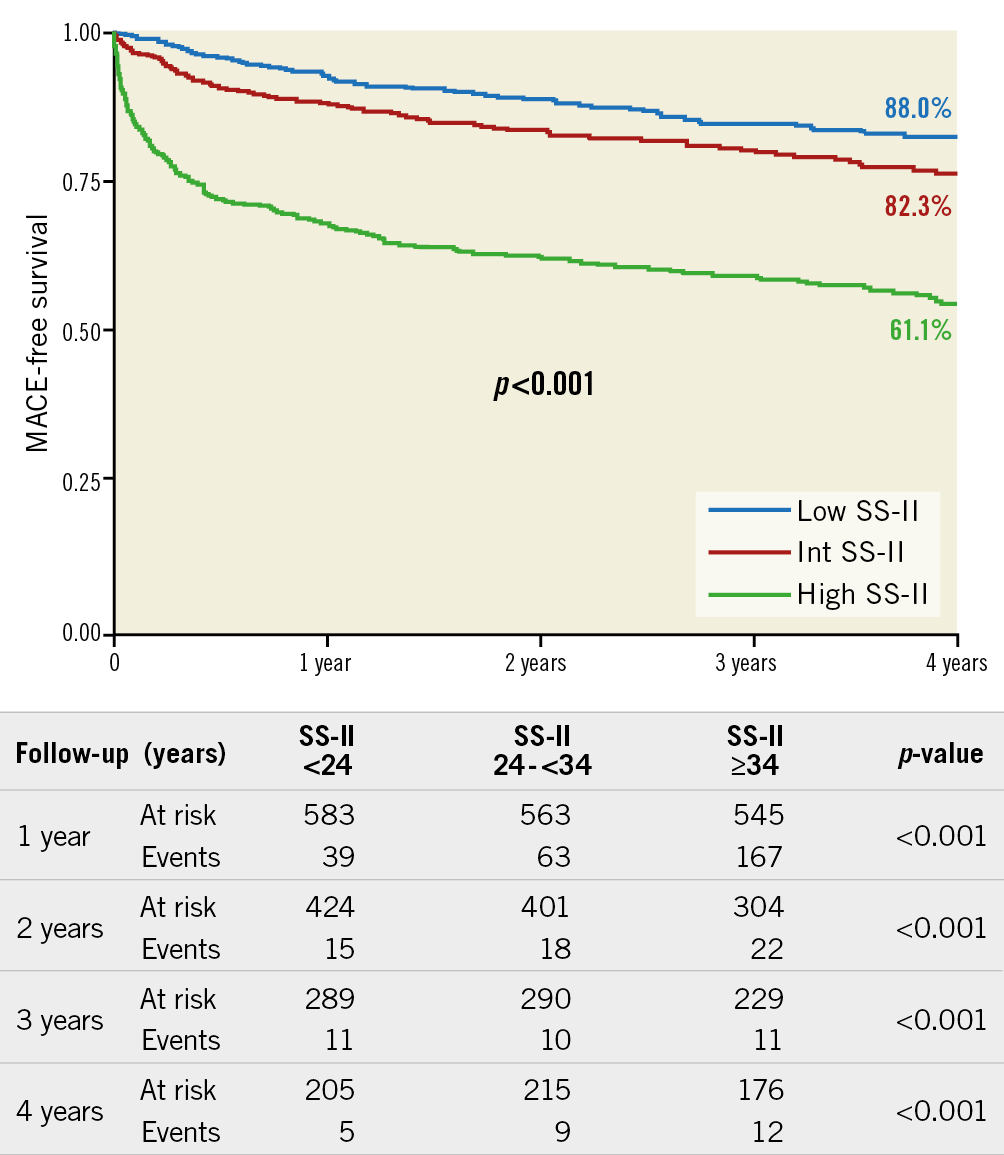
Figure 1. Kaplan-Meier curves for MACE. MACE: major adverse cardiovascular events
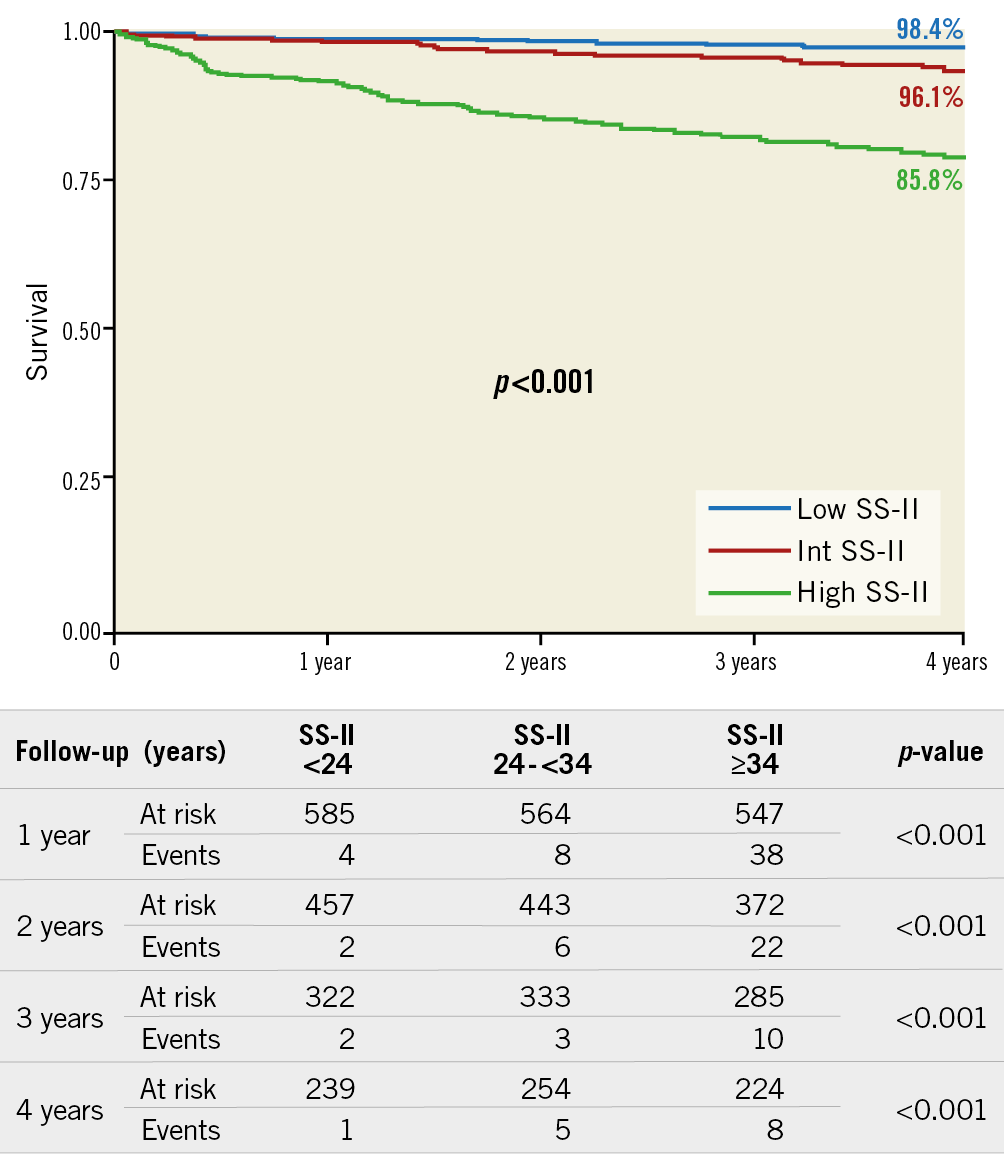
Figure 2. Kaplan-Meier curves for all-cause mortality.
ADDITIVE VALUE OF SS-II
The Cox survival models for MACE and all-cause mortality are depicted in Table 3. In our population, the SS-II was also an independent predictor of MACE and all-cause mortality during follow-up, adding prognostic value over control variables and GRACE, anatomical SS and rSS. Additional independent predictor variables for mortality were heart rate, smoking, Killip class, diabetes mellitus, haemoglobin on admission, beta-blockers and ACE inhibitors at discharge and stent type. Models that consider SS-II are preferred according to the C-statistic, AIC and BIC values. When compared with patients with a low SS-II, intermediate-risk and high-risk SS-II patients have a 2.5 and 10.5 times higher risk of MACE, respectively. Regarding all-cause mortality, intermediate-risk and high-risk SS-II patients have a 1.496 and 4.041 times higher risk of an event compared to the low-risk SS-II group.
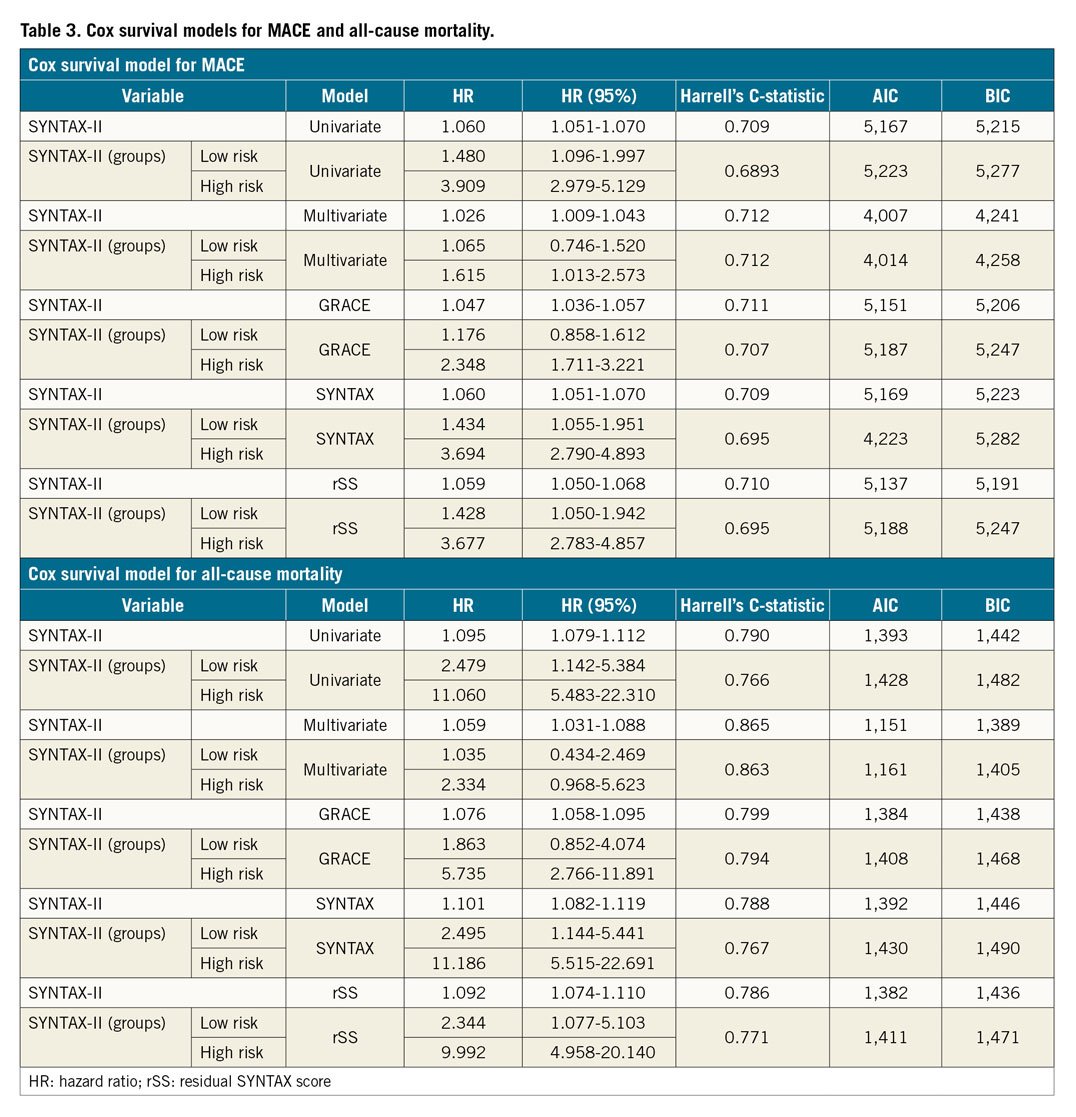
The additive value of SS-II on top of GRACE, SS and rSS is also supported by the increase of the area under the ROC curve (Figure 3) and the correct reclassification of patients after the addition of SS-II to GRACE, anatomical SS and rSS regarding in-hospital mortality, MACE, all-cause mortality and the development of HF during follow-up (Supplementary Table 1-Supplementary Table 3).
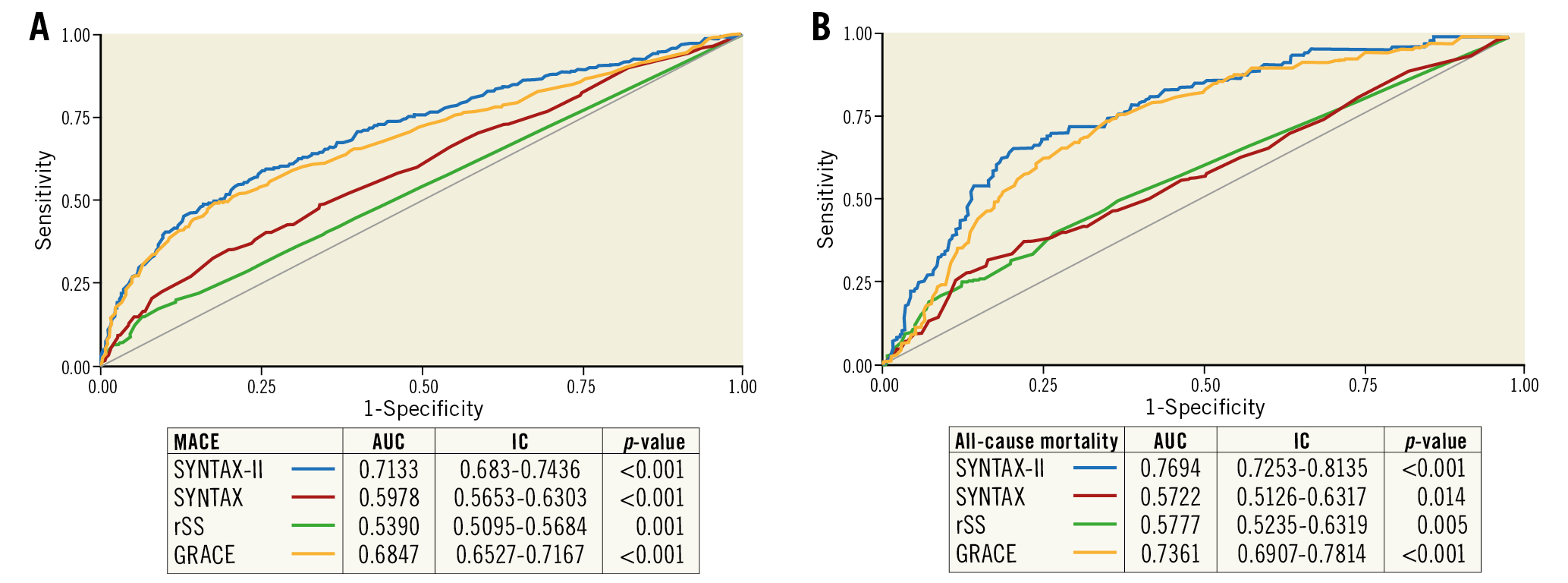
Figure 3. ROC curves for MACE and all-cause mortality. A) MACE. B) All-cause mortality. MACE: major adverse cardiovascular events
Discussion
In this study, we aimed to assess the midterm prognostic value of the SS-II in a real-life population of consecutive patients with STEMI who underwent pPCI. The main findings are the following: 1) a high SS-II was associated with adverse outcomes in STEMI patients after pPCI; 2) SS-II was shown to be a strong independent predictor of midterm all-cause mortality, MACE and HF, but not of MI or uRR; 3) SS-II adds prognostic value on top of the traditional GRACE score, anatomical SYNTAX score and residual SYNTAX score.
Risk stratification in patients with STEMI is a major feature in real clinical practice, as it provides a broad perspective of patient outcomes based on patient characteristics and optimal treatment. In this regard, plenty of clinical risk scores for determining prognosis in STEMI patients, such as the GRACE risk score, TIMI score, PAMI score, Zwolle risk score, CADILLAC score, ALPHA score14,15,16,17,18,19 have been tested to provide an optimal management. The GRACE risk score is considered the most robust score for evaluating the risk in patients with STEMI/NSTEMI at initial presentation14, although it is a classic score which was developed in an era of less effective pharmacological and interventional treatment and it does not consider the impact of the angiographic severity of the disease, the history of peripheral vascular disease and the effect of pulmonary disease on cardiovascular outcomes. In our study, the SS-II was demonstrated to add prognostic value for all-cause mortality and MACE better than a clinical score such as the GRACE risk score.
The SYNTAX score II considers angiographic and clinical variables, which are widely known to affect long-term outcomes of PCI2. The SS-II has been tested in different challenging clinical scenarios such as in complex coronary artery disease (CAD) in patients undergoing PCI6, where it was superior to the anatomical SS in predicting two-year mortality. In acute coronary syndromes with severe CAD, the SS-II has proved to be a good tool for predicting MACE after one-year follow-up. A single study has assessed the prognostic ability of SS-II in a real-life STEMI population of 477 patients undergoing pPCI with a one-year follow-up. It did not show superiority to other scores in predicting MACE, but it did in predicting target vessel revascularisation (TVR) after pPCI20. Our study is the first to show a long-term prognostic value for SS-II in terms of all-cause mortality and MACE in a cohort of a significant number of patients; nonetheless, it did not show any difference in ischaemic soft outcomes such as MI and repeat revascularisation, probably due to the high index of complete revascularisation among MVD patients.
The anatomical SYNTAX score has proved to be useful in the risk stratification of non-STEMI and STEMI patients who underwent urgent PCI as an independent predictor of mortality, MACE, and stent thrombosis up to one-year follow-up, albeit the ability of this score would have been reinforced by adding a combination of angiographical and clinical variables1,4,21,22. On the other hand, the rSS showed it was also an independent predictor of MACE and all-cause mortality during follow-up (OR 2.9 for reasonable incomplete and 3.9 for incomplete revascularisation), adding prognostic value over control variables and GRACE13. In our study, the SS-II improved the predictive accuracy of long-term all-cause mortality, MACE and HF when compared with the anatomical SYNTAX score and the residual SYNTAX score, demonstrating that the addition of clinical variables to purely angiographic scores enables better prediction of the long-term prognosis of the patients with STEMI undergoing pPCI. Nonetheless, the rate of MI and uRR during follow-up was not different between groups.
In addition, our study provides important information regarding the prediction of developing HF after a pPCI. This is a very relevant issue since HF after a STEMI event has been shown to be a predictor of late mortality even after successful revascularisation23. In our total cohort, 17% of patients were classified as Killip class II to IV at the time of presentation, of whom 12.6% were in the high SS-II tertile group. Of this group, 6.4% of patients developed HF in the first year, with a yearly downward trend to 0.6% after four years. HF has been shown to have a significant impact in patients after an acute coronary syndrome (ACS)3 or after a pPCI24; nevertheless, HF has not been properly assessed among real-life cohorts after a STEMI and pPCI. None of the trials assessing the anatomical SYNTAX score, or the residual SS in this set of patients, has provided information on predicting the development of HF4,13. Other MI trials have focused predominantly on thrombosis, bleeding and MACE, rather than HF events specifically25.
In our study, the SS-II improved the predictive accuracy of intermediate-term all-cause mortality, MACE and HF when compared with the anatomical SYNTAX score, the residual SYNTAX score and the GRACE risk score. Analysing the results, we consider that the strongest characteristic of the SS-II is the integration of the anatomical characteristics of the SYNTAX score and clinical variables.
Although it is necessary to analyse the anatomical coronary lesions to obtain the SS-II score, it provides a good stratification profile that makes it worth employing on a routine basis.
Limitations
This was a retrospective observational and non-randomised study conducted at a single hospital and, as such, has the inherent limitations and bias related to retrospective single-centre studies. Interpretation of angiograms and assessment of the SS were not adjudicated by a core laboratory; although each interventional cardiologist was experienced and well trained to calculate this score, different results might have been obtained if they had been carried out by consensus. We did not collect data on functional assessment of coronary stenosis in patients who underwent multivessel PCI; it is likely that in most patients the assessment of non-culprit lesion significance was made only on coronary angiography.
Conclusions
The present study shows that the SS-II in patients with STEMI undergoing pPCI adds important prognostic information regarding intermediate-term adverse outcomes, being an independent and powerful predictor of MACE, heart failure and all-cause mortality during follow-up.
|
Impact on daily practice Risk stratification in patients with STEMI is a major feature in real clinical practice, as it provides a broad perspective of patient outcomes based on patient characteristics and optimal treatment. Our results may have several clinical implications and implications for the health-system organisation. We describe for the first time the intermediate-term prognostic value of SS-II in terms of all-cause mortality and MACE from a large, contemporary real-world cohort of STEMI patients submitted to pPCI. Our results also suggest that this score may be used for improvements in the “network care system” for STEMI patients, with implications for risk stratification and hospital and long-term care organisation. |
Conflict of interest statement
The authors have no conflicts of interest to declare.