Abstract
Aims: The SYNTAX Score (SXscore) has established itself as an important prognostic tool in patients undergoing percutaneous coronary intervention (PCI). A limitation of the SXscore is the inability to differentiate outcomes in patients who have undergone prior coronary artery bypass graft (CABG) surgery. The CABG SXscore was devised to address this limitation.
Methods and results: In the SYNTAX-LE MANS substudy 115 patients with unprotected left main coronary artery disease (isolated or associated with one, two or three-vessel disease) treated with CABG were prospectively assigned to undergo a 15-month coronary angiogram. An independent core laboratory analysed the baseline SXscore prior to CABG. The 15-month CABG SXscore was calculated by a panel of three interventional cardiologists. The CABG SXscore was calculated by determining the standard SXscore in the “native” coronary vessels (“native SXscore”) and deducting points based on the importance of the diseased coronary artery segment (Leaman score) that have a functioning bypass graft anastomosed distally. Points relating to intrinsic coronary disease, such as bifurcation disease or calcification, remain unaltered. The mean 15-month CABG SXscore was significantly lower compared to the mean baseline SXscore (baseline SXscore 31.6, SD 13.1; 15-month CABG SXscore 21.2, SD 11.1; p<0.001). Reproducibility analyses (kappa [k] statistics) indicated a substantial agreement between CABG SXscore measurements (k=0.70; 95% CI [0.50-0.90], p<0.001), with the points deducted to calculate the CABG SXscore the most reproducible measurement (k=0.74; 95% CI [0.53-0.95], p<0.001). Despite the limited power of the study, four-year outcome data (Kaplan-Meier curves) demonstrated a trend towards reduced all-cause death (9.1% vs. 1.8%, p=0.084) and death/CVA/MI (16.4% vs. 7.0%, p=0.126) in the low compared to the high CABG SXscore group.
Conclusions: In this pilot study the calculation of the CABG SXscore appeared feasible, reproducible and may have a long-term prognostic role in patients with complex coronary disease undergoing surgical revascularisation. Validation of this new scoring methodology is required.
Introduction
The SYNTAX Score (SXscore) (http://www.syntaxscore.com)1-5 has established itself as an important prognostic tool in risk stratifying patients being considered for revascularisation, and has been validated in patients undergoing percutaneous coronary intervention (PCI) at one-year follow-up6-11. In addition, the SXscore has been applied to contemporary drug-eluting stent trials enrolling “all-comers” type populations, and has been shown to be an independent predictor of one-year mortality and major adverse cardiac events (MACE)12-14.
As a consequence, the SXscore is now advocated in both the European and the US revascularisation guidelines in aiding the risk stratification of patients with complex coronary artery disease to the most appropriate revascularisation modality15-17. Furthermore, the US FDA (Food and Drug Administration) recommends the application of the SXscore in selecting low-intermediate SXscore patients with unprotected left main coronary artery disease in the ongoing EXCEL Trial (ClinicalTrials.gov Identifier: NCT01205776), and low SXscore patients suitable for transcatheter aortic valve implantation in the SURTAVI Trial (ClinicalTrials.gov Identifier: NCT01586910). However, a limitation of the SXscore is the inability to apply it usefully to patients who have previously undergone CABG.
Based on the principles first defined by Leaman et al (Leaman score)18, the SXscore takes into account both the coronary anatomy and also the importance of the diseased coronary artery segment supplying the myocardium –termed “vessel-segment weighting”. Although the baseline SXscore, calculated prior to surgical revascularisation, has been shown not to have any effect on the short to long-term prognosis after CABG3,4,7,19,20, it was hypothesised that a suitably developed CABG SXscore that takes into account native coronary disease anatomy, including features such as calcification, bifurcation disease and the effects of surgical revascularisation on the vessel-segment weighting, may have potential clinical and research applications. The purpose of this pilot study is to examine the feasibility of the newly developed CABG SXscore in the SYNTAX-LE MANS angiographic substudy21.
Methods
The overall study design of the all-comers SYNTAX Trial3,5,22 and the SYNTAX-LE MANS substudy21 have previously been described. In brief, SYNTAX-LE MANS was a predefined substudy of patients from the randomised SYNTAX Trial who provided a separate written, informed consent for the substudy entry21. Eligible patients were those with left main disease (isolated or associated with one, two or three-vessel disease) who did not have renal dysfunction (defined as creatinine >2.0 mg/dL [150 μmol/L]) or hypersensitivity to contrast agents that could not be adequately premedicated. Per protocol, the time window for the 15-month angiogram was set between 14 and 16 months post-allocation. Patients enrolled in the study who had a clinically driven angiogram from 9 to 13 months (inclusive) after treatment allocation were permitted to use the earlier coronary angiogram to fulfil the 15-month angiographic requirement.
CABG SYNTAX SCORE ANALYSIS
Baseline and 15-month coronary angiograms were analysed side by side by a panel of three interventional cardiologists to calculate the 15-month CABG SXscore. All reviewers were blinded to the clinical outcomes of the patient analyses and to the baseline SXscore, undertaken prior to CABG by an independent core laboratory (Cardialysis BV, Rotterdam, The Netherlands) as part of the original SYNTAX Trial3.
The CABG SXscore calculation was repeated on 30 randomly selected cases at a three-month interval with the reviewers blinded to the original baseline and CABG SXscores. Intraobserver reproducibility analyses were undertaken.
CABG SYNTAX SCORE
The CABG SXscore is essentially the SXscore of the “native” coronary vessels (“native SXscore”), with points deducted based on the vessel-segment weighting of the bypassed coronary vessel as previously proposed by Leaman et al18.
SYNTAX SCORE
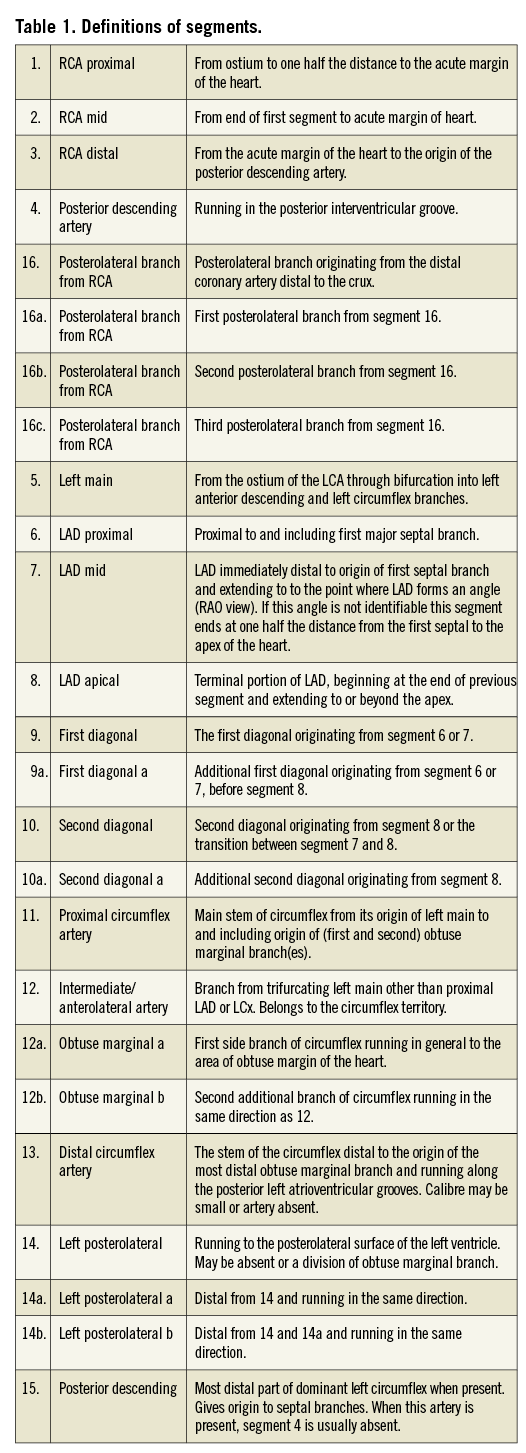
In brief, the SXscore1-4 was developed by combining the importance of a diseased coronary artery segment by the vessel-segment weighting (Leaman score)18, adverse characteristics of such a lesion for revascularisation (ACC/AHA lesion classification)23,24 and the Medina classification system for bifurcation lesions25. Each vessel segment, 1.5 mm in diameter or greater (Figure 1, labelled 1 to 16), with a ≥50% diameter stenosis by visual estimation, is awarded a multiplication factor related to coronary lesion location and severity (Figure 2). Further characterisation of the coronary lesions leads to the addition of more points, which includes features of total occlusions (duration, length, blunt stump, presence of bridging collaterals or side branch), presence of bifurcation (based on the Medina classification) or trifurcation disease (number of diseased branches involved), side branch angulation, aorto-ostial lesion, severe tortuosity, lesion length >20 mm, heavy calcification, thrombus and diffuse or small vessel disease. An online SXscore algorithm1 automatically summates each of these features to calculate the final total SXscore.
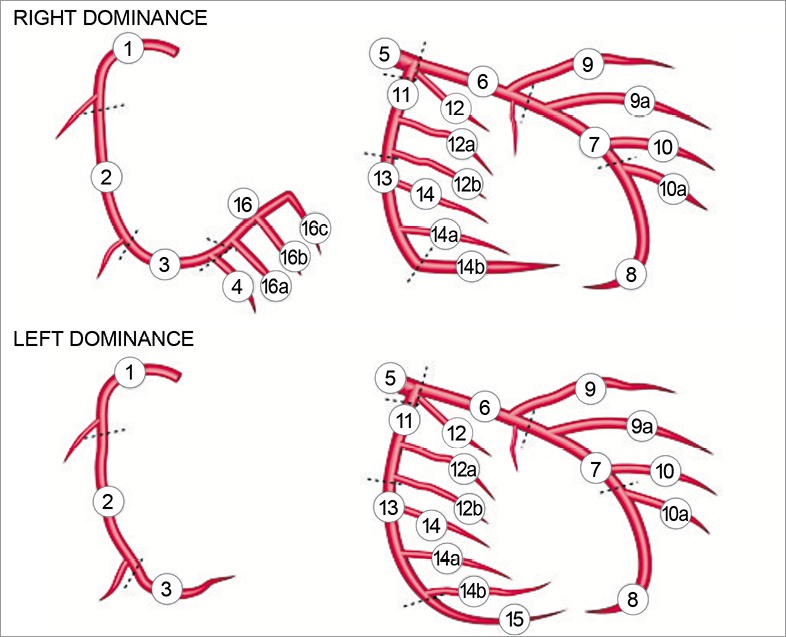
Figure 1. The effect of right and left arterial dominance on the segment numbering – refer to Table 1 for the segment-weighting for the respective arterial segments. Anatomical description of the segment numbers has previously been described2 and is included in the supplementary appendix.
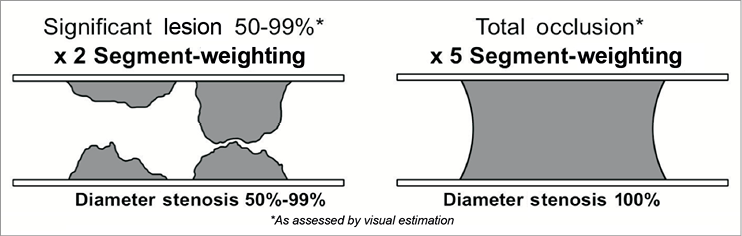
Figure 2. Segment-weighting multiplication factors utilised in the SYNTAX Score – used to calculate the points required to deduct from the “native SXscore” to calculate the CABG SYNTAX Score.
LEAMAN SCORE
The Leaman score is based on the severity of luminal diameter narrowing, and is weighted according to the usual blood flow to the left ventricle (LV) in each vessel or vessel segment based on whether the coronary system is right or left dominant18.
In a right dominant system the right coronary artery (RCA) supplies approximately 16% and the left coronary artery (LCA) approximately 84% of the blood flow to the LV. This 84% is normally directed 66% to the left anterior descending (LAD) and 33% to the left circumflex (LCx) vessels. Thus the LAD and LCx respectively carry approximately 3.5 times and 1.5 times as much blood as the RCA. In a left dominant system the LV receives all of its blood supply from the LCA; consequently, the RCA is not weighted and its value is assigned to the LCA, thereby leading to a heavier vessel-segment weighting of the LAD and LCx compared to a right dominant system18,26-28. These principles ultimately formed the basis of the segment-weighting factors that were incorporated into the SXscore (Table 1)1-4.
CALCULATION OF THE CABG SYNTAX SCORE
In order to allow consistency and reproducibility in the application of the CABG SXscore, five rules were adhered to in calculating the CABG SXscore.
1. The SXscore of the native coronary vessels (native SXscore) was analysed using the standard methodology (http://www.syntaxscore.com)1, utilising the bypass graft angiogram as necessary to allow visualisation of the entire vessel.
2. All the bypass grafts were analysed to establish the vessel-segment weighting of the “protection” conferred by the bypass grafts (Figure 1, Table 1).
3. Based on the presence of obstructive or non-obstructive bypass disease by visual assessment, segment-weighting points were deducted from the native SXscore:
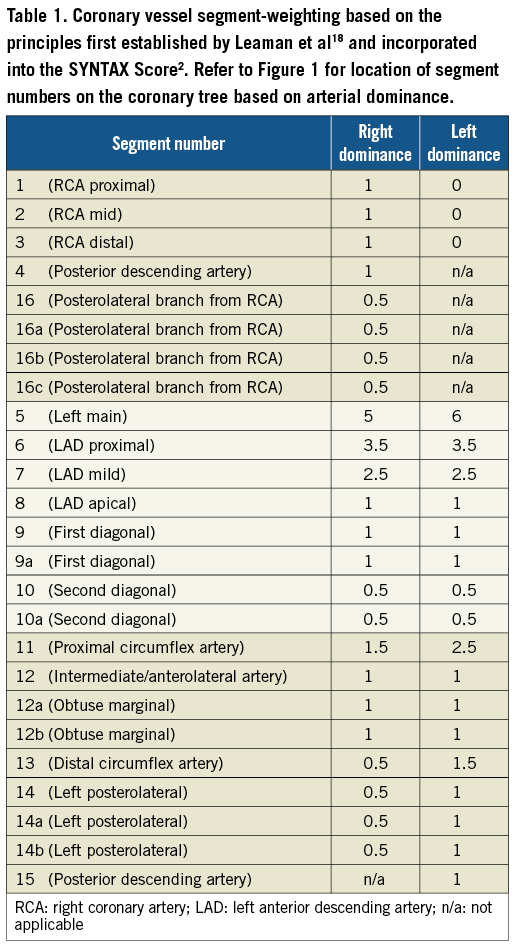
a. Patent bypass graft to a significant coronary lesion: segment-weighting points for the coronary lesion were deducted, provided there was no intervening significant coronary disease (Figure 3).
b. Occluded bypass graft: native SXscore remained unaltered (Figure 3).
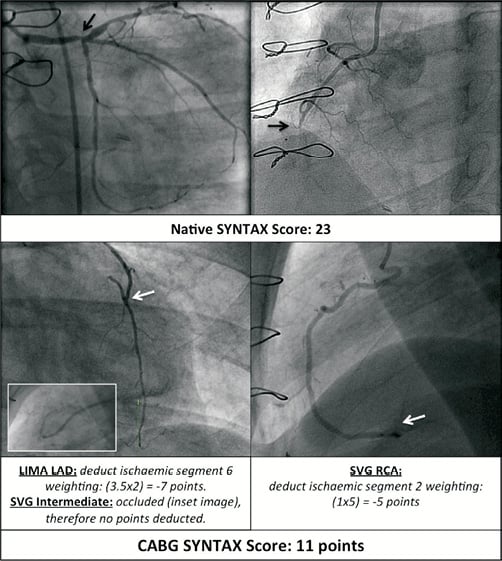
Figure 3. Example of the calculation of the CABG SXscore in a patient with distal left main trifurcation disease and an occluded mid RCA. The native SXscore was 23 (upper images). A patent LIMA to the LAD with no intervening obstructive coronary disease (lower left image) led to the deduction of 3.5×2 points (x2 segment-weighting due to ischaemic LAD) from the native SXscore. An occluded SVG to the intermediate led to no points being deducted (inset lower left image). A patent SVG to the distal RCA led to 1×5 points (x5 segment-weighting due to occluded mid RCA) deducted from the native SXscore. Final CABG SXscore was therefore 23-7-5=11 points. LIMA: left internal mammary artery; SVG: saphenous vein graft; RCA: right coronary artery. Black arrows indicate obstructive native coronary disease; white arrows indicate patent anastomosis sites of grafts to vessels
c. Bypass graft with obstructive (50-99%) disease (Figure 4):
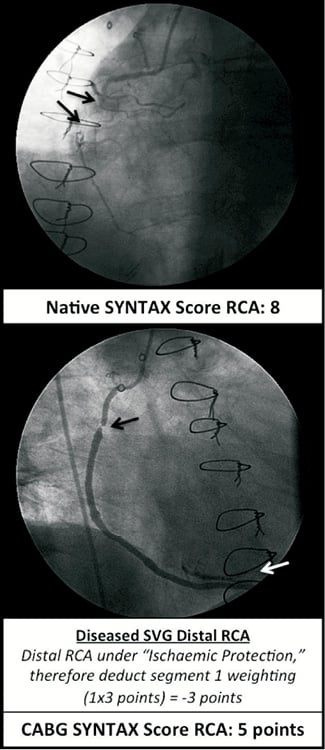
Figure 4. Principle of “ischaemic protection” in the CABG SXscore. Upper image: occluded mid RCA (segment 2 - black arrows) with bridging collaterals: native SXscore for the RCA is 8. Lower image: SVG anastomosed to distal RCA (white arrow). If the SVG was free of obstructive disease then the CABG SXscore would be 8 minus (1×5)=3 points. If the SVG was diseased with an obstructive lesion as illustrated (lower image, black arrow) the distal RCA would be under “ischaemic protection”. Consequently x2 weighting factor for the RCA should remain – therefore x3 weighting needs to be deducted leading to a CABG SXscore of 8 minus (1×3) points=5 points. If the SVG was occluded then the CABG SXscore would remain unaltered at 8 points. RCA: right coronary artery; SVG: saphenous vein graft
i. obstructive native coronary lesion (50-99%): no segment-weighting points deducted;
ii. occluded native coronary lesion (100%, TIMI 0 flow): x3 segment-weighting points deducted.
With an obstructive native coronary lesion (50-99%), it is assumed that a significantly diseased graft (50-99%) would confer no additional benefit to the blood supply to the affected coronary vessel; consequently, there would be no net gain or loss in the segment-weighting points to the native SXscore. Conversely, if the coronary vessel was occluded, then a diseased graft (50-99%) would provide “ischaemic protection” to the territory supplied by the occluded lesion. Consequently, the segment-weighting factor would be reduced from x5 (occluded vessel) to x2 (non-occluded vessel with a significant lesion [50-99%]), i.e., a deduction of x3 segment-weighting factor from the native SXscore.
4. Any further native coronary disease clearly identified through the angiograms of the bypass grafts were added to the native SXscore. Lesions ≥3 reference vessel diameters were viewed as two separate lesions and within this distance as one lesion.
5. If an obstructive coronary lesion interferes with the blood flow to the vessel being protected by the bypass graft, then the points deducted were for the segment weighting of the lesion only (Figure 5).
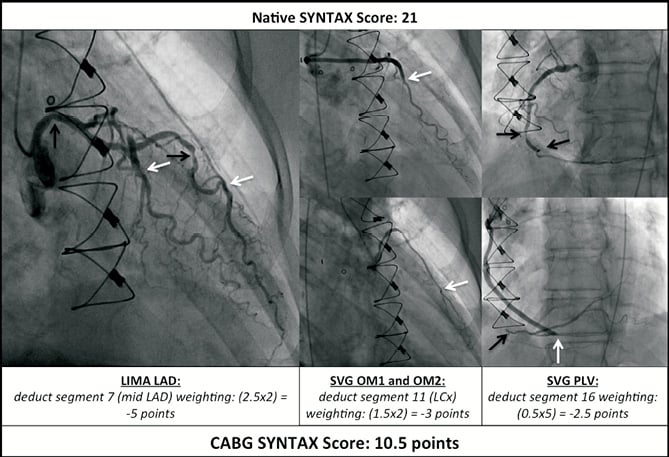
Figure 5. Example of the calculation of the CABG SXscore in a patient with mid left main and two-vessel coronary disease. Native SXscore was 21. A patent LIMA anastomosed to the mid LAD, with upstream native mid LAD disease, and led to the segment-weighting (2.5×2 points) of the mid LAD (segment 7) being deducted from the native SXscore (left image). The LCx was protected by two OM SVGs leading to a deduction of 1.5×2 points from the native SXscore (middle image). The occluded PLV was protected by an SVG leading to the deduction of 0.5×5 points from the native SXscore (right image). Final CABG SXscore was therefore 21-5-3-2.5=10.5 points. LAD: left anterior descending artery; LCx: left circumflex; OM: obtuse marginal; RCA: right coronary artery; PLV: posterior left ventricular branch of the RCA; LIMA: left internal mammary artery; SVG saphenous vein graft. Black arrows indicate obstructive native coronary disease; white arrows indicate patent anastomosis sites of grafts to vessels.
Points related to the lesion characteristics of the “native” coronary disease, such as calcification, bifurcation disease, total occlusion, etc., would remain unaltered as these reflect the native coronary anatomy. Further detail on the SXscore/Leaman score and applications of the CABG SXscore are provided in the Supplementary Appendix.
STATISTICAL ANALYSIS
Continuous variables are expressed as means±SD. Comparisons of means and four-year outcomes (Kaplan-Meier curves) were performed with the paired t-test and log-rank test respectively. Intraobserver variability (tertile partitioning) was determined with kappa statistics (<0 none, 0-0.20 slight, 0.21-0.40 fair, 0.41-0.60 moderate, 0.61-0.80 substantial, 0.81-1.00 almost perfect) on the native SXscore, deducted points and CABG SXscore4. A two-sided p-value <0.05 was considered significant for all tests. Analyses were conducted with SAS System Software Version 8.0+ (SAS Institute, Cary, NC, USA) and SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
Results
In total, 271 patients were enrolled in the SYNTAX-LE MANS study, 115 of whom were enrolled in the CABG arm. Available 15-month coronary angiograms were suitable for analysis in 113 of 115 (97.4%) CABG patients. No patients died in the CABG arm from baseline to undergoing the 15-month coronary angiogram. One patient had no angiographic films available and a further patient did not have native coronary vessels filmed. Baseline characteristics for the SYNTAX-LE MANS substudy have been published previously21.
COMPARISONS OF THE BASELINE SYNTAX SCORE AND 15-MONTH CABG SYNTAX SCORE
Comparisons of the baseline SXscores and 15-month CABG SXscores demonstrated a significant decline in the mean value of the 15-month CABG SXscores (Figure 6). Both the baseline SXscore and the 15-month CABG SXscore appeared to be broadly normally distributed with the mean 15-month CABG SXscore significantly moved to the left (Figure 7). The mean 15-month CABG SXscore was significantly lower compared to the mean baseline SXscore (baseline SXscore 31.6, SD 13.1; 15-month CABG SXscore 21.2, SD 11.1; p<0.001) (Figure 7).
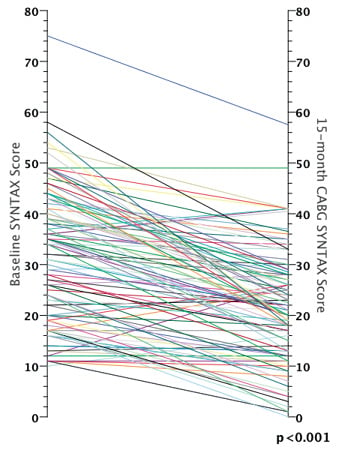
Figure 6. Reduction in the CABG SYNTAX Score at scheduled coronary angiography at 15 months, compared to the baseline SYNTAX Score (n=113).
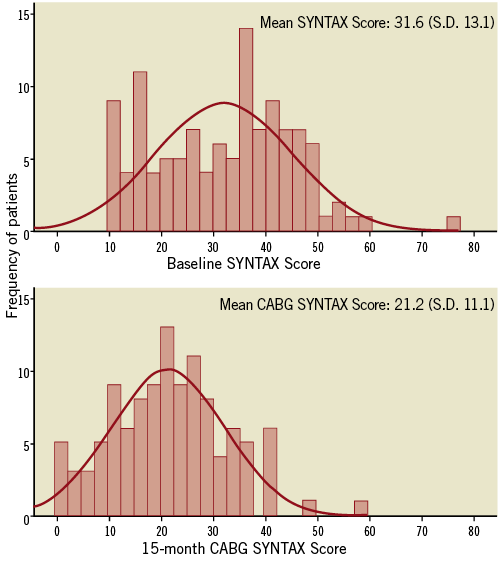
Figure 7. Distribution of the baseline SYNTAX Scores and the 15-month CABG SYNTAX Scores (n=113). Note the significant decrease in the mean CABG SYNTAX Score compared to the mean baseline SYNTAX Score (p<0.001). SD: standard deviation.
Comparisons of the baseline SXscore and 15-month native SXscore did not demonstrate any significant statistical differences (baseline SXscore 31.6, SD 13.1; 15-month native SXscore 31.1, SD 12.2; p=0.50). The mean number of points deducted from the 15-month native SXscore to derive the CABG SXscore was 9.9 (SD 5.3) (Figure 8).
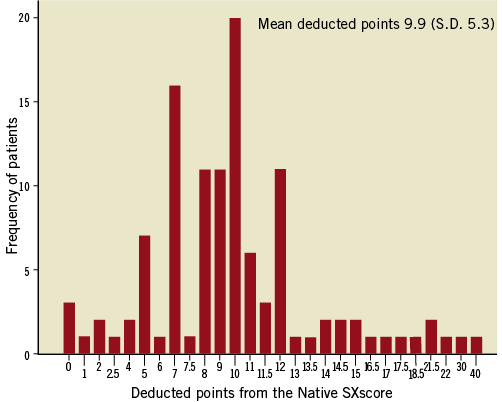
Figure 8. Distribution of the deducted points from the native SXscore to calculate the CABG SXscore (n=113). SD: standard deviation.
REPRODUCIBILITY ANALYSES
The intraobserver variability for the 15-month native SXscore (k=0.70; 95% CI: 0.50-0.91, p<0.001), points deducted from the native SXscore to derive the 15-month CABG SXscore (k=0.74; 95% CI: 0.53-0.95, p<0.001) and the final 15-month CABG SXscore (k=0.70; 95% CI: 0.50-0.90, p<0.001) were all substantial. The number of points deducted to derive the 15-month CABG SXscore was the most reproducible measurement.
CLINICAL OUTCOMES
Due to limited power the present outcome analyses should be interpreted as exploratory and hypothesis-generating. The CABG SXscores were separated into two groups, divided by the median of the normally distributed 15-month CABG SXscores into low (0-21) (n=58) and high-risk groups (≥22) (n=55).
Four-year clinical outcome data demonstrated a trend towards an increased mortality in the high CABG SXscore group compared to the low CABG SXscore group (low CABG SXscore: 1.8%, high CABG SXscore: 9.1%, p=0.084) (Figure 9). Furthermore, an increase in the composite of all-cause death/cerebrovascular accident (CVA)/ myocardial infarction (MI) at four years was also evident in the high CABG SXscore group compared to the low CABG SXscore group (low CABG SXscore: 7.0%, high CABG SXscore: 16.4%, p=0.126).
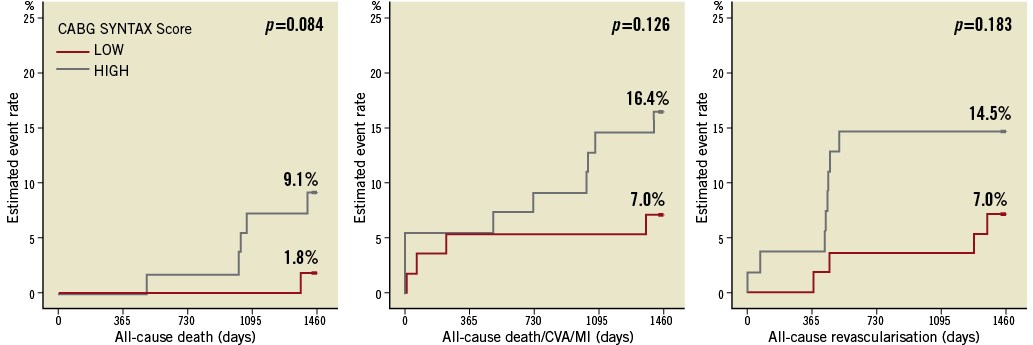
Figure 9. Clinical outcomes separated by the median of the CABG SYNTAX Score into low (0-21) (n=58) and high (≥22) (n=55) score groups. A non-significant trend towards higher mortality (left image) and all-cause death/CVA/MI (middle image) were evident in the high CABG SYNTAX Score group at four years. The peak in repeat all-cause revascularisation between years one and two (right image) were secondary to patients undergoing scheduled coronary angiography, the findings of which triggered repeat revascularisation. CVA: cerebrovascular accident; MI: myocardial infarction
Notably, the Kaplan-Meier curves for all clinical outcomes in the low and high CABG SXscores did not start to separate until after one year of follow-up, with continued separation of the curves up to four years of follow-up. A peak in the incidence of all-cause revascularisation was observed at approximately 15 months secondary to the scheduled study coronary angiogram triggering repeat revascularisation (Figure 9).
Discussion
The main findings of this pilot study are: 1) that the application of the newly developed CABG SXscore appears feasible; 2) that the 15-month CABG SXscore demonstrated a significant decrease in value compared to the baseline SXscore (prior to CABG), secondary to a deduction in points attributed to the segment-weighting of the revascularised coronary vessels; 3) that the CABG SXscore appears to be a reproducible technique when performed by a panel of interventional cardiologists experienced in the reporting of the SXscore; 4) that the deduction of the segment-weighting related points due to the presence of bypass grafts was the most reproducible technique; and 5) that the CABG SXscore may have a long-term prognostic role. Further validation of this newly developed score is required.
The findings from this present study are consistent with the methodology adopted by Leaman et al when applying the Leaman score to patients pre and post CABG18, namely that the segment-weighting for the treated vessel would be deducted if it had a functioning bypass graft anastomosed distal to the treated lesion. In comparison to the baseline SXscore, a clear and significant reduction in the 15-month CABG SXscore was evident. The main difference between the CABG SXscore and the Leaman score was that the points relating to lesion characteristics in the CABG SXscore remained.
One of the unavoidable limitations of the present study was that the coronary angiograms were taken 15 months post CABG and the results compared to the baseline SXscore taken prior to surgery. The mean baseline SXscore and the 15-month native SXscore did however not differ significantly (baseline SXscore 31.6, SD 13.1; 15-month native SXscore 31.1, SD 12.2; p=0.50), making the potential effects of native coronary disease progression at 15 months likely to be of lesser significance.
Conversely, as reported in the SYNTAX-LE MANS substudy, over a quarter of the CABG patients (27.2%) had a significantly diseased (≥50% to <100%) or obstructed (100%) bypass graft at 15 months21. These findings may have led to the underestimation of the 15-month CABG SXscore compared to if the CABG SXscore had been performed post CABG surgery. Although it has previously been reported that early bypass graft occlusion rates may be associated with adverse clinical events29-31, the reported loss of the bypass grafts in SYNTAX-LE MANS were not significantly associated with early MACCE21.
It may be speculated that a proportion of these bypass grafts may potentially have been unnecessary. Early bypass graft patency rates for functionally significant native coronary lesions have been shown to be significantly higher compared to those for bypass grafts with functionally insignificant native coronary lesions32-34. Furthermore, angiographically defined percentage diameter stenoses or the minimum lumen diameter of native coronary vessels29,35 and grafts that have competitive filling with the treated native vessel36,37 have been shown to be predictors of insufficient flow and/or early graft failure. Consequently, despite the limitations, the 15-month CABG SXscore may potentially be representative of patients who have been surgically revascularised at baseline.
ASSOCIATION OF THE CABG SYNTAX SCORE WITH CLINICAL OUTCOMES
The SXscore taken prior to surgery has consistently been shown not to have any significant effect on the short to long-term prognosis after CABG2-4,7,19,20. It has previously been suggested that this observation may be related to the fact that bypass grafts are anastomosed distal to the proximal disease regardless of the complexity of the native coronary disease, providing there are suitable graftable targets4,38. With the CABG SXscore this concept is potentially challenged, with the observation of a non-significant trend towards a higher longer-term mortality and death/MI/CVA in the high (compared to the low) CABG SXscore group. MACCE was not examined as the 15-month scheduled coronary angiogram triggered repeat revascularisation (Figure 9).
PREVIOUS STUDIES
Alderman et al39 previously demonstrated in The Bypass Angioplasty Revascularisation Investigation (BARI) trial –consisting of patients treated with percutaneous or surgical revascularisation who underwent entry and five-year coronary angiographic follow-up– that native coronary disease progression (and not the extent of initial revascularisation) was the predominant determinant of the recurrence of angina and jeopardised myocardium at five years. Notably within the BARI Trial two thirds of the increase in myocardial jeopardy at five years was in previously untreated coronary vessels.
Although other studies have suggested that incomplete surgical revascularisation may be associated with short and long-term adverse outcomes40,41, further predominantly more contemporary studies have suggested that “reasonable” incomplete surgical revascularisation does not have an adverse effect on long-term clinical outcomes42-45. Furthermore, the long-term survival of patients treated with surgical revascularisation in the CASS (Coronary Artery Surgery Study)46 and Rotterdam47 registries has been shown to be associated with more extensive preoperative coronary disease, which in turn was linked to the higher prevalence and severity of other clinical risk factors.
In addition, the Duke graft index48 –an anatomical-based scoring system for patients who had previously undergone CABG– was demonstrated to be significantly more associated with long-term prognosis compared to the native coronary anatomy prior to CABG. Remarkably, the Duke graft index had a design concept that in principle was similar to the CABG SXscore, namely associating anatomical coronary disease (Duke Graft index: based on the number of diseased coronary territories; CABG SXscore: a more sophisticated assessment of the coronary anatomy as previously described) with the level of protection to the diseased territories conferred by bypass grafts in both scores.
IMPLICATIONS OF THE CABG SYNTAX SCORE FOR CLINICAL PRACTICE
The CABG SXscore may thus be regarded as both a marker of anatomical coronary disease complexity, and of the degree of revascularisation secondary to the deduction of segment-weighting points related to the bypass grafts. Furthermore, it may be speculated that the CABG SXscore consisting of anatomical characteristics of the coronary vessel –such as bifurcation disease, calcification, total occlusions, etc.– may reflect the clinical risk profile of the patient and the likelihood of native coronary (and possibly non-coronary as detailed below) atherosclerotic disease progression which, importantly, may actually target the bypass grafts.
It has previously been suggested that the SXscore is a marker of patients with a more adverse clinical risk profile who have evidence of systemic atherosclerotic disease, and are thus at greater longer-term cardiovascular and cerebrovascular risk19,20,49. This hypothesis is supported by the significant and direct relationship of the 10-year predicted Framingham risk scores with the prevalence and magnitude of coronary artery calcium scores50. In addition, the ankle-brachial index51-54 and common carotid intima-media thickness55-58, both markers of extra-cardiac disease, have been correlated with the severity of coronary artery disease and even clinical events.
Notably, the clinical outcomes in the present study did not start to separate until after one year, and continued to separate at up to four years (Figure 9). It may be further hypothesised that the curves would continue to separate in the longer term where the clinical manifestations of continued native atherosclerotic coronary disease progression, and importantly bypass graft disease progression particularly with SVG, would become more apparent. Consistent with these hypotheses are the findings that SVGs have been shown to be protective in the first seven years, and that thereafter mortality increases significantly in parallel to the gradual loss of SVG patency47,59.
POTENTIAL CLINICAL AND RESEARCH APPLICATIONS OF THE CABG SYNTAX SCORE
Potential clinical applications of the CABG SXscore include long-term risk stratification of patients who have previously undergone CABG to aid in the identification of a group at high risk for future clinical events and repeat revascularisation. Even without the use of a CABG SXscore, it may be further postulated that higher SXscore patients may benefit more from undergoing revascularisation with more durable grafts that have a proven long-term patency (e.g., LIMA and RIMA) compared to SVG60,61.
Although aggressive risk factor control would undoubtedly improve the prognosis of all these patients, perhaps future study may target patients with a higher SXscore/CABG SXscore who may potentially benefit from more aggressive risk factor control with established and emerging drugs that cause atherosclerotic disease regression.
Other potential applications of the CABG SXscore in a research setting include the allowance of the incorporation of CABG patients into contemporary stent trials measuring the SXscore, where such patients are at present excluded.
STUDY LIMITATIONS
As previously discussed, apart from the time frame at which the CABG SXscore was taken, the main limitation of this study is that there was limited power to examine long-term clinical outcomes. Despite this limitation, a non-significant trend towards more adverse clinical outcomes in the higher CABG SXscore group was seen, which is further supported by the concept of the Duke graft index, as previously discussed48.
One other limitation is that the CABG SXscore does not account for the type of graft anastomosed and the characteristics of the graft disease (if present), except if there is obstructive graft disease or not. This is perhaps more notable with the LIMA bypass graft given its proven higher long-term patency rates compared to other types of bypass graft60,61. The hypothesis central to the CABG SXscore does, however, relate to the native SXscore and its apparent association with clinical comorbidity, with the additional “protection” conferred by the bypass grafts. Furthermore, reducing the CABG SXscore by an arbitrary number of points based on the type and numerous anatomical complexities of the bypass graft would substantially increase the complexity of the analyses, making this impractical.
FUTURE DIRECTIONS
Potentially, the integration of the CABG SXscore into an online algorithm, as is currently available with the SXscore1, may serve to simplify the calculation of the CABG SXscore. The functional SYNTAX Score –a fractional flow reserve (FFR) guided SYNTAX scoring methodology– has recently been demonstrated to improve the diagnostic accuracy of the SXscore62. Furthermore, the feasibility of undertaking non-invasive anatomical and fractional flow measurements has since been proven, utilising computational fluid dynamics applied to coronary computed tomography (CT) angiography63. The application of this emerging technology to the CABG SXscore may improve the diagnostic accuracy and reproducibility of the CABG SXscore. In addition, the non-invasive combined coronary CT and FFR technology may potentially allow for the automatic adjustment of the vessel-segment weighting for coronary vessels based on actual measured blood flow, in order to calculate a more “physiological” functional CABG SXscore.
Conclusion
The calculation of the CABG SXscore is feasible, reproducible and may have a long-term prognostic role in the assessment of risk in patients undergoing coronary artery bypass grafting. Confirmation and validation of the findings from this pilot study are required in larger studies.
Acknowledgements
The authors express their gratitude to all of the study centres and participants whose work made this study possible. Furthermore, thanks go to Peggy Pereda and Jian Huang of Boston Scientific for their invaluable support in accessing the study database. The authors thank Ana Guimarães of Cardialysis for her technical support in producing the images.
Funding sources
The SYNTAX Trial was funded by Boston Scientific.
Conflict of interest statement
K.D. Dawkins is a full-time employee in Boston Scientific and holds stock in Boston Scientific. M. Mack has served on the Speakers’ Bureau of Boston Scientific, Cordis and Medtronic. T. Feldman reported serving on the Speakers’ Bureau of Boston Scientific, receiving grant support from Abbott, Atritech, BSC, Edwards, Evalve, and consulting for Abbott, Coherex, Intervalve, Square One, WL Gore. M. Morice reported that her institution received a research grant from Boston Scientific. M.A. Morel, M. van der Brand and G.A. van Es are employees of Cardialysis BV, The Netherlands. The other authors have no conflict of interest to declare.
Scores
LEAMAN SCORE
The Leaman Score64 is based on the severity of luminal diameter narrowing and is weighted according to the usual blood flow to the left ventricle in each vessel or vessel segment. In a right dominant system, the right coronary artery (RCA) supplies approximately 16% and the left coronary artery approximately 84% of the blood flow to the left ventricle. This 84% is normally directed 66% towards the left anterior descending (LAD) and 33% to the left circumflex (LCx) vessels. Consequently, theLMS, LAD and LCx supply approximately x5, x3.5 (84/16 x0.66) and x1.5 respectively as much blood as the RCA to the left ventricle, the values of which are designated as the respective vessel’s segment-weighting factors. In a left dominant system, the RCA does not contribute to the blood supply of the left ventricle, which is instead supplied by the LCx. Thus the LMS supplies 100% of the blood flow to the left ventricle. Hence the LAD provides 58% (segment-weighting factor x3.5) and the LCx 42% (segment-weighting factor x2.5) of the total blood flow to theLV. These concepts ultimately formed the basis of the segment-weighting factors that were incorporated into the now validated SXscore65-73.
APPLICATION OF THE LEAMAN SCORE IN PATIENTS UNDERGOINGCABG. Leaman et al previously applied the Leaman Score, derived from the segment-weighting factors, to patients at baseline and post CABG surgery64. This concept was based on the principle that the segment-weighting for the treated vessel would be deducted if it had a functioning bypass graft anastomosed distal to the treated lesion. For example, a significant mid RCA lesion would score a segment-weighting factor of 1x2 (2 points) if the lesion was significantly (non-total) diseased, or 1x5 (5 points) if the lesion was occluded. Post-surgery, if the graft to the RCA was patent, the respective segment-weighting points for the treated vessel would be deducted. Conversely, if the graft was occluded, the points would remain unaltered.
SYNTAX SCORE
The SXscore methodology has previously been described74-77. In brief, the SXscore was developed by combining the importance of a diseased coronary artery segment by the vessel-segment weighting (modified Leaman Score)64, adverse characteristics of such a lesion for revascularisation (ACC/AHA lesion classification)78,79 and the Medina classification system for bifurcation lesions80,81.
Each vessel segment, 1.5 mm in diameter or greater, with a ≥50% diameter stenosis by visual estimation, is awarded a multiplication factor related to the location of the lesion, and the severity of the stenosis (non-total vs. total occlusion). Further characterisation of the coronary lesions leads to the addition of more points. These include features of total occlusions (duration, length, blunt stump, presence of bridging collaterals or side branch), the presence of bifurcation (based on the Medina classification) or trifurcation disease (number of diseased branches involved), side branch angulation, aorto-ostial lesion, severe tortuosity, lesion length >20 mm, heavy calcification, thrombus and diffuse or small vessel disease. The above information is entered into the online available SXscore algorithm75 which automatically sums each of these features to calculate the total SXscore.
DEFINITIONS OF VESSELSEGMENTS. A table of vessel segments relating to the SYNTAX Score is detailed hereafter (Online Table 1).
Further illustrative examples of the application of the CABG SXscore
CASE 1
Occluded LMS (#) in a left dominant system gave a native SXscore of 39 (upper image). The ostial involvement of the LAD (black arrow) was regarded as part of the LMS lesion as it was located within ≥3 vessel reference diameters from the occluded LMS lesion. A patent LIMA inverse Y graft anastomosed to the mid LAD (upper white arrow), with sequential anastomoses to the 1st, 2nd and 3rd OM branches (lower three white arrows) are shown. Based on the segment-weighting 30 points were deducted from the native SXscore. Final CABG SXscore was therefore 39–17.5–12.5=9 points (Online Figure 1).
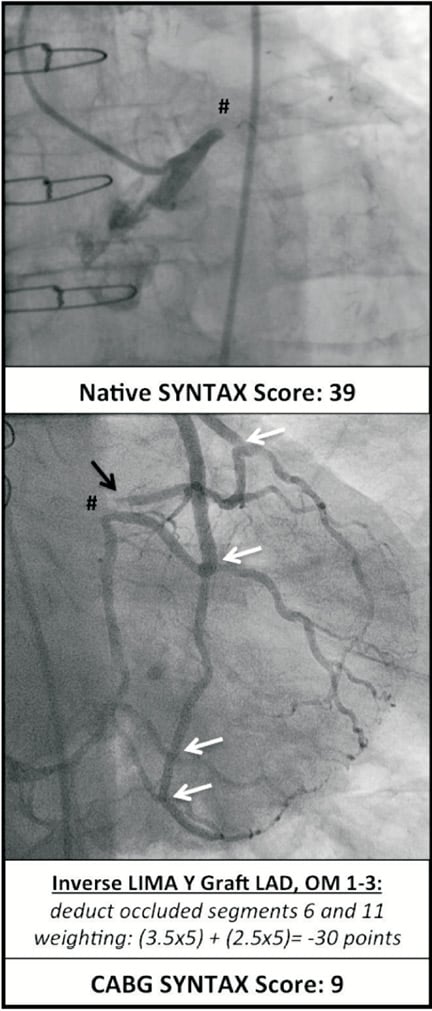
Online Figure 1. Example of the calculation of the CABG SXscore in a patient with an occluded LMS. Black arrows indicate obstructive native coronary disease; white arrows indicate patent anastomosis sites of grafts to vessels, # occluded LMS. LMS: left main stem; RCA: right coronary artery; LIMA: left internal mammary artery; OM: obtuse marginal; LAD: left anterior descending artery; SVG: saphenous vein graft
CASE 2
Upper images: native SXscore was 35.5 with distal LMS disease (Medina 1.1.1), distal RCA disease, and an occluded ostial LCx (#).
Lower images: distal RCA protected by SVG (left image), therefore 1x2 points were deducted from the native SXscore. Occluded ostial LCx is under “ischaemic protection” by the RIMA to the distal OM (middle image) secondary to disease more proximal to the anastomosis. Therefore 1.5x3 points are deducted from the native SXscore (no points are added for the OM disease as it is protected by the RIMA graft). The ostial LAD disease is protected by the LIMA (right image) anastomosed to the distal LAD with no intervening obstructive disease, so 3.5x2 points are deducted from the native SXscore. Final CABG SXscore was therefore 35.5–2–4.5–7=22 points (Online Figure 2).
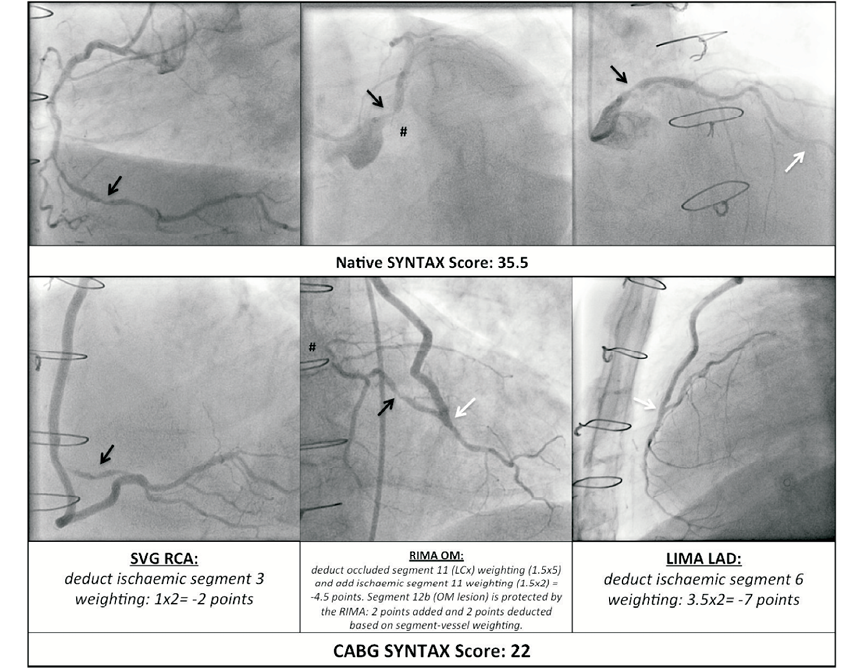
Online Figure 2. Example of the calculation of the CABG SXscore in a complex case. Black arrows indicate obstructive native coronary disease; white arrows indicate patent anastomosis sites of grafts to vessels. LMS: left main stem; RCA: right coronary artery; LIMA: left internal mammary artery; RIMA: right internal mammary artery; LCx: left circumflex; OM: obtuse marginal; LAD: left anterior descending artery; SVG: saphenous vein graft

