Percutaneous coronary intervention (PCI) was performed in a patient with unstable angina and severe left main coronary (LMCA) disease. The lesion was predilated with a 3.5×11 mm compliant balloon at 16 atm, and a 4×14 mm everolimus-eluting stent was deployed (Figure 1A).
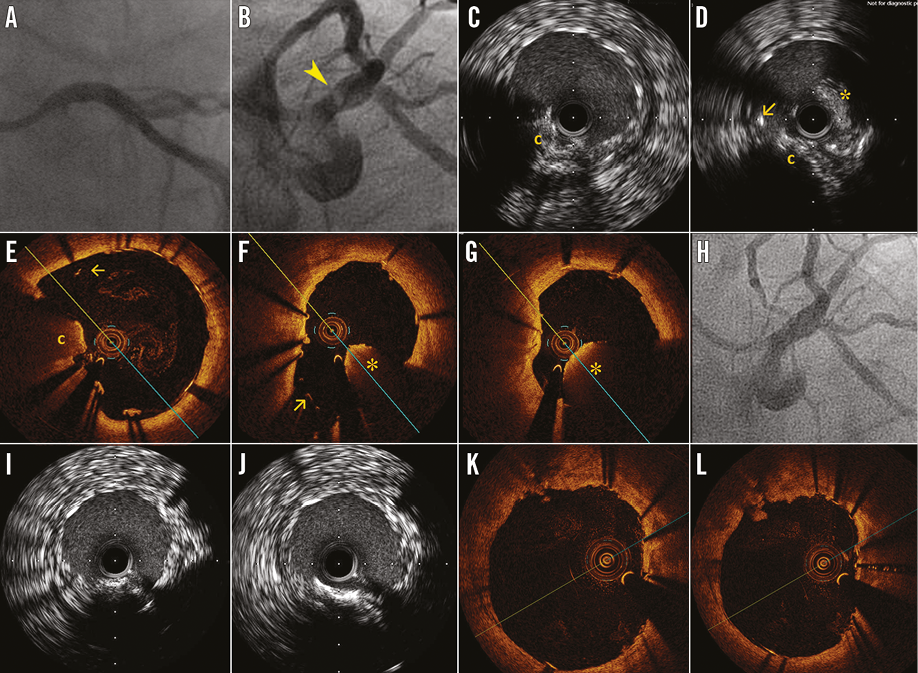
Figure 1. A) AP caudal post LMCA PCI angiography. B) Intra-stent mobile image compatible with stent thrombosis (arrowhead). C & D) and E-G) IVUS and OCT images (distal to proximal) showed a calcium spicule protruding into the lumen (“c”) and causing stent malapposition (arrow), with large stent thrombosis (“*”). H-L) Post-procedure imaging showing improvement of apposition and reduction of thrombus.
Twenty days after PCI the patient was referred for recurrence of symptoms. Angiography demonstrated early stent thrombosis (Figure 1B). IVUS (Figure 1C, Figure 1D) showed an eccentric calcified atheroma with a large calcium spicule protruding into the lumen distally and thrombus proximally. OCT (Figure 1E-Figure 1G) showed a large protruding calcium spicule impeding the correct stent apposition, and a black retro-optic shadow intra-stent protrusion suggested a red thrombus proximally. The thrombosis was explained by the extended malapposition of the LMCA stent due to a large calcified spicule. Thromboaspiration and angioplasty with a 4.5×12 mm non-compliant balloon at 20 atm were performed with improvement of malapposition and thrombus burden (Figure 1H-Figure 1L).
Conflict of interest statement
The authors have no conflicts of interest to declare.