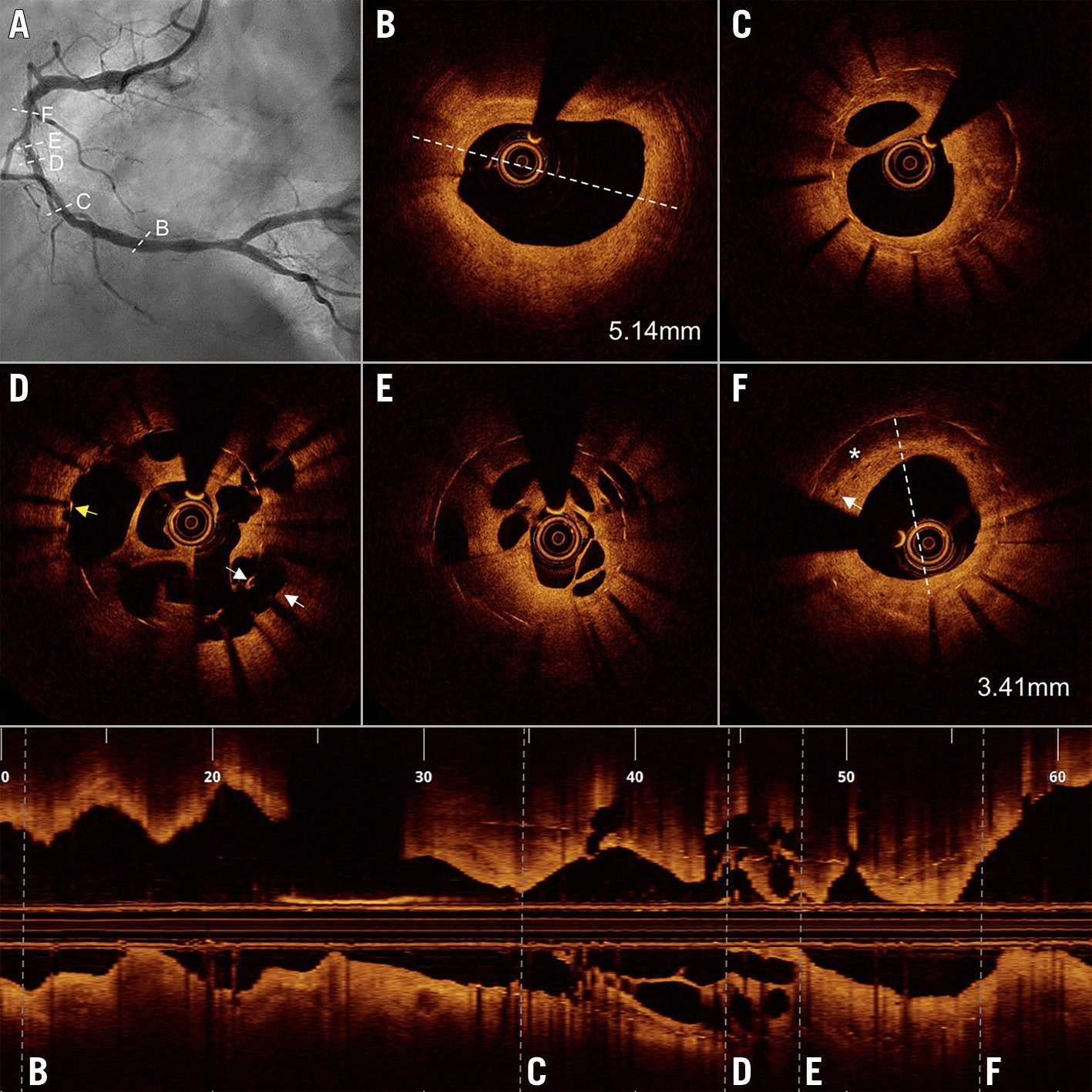
Figure 1. Angiography and optical coherence tomography findings. A) Angiography showed in-stent restenosis in the right coronary artery. B) External elastic membrane diameter at the distal reference was 5.14 mm. C) - E) Recanalised thrombus with multiple channels within the stent. D) Recanalised thrombus with malapposition (white arrows) and uncovered struts (yellow arrow). F) Neoatherosclerosis with lipid pool (asterisk) and microvessels (white arrow) in the setting of an undersized stent.
A 68-year-old man was admitted to our hospital with unstable angina. His medical history was remarkable for an acute myocardial infarction one year before, treated with a zotarolimus-eluting stent (3.5×30 mm) in the mid right coronary artery. Coronary angiography showed a diffused in-stent restenosis (ISR) with haziness and filling defects (Figure 1A, Moving image 1). In order to identify the underlying mechanisms of ISR, optical coherence tomography (OCT) was performed due to its high resolution. OCT showed a large, recanalised thrombus with multiple channels divided by thin septa (longitudinal view and Figure 1C-Figure 1E) in the setting of an undersized stent (Figure 1F compared to Figure 1B, distal reference). Coexistent malapposition, uncovered struts and neoatherosclerosis were also detected (Figure 1D, Figure 1F, Moving image 2).
Based on OCT findings, a scoring balloon followed by high-pressure non-compliant balloon inflation was used to break the multiple septa, compress the neointima and fully expand the undersized and malapposed stent segments (Moving image 3). Two sirolimus-eluting stents (4.0×29 mm and 4.0×23 mm) were implanted to cover the ISR segment and ruptured thin-cap fibroatheroma distally to the stent. OCT documented optimal stent expansion with a large minimum stent area (Moving image 4).
Although recanalised thrombus with multiple channels has been reported in native coronary disease1, it is rarely seen as a contributing mechanism of ISR. This case suggests a prior thrombotic event followed by a recanalisation process. Mechanisms leading to recanalised thrombus are intriguing. The most likely driver for failure was undersizing of the original stent in the setting of an acute myocardial infarction, leading to significant malapposition. When encountering stent failure, OCT should be the preferred imaging tool to understand the underlying mechanisms of failure and facilitate treatment strategies. There are no specific treatments for recanalised thrombus; however, appropriate lesion preparation with stent implantation under OCT guidance is a pragmatic strategy.
Funding
Dr. Yu has received research grants from the National Key R&D Program of China (2016YFC1301103). Dr.Jia has received grants from the National Natural Science Foundation of China (81722025)
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Baseline angiography showing a diffused in
Moving image 2. Baseline OCT images illustrating coexistent mechanisms of in-stent restenosis and disrupted thin-cap fibroath
Moving image 3. OCT images after a scoring balloon and high pressure non-compliant balloon showing successful lesion preparation.
Moving image 4. OCT documented satisfactory final results with adequate expansion and large minimum stent area.