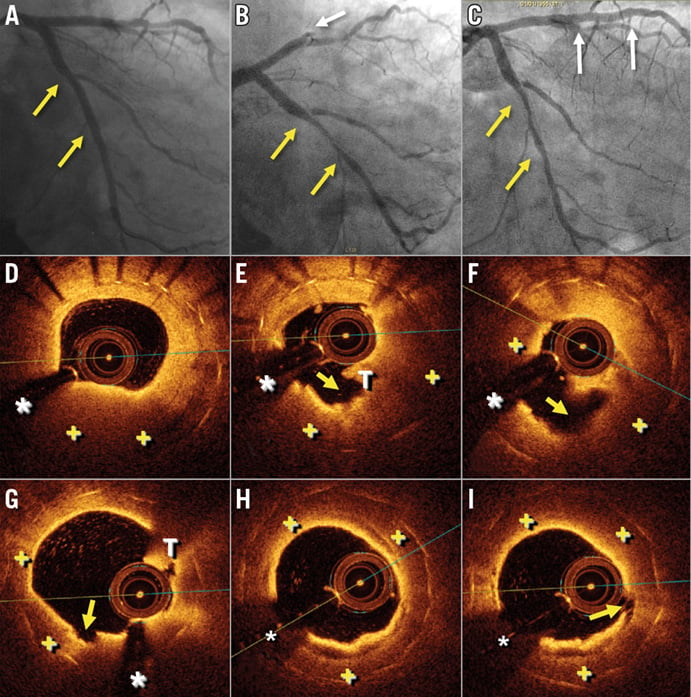
A 53-year-old man, with previous bare metal stent (BMS) implantation in the left circumflex (LCX) coronary artery 10 years ago (Panel A, yellow arrows), was admitted with a large anterior ST-segment elevation acute myocardial infarction (STEMI). Urgent coronary angiography showed a total occlusion of the left anterior descending (LAD) coronary artery (Panel B, white arrow) and also a severe in-stent restenosis (ISR) in the LCX (Panel B and Panel C, yellow arrows). A drug-eluting stent (DES) was implanted successfully in the LAD (Panel C, white arrows). Three days later a new coronary angiography was performed in order to treat the ISR in the LCX. Optical coherence tomography (OCT) revealed the presence of complicated neoatherosclerosis, with a glistening neointima with dark areas consistent with lipid pools (Panel D-Panel I, +) and several ruptured and ulcerated plaques, associated with an intracoronary red thrombus (Panel E-Panel I, yellow arrow and T). A bioresorbable vascular scaffold was successfully implanted.
Some previous studies have reported the association between in-stent neoatherosclerosis and progression of native coronary atherosclerosis. A pan-inflammatory process might be implicated. To the best of our knowledge, the presence of ruptured and complicated neoatherosclerosis in a “non-culprit” remote vessel in patients presenting with STEMI has not been reported previously.
Conflict of interest statement
The authors have no conflicts of interest to declare.