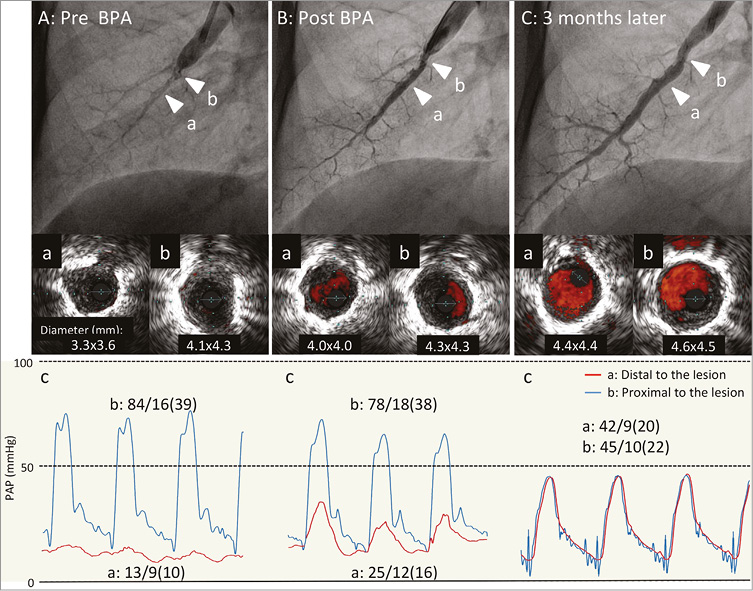
A 72-year-old woman with inoperable chronic thromboembolic pulmonary hypertension underwent balloon pulmonary angioplasty (BPA). Intravascular ultrasound (Eagle Eye® Platinum; Volcano Corp., San Diego, CA, USA) revealed severe stenosis in the right A8 with a narrow vessel distal to the lesion (Panel Aa, Panel Ab). According to a pressure wire (Primewire Prestige® PLUS; Volcano Corp.) measurement, the pulmonary artery pressure distal to the lesion was much lower than that proximal to the lesion with little pulse pressure (Panel Ac). Immediately after the dilation with a 2.5 mm balloon catheter (IKAZUCHI PAD; Kaneka, Osaka, Japan) at 14 atm, the vessel diameter distal to the lesion expanded, although the vessel diameter at the lesion was unchanged and angiographic stenosis was still observed (Panel Ba, Panel Bb). The pulmonary artery pressure distal to the lesion increased as a result of the improved blood flow (Panel Bc). Next, the right A7 and A10 were also treated. Three months later, angiographic stenosis and the blood flow improved even more, although no additional treatment was performed at the lesion. Intravascular ultrasound observations revealed dilatation of the lumen diameter and the blood flow improved (Panel Ca, Panel Cb), effectively eliminating the pressure gradient across the lesion (Panel Cc).
Increase in perfusion pressure in the pulmonary artery distal to the obstruction with partial detachment of the organised thrombi may be a driving force to dilate pulmonary arteries spontaneously over time without causing restenosis after BPA. Thus, the immediate elimination of the pressure gradient may not be necessary for the long-term success of BPA.
Conflict of interest statement
H. Matsubara has received lecture fees from GlaxoSmithKline K.K., Actelion Pharmaceuticals Japan Ltd., and Pfizer Japan Inc. The other authors have no conflicts of interest to declare.