Group 4 pulmonary hypertension (PH), i.e., chronic thromboembolic pulmonary hypertension (CTEPH), is the most curable form of PH. The gold standard treatment is surgical pulmonary endarterectomy (PEA)1, which is able to remove obstructive pulmonary artery lesions, normalise or reduce pulmonary vascular pressure and resistance, reverse right ventricular dysfunction, and improve exercise capacity and quality of life. Nevertheless, PEA has a few important limitations2: a sizeable proportion of patients with CTEPH are not eligible for PEA; up to 30-40% of the patients have residual or recurrent PH; PEA requires surgical expertise which is generally confined to a few referral institutions. PH-targeted medical therapy may complement PEA by addressing secondary microvascular changes akin to that seen in pulmonary arterial hypertension, and it can mitigate the detrimental effects of PH when PEA is either not effective or not feasible. However, it cannot target the proximal mechanical component of CTEPH and is therefore basically of a palliative nature. In this context, balloon pulmonary angioplasty (BPA) represents a very promising treatment, being able to address the unmet clinical need of many patients with CTEPH.
Originally described in the early 2000s, BPA was fraught with fatal and life-threatening complications and therefore was virtually abandoned. It was only in 2012, thanks to the refined BPA technique developed in Japan, that BPA started to gain an established role for the treatment of CTEPH3. Since then, the results of several BPA registries have been reported, showing consistent results across different institutions and countries. BPA has been associated with a reduction in mean pulmonary artery pressure (mPAP) and in pulmonary vascular resistance (PVR), improvements in symptoms, right ventricular function and haemodynamics. In parallel, the incidence of serious complications has declined steadily. Hence, BPA in experienced centres is now recommended by current guidelines for patients who are not eligible for PEA1. The modern BPA technique is based on the use of percutaneous coronary intervention material and consists of multiple, staged procedures, with progressive dilatation of obstructions in different pulmonary areas, commonly starting from the basal lung segments. Lesions are initially dilated with undersized balloons in order to reduce the risk of reperfusion injury, and treatment is then optimised during subsequent procedures.
Several issues about BPA remain unsettled: including clinical, functional and haemodynamic targets; long-term efficacy, role and timing of concomitant PH-specific medical therapy; and others. Many ongoing studies will fill the lingering gaps in our knowledge and help in defining the clinical role of BPA and its relationship with other available treatments for CTEPH. In parallel, there are logistical issues that should also be addressed, including where BPA should be performed to maintain optimal clinical results while ensuring widespread availability of the treatment, and how to ensure a balanced evaluation of inoperability for PEA, considering that the surgical expertise is limited to few centres.
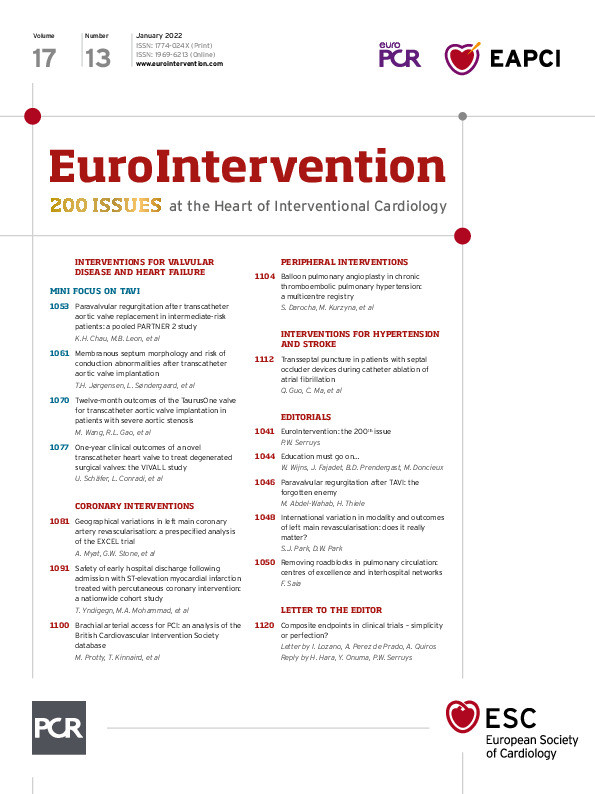
The paper by Darocha and colleagues4, published in this issue of EuroIntervention, represents an extraordinary contribution to the BPA literature and addresses many of these issues.
It is the first nationwide multicentre registry based on a solid interhospital network, where two major CTEPH teams with a cardiac surgeon experienced in PEA, an interventional cardiologist experienced in BPA, and a cardiologist experienced in medical management of PH evaluated all the patients for operability and recommended the best treatment strategy. Diagnosis of CTEPH was based on a rigorous diagnostic algorithm. BPA was performed in eight centres distributed throughout Poland. Clinical outcomes and incidence of complications were comparable to other European and international experiences. Long-term survival after BPA was excellent, being 92.4% in the whole population at three years and 95.2% for those who completed the treatment according to specific criteria. Haemodynamic improvement was maintained at midterm follow-up.
The Polish BPA experience confirms the clinical value of BPA and demonstrates the potential of networking to treat rare diseases such as CTEPH. Given the low incidence of CTEPH, it is unlikely that many centres could develop sufficient expertise to provide excellent results. The present study emphasises the need to establish recognised centres of excellence in CTEPH to ensure that patients always receive the best available treatment. At the same time, it suggests that BPA could be performed within a network of a few more centres, provided they have experience in the treatment of PH, submit cases for decision-making to an established CTEPH team, share common knowledge and rigorous methodology, and follow adequate, assisted training; a virtuous synergy to remove roadblocks in the pulmonary circulation!
Conflict of interest statement
The author has no conflicts of interests to declare in relation to this editorial.
Supplementary data
To read the full content of this article, please download the PDF.