Abstract
Background: Balloon pulmonary angioplasty (BPA) is a promising therapy for patients with chronic thromboembolic pulmonary hypertension (CTEPH) who are ineligible for pulmonary endarterectomy.
Aims: The present study aimed to evaluate the safety and efficacy of BPA for CTEPH using the first multicentre registry of a single European country.
Methods: Data were obtained from the Database of Pulmonary Hypertension in the Polish Population (NCT03959748), a prospective, multicentre registry of adult and paediatric pulmonary arterial hypertension (PAH) and CTEPH, for a total of 236 patients with confirmed CTEPH (124 women; mean age 67 years) who underwent 1,056 BPA procedures at eight institutions in Poland.
Results: In 156 patients who underwent follow-up assessments after a median of 5.9 (IQR: 3.0-8.0) months after final BPA, the mean pulmonary arterial pressure decreased from 45.1±10.7 to 30.2±10.2 mmHg (p<0.001) and pulmonary vascular resistance from 642±341 to 324±183 dynes (p<0.001), and the six-minute walking test (6MWT) improved from 341±129 to 423±136 m (p<0.001). Pulmonary injury related to the BPA procedure occurred in 6.4% of all sessions. Eighteen patients (7.6%) died during follow-up, including 4 (1.7%) who died within 30 days after BPA. Overall survival was 92.4% (95% confidence interval [CI]: 87.6%-94.9%) three years after the initial BPA procedure.
Conclusions: This multicentre registry confirmed significant improvement of haemodynamic, functional, and biochemical parameters after BPA. Complication rates were low and overall survival comparable to the results of another registry. Therefore, BPA may be an important therapeutic option in patients with CTEPH in Poland.
Introduction
Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare condition with significant risk of morbidity and mortality. CTEPH is associated with incomplete thromboembolic resolution, which leads to narrowing and obstruction of the pulmonary arteries, resulting in high pulmonary vasculature resistance, increased right heart afterload, and progression of right heart failure if left untreated1. The gold standard treatment is pulmonary endarterectomy (PEA)2. The range of CTEPH patients ineligible for PEA varies from 12.0% to 60.9%, according to the centre3. The reasons for non-operability are usually distal thromboembolic lesions, high risk-benefit ratio, or patient refusal45. Balloon pulmonary angioplasty (BPA) was first reported in 1988 as an alternative treatment for a patient with CTEPH who was ineligible for PEA6. The first case series of BPA in 2001 reported a discouraging 5.6% death rate, a 61% incidence of lung injury, and a 17% requirement for mechanical ventilation, despite technical success and significant haemodynamic improvement7. BPA underwent later refinement by Japanese interventionists, which had set a new standard for the procedure by 201289. Since that time, the efficacy of BPA in improving haemodynamics, exercise capacity, and other parameters has been established by case series and small cohorts reported by several groups in Japan1011 and Europe12131415161718. In 2017, a group of Japanese investigators published the results of the first multicentre registry, which included 308 CTEPH patients (1,408 procedures). To date, this remains the largest study evaluating the efficacy and safety of BPA. The largest European series, which described German19 and French20 experiences, was published shortly thereafter. We assessed the efficacy and safety of BPA in the first multicentre European registry study.
Methods
Patient selection
We included patients with CTEPH who underwent BPA at eight institutions in Poland (Otwock, Krakow, Warsaw, Poznań, Wrocław, Szczecin, Zabrze, and Katowice) between July 2013 and June 2019. These are pulmonary hypertension (PH) referral centres where BPA was introduced after this treatment was initiated in 2013 in Otwock21. All consecutive patients with CTEPH who underwent BPA in the participating centres were enrolled.
Diagnosis of CTEPH was based on detailed medical history, physical examination, chest radiography, chest computed tomography, transthoracic echocardiography, lung ventilation-perfusion scintigraphy, right heart catheterisation (RHC), and angiographic demonstration of multiple stenoses and obstruction of the bilateral pulmonary arteries according to current guidelines122. All patients were referred to an experienced CTEPH team for evaluation of operability. Two major CTEPH teams (at Otwock and Krakow) worked actively in Poland in the period of recruitment. Each consisted of a cardiac surgeon experienced in PEA, a cardiologist experienced in the medical management of PH patients, and an interventional cardiologist experienced in BPA. Those two CTEPH teams played a central role in assessing CTEPH patients for the optimal treatment strategy and are the only institutions performing PEA in the country. Participating BPA centres were obliged to accept the CTEPH team decision of non-operability before they started BPA treatment. All of the patients were informed about the potential risks and benefits of the BPA procedure, and all provided written informed consent.
Data collection
Data were obtained from the Database of Pulmonary Hypertension in the Polish Population (BNP-PL; NCT03959748), a prospective, multicentre registry of adult and paediatric PAH and CTEPH patients created in a Central Eastern European country23. The design of the BNP-PL registry, enrolment criteria, and data collection have been described in detail elsewhere24. The BPA arm of the registry had two parts. The first part consisted of retrospective enrolment of all adults with CTEPH treated with BPA from July 2013 to February 2018 in all eight BPA centres in Poland. The second part consisted of prospective enrolment from March 2018 to November 2019 using the same inclusion criteria. The study protocol was reviewed and accepted by the Bioethical Committee (L.dz.OIL/KBL/27/2018). Data included medical history, comorbidities, World Health Organization (WHO) Functional Class, exercise tolerance measured by the 6-minute walk test (6MWT), laboratory measurements, haemodynamic parameters, and treatment. Regarding BPA, the number of procedures, the contrast medium volume, radiation time, number of treated lesions, reason for BPA termination, and complications were collected. The classification of complications proposed by the Working Group of the 6th World Symposium of Pulmonary Hypertension was used2. The complications were divided into two parts - during the procedure, and after the procedure. The first group comprised vascular injury, which was defined as extravasation of contrast medium recognised according to wire perforation of the vessel, balloon catheter overdilatation or high-pressure contrast injection. Vascular dissection was recognised when angiographic patterns of dissection were present in control selective angiography after balloon catheter inflation. Severe allergic reaction to contrast medium was defined when shock occurred after the contrast medium injection. The second group comprised lung injury, which was defined when radiographic opacities were seen on control chest radiography or computed tomography. Renal dysfunction was defined as an increase in serum creatinine ≥25% or an absolute increase ≥0.5 mg/dl compared to the baseline value 48-72 hours after exposure to contrast medium. Access-site problems included prolonged bleeding, aneurysm, or fistula. Investigators may have reported other complications.
Outcomes of BPA
The BPA treatment was defined as being complete when all accessible lesions were addressed according to current experience or the patient did not consent to further treatment. In cases with complex lesion morphology (e.g., pouch lesions, chronic total occlusions, organised proximal lesions) which were not accessible in terms of the operator`s experience, the BPA treatment was completed using the definition technical difficulties.
The follow-up period for monitoring survival ended on 30 November 2019. The primary endpoint for survival analysis was all-cause death. Long-term survival from the initial BPA procedure and the final BPA procedure was evaluated for all participating patients. The efficacy of BPA procedures was evaluated upon full examination (including functional class, 6MWT, biochemical and haemodynamic parameters) of all patients who completed their BPA treatment in the short-term (3-9 months after final BPA procedure) and long-term follow-up (at least 12 months after final BPA procedure).
Statistical analysis
Nominal variables are presented as numbers and percentages. Continuous variables with normal distribution are presented as mean and standard deviation (SD). Variables with a non-normal distribution are presented as the median and interquartile range (IQR). The differences between the parameters at baseline and follow-up were analysed by the paired Student’s t-test or Wilcoxon signed-rank test where appropriate. To compare prevalent and incident patients we used the Mann-Whitney U test for continuous variables and the chi-square test for categorical variables. The improvement in functional capacity, biomarkers, and haemodynamic parameters at the short-term follow-up are expressed as a ratio of the baseline values. Secondary survival analyses were carried out using the Kaplan-Meier method. All statistical analyses were performed using Statistica13.1 software (StatSoft). Significance was defined as p<0.05.
Results
Patient characteristics
Two hundred and thirty-six CTEPH patients were recruited into the study. The patient distribution among centres participating in the BPA programme is presented in Supplementary Table 1. Patient characteristics at study enrolment are summarised in Table 1. The differences between prevalent and incident subpopulations are described in Supplementary Table 2.

More than half of the patients were women. History of a previous episode of acute pulmonary embolism (APE) was present in 80% of patients. Seventy-nine patients (33.4%) were screened for thrombophilia, and it was found in 15.1% (n=12) of them. The following thrombophilic disorders were noted: antiphospholipid syndrome (n=6), high coagulation factor VIII level (n=2), factor V Leiden mutation (n=2), protein S deficiency (n=3), protein C deficiency (n=2), and antithrombin III deficiency (n=1). Eighteen patients were diagnosed with psychiatric disorders; 16 of them suffered from depression, and in two cases schizophrenia was noted.
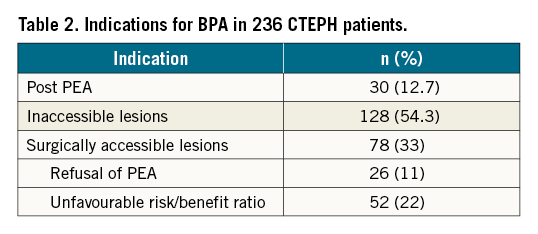
All patients were evaluated for eligibility for PEA before they underwent BPA. At baseline, 97% of patients were examined with pulmonary angiography, 84% had angio-CT, and 28% had a V/Q (ventilation/perfusion) scan performed to choose the optimal treatment strategy for CTEPH for each patient. Thirty patients (12.7%) had already undergone PEA, and the risk of reoperation was considered to be high. A total of 128 (54.3%) patients were diagnosed as having surgically inaccessible lesions, and 78 (33%) patients were found to be technically operable. Among them, 52 patients were considered to have an unfavourable risk/benefit ratio based on comorbidities or older age. The remaining 26 patients refused surgical treatment and were assigned to BPA (Table 2).
In 164 patients (69.4%), PH-specific therapy was administered before the initiation of BPA treatment. Monotherapy with riociguat in 101 cases (61.5%), sildenafil in 52 cases (31.7%), and treprostinil in 9 cases (5.5%). Two patients (1.2%) received a combination of treprostinil and sildenafil. The treatment with PH-specific medication at baseline, short-term, and long-term follow-up is presented in Supplementary Table 3. Anticoagulation consisted of direct oral anticoagulants in 136 patients (57.6%), rivaroxaban in 106 patients (77.9%), dabigatran in 28 patients (20.5%), and apixaban in 2 patients (1.4%). A vitamin K antagonist was administered in 74 patients (31.4%), and 26 patients (11%) received low molecular weight heparin. Thirty-two patients (13.5%) received oxygen therapy before BPA therapy was started.
BPA procedure
During the study period, 1,056 BPA procedures were performed with a median 4.5 (IQR: 2-7) procedures per person. A total of 4,852 lesions were treated. A mean 290±124 ml of contrast medium was used per BPA session. The mean radiation dose was 949±688 mGy per session, and the mean time for fluoroscopy was 44±15 minutes during a single BPA procedure. There were some differences in BPA technique between participating centres, especially in the use of intravascular ultrasound (IVUS) and pressure wire1314.
BPA treatment was considered complete in 172 (72.8%) patients. Median time from the first to the final procedure was 7.7 (IQR: 3.4–13.9) months. The reasons for BPA termination were haemodynamic improvement (n=121, 70.3%), symptomatic improvement (n=44, 25.5%), technical difficulties (n=4, 2.3%), and patient withdrawal (n=3, 1.7%).
Outcome of BPA
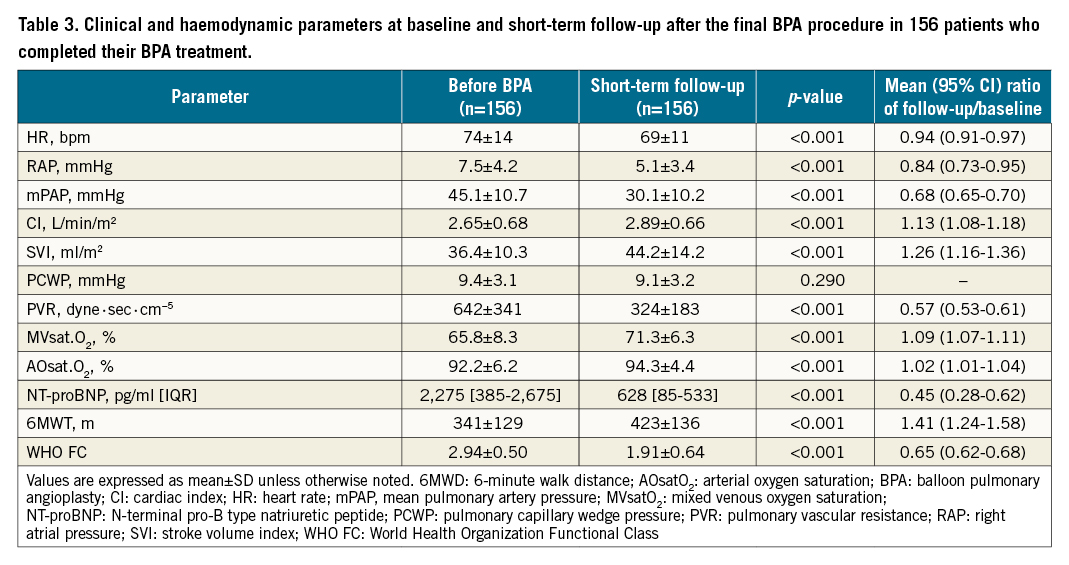
The haemodynamic, biochemical, and functional parameters of 156 patients who completed the treatment cycle and underwent short-term follow-up a median 5.9 months (IQR: 3.0-8.0) after final BPA are shown in Table 3. At baseline, 86% of patients were in WHO Functional Class III or IV. Haemodynamic parameters were severely compromised, with high mPAP and PVR at baseline. WHO Functional Class, distance covered in the 6MWT, and NT-proBNP were significantly improved at the short-term follow-up (Table 3). A significant reduction in mean pulmonary artery pressure (mPAP) and pulmonary vascular resistance (PVR) was found during control RHC.
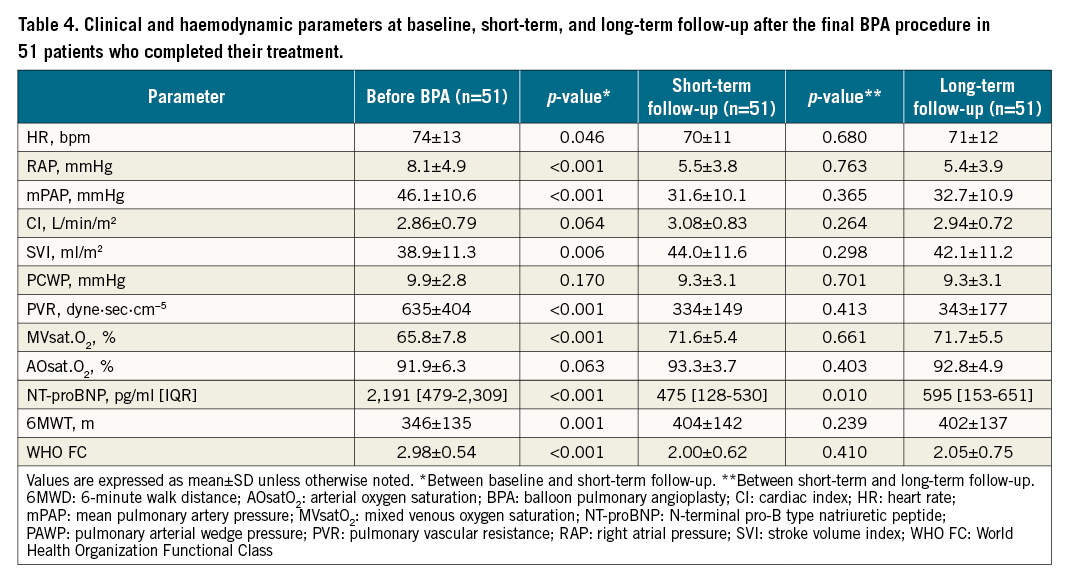
Fifty-one patients (30.1% of those who terminated BPA treatment) underwent a full evaluation with control RHC at long-term follow-up a median 17.7 months (IQR: 14.0–24.8) after the final BPA procedure. The improvement achieved by BPA was maintained (Table 4). Pulmonary haemodynamics, including mPAP and PVR, did not worsen.
BPA did not reduce the use of PH-specific medication in short-term and long-term follow-up (Supplementary Table 3).
Complications
Complications related to BPA are summarised in Table 5. Injury caused by wire perforation or interruption of the diseased vessel occurred in 3.3% of all BPA procedures. Lung injury was observed in 6.4% of all procedures. Severe complications requiring tracheal intubation with mechanical ventilation occurred in 2 patients (0.8%). In 12 cases (1.1%), non-invasive positive pressure ventilation was used. In 9 cases (0.8%), prolonged balloon catheter inflation was used to treat pulmonary artery perforation. One patient was treated with embolisation of the ruptured pulmonary artery. In one case, a covered stent was used to treat pulmonary artery rupture, as reported elsewhere. Contrast-induced nephropathy (CIN) occurred in 30 cases (2.8%), and one patient required transient haemodialysis, resulting in recovery of renal function.

Survival
A total of 18 patients (7.6%) died during the study period. Four patients (1.7%) died within the first 30 days after BPA due to procedural complications. Fourteen patients died during the follow-up period. Overall survival among 236 patients was 97.3% (95% CI: 94.6%–98.8%), 93.4% (95% CI: 92.4%–96.8%), and 92.4% (95% CI: 87.6%–94.9%) 1, 2, and 3 years after the initial BPA procedure, respectively (Figure 1A). Overall survival after the final BPA among 156 patients was 98.3% (95% CI: 96.5%–99.6%), 96.5% (95% CI: 96.3%–98.1%), and 95.2% (95% CI: 94.2%–95.5%) at 1, 2, and 3 years, respectively (Figure 1B).

Figure 1. Long-term survival after balloon pulmonary angioplasty (BPA). A) Survival from the initial BPA procedure in all registered patients (n=236). B) Survival from the last BPA procedure in patients for whom BPA was terminated (n=156).
Discussion
We report the first results of the multicentre registry of CTEPH patients treated with BPA in Poland. Our study design was based on the first multicentre BPA registry published in 2017 by Ogawa et al25. The BPA programme in Poland was supported by multiple contacts with experienced BPA centres in Japan.
Our study population included 236 consecutive patients from eight institutions, which were PH referral centres in Poland with expertise in the management of CTEPH. In contrast to French and German BPA experience, in which treatment is concentrated in one or two high-volume centres1920, the structure of the Polish BPA programme presented in this study was similar to the Japanese programme and characterised by a higher number of centres performing BPA distributed throughout the country. However, the phenotype of Polish CTEPH patients who underwent BPA was distinctly different from that reported by Ogawa et al. Whilst the Japanese population included 80% females presenting with a low number of concomitant diseases, the Polish population consisted of nearly equal male to female prevalence, with a much higher proportion of comorbidities. Our population was the oldest of those described in the largest BPA series (67±14 vs 61±12.5 years in Japan25; 65 years, range 55–74 years in Germany19; and 63±14 years in France20). Our patients had higher body mass index (27.4±5.3 vs 22.3±3.4 kg/m2) than the Japanese patient population25 and presented a significant number of conditions predisposing for CTEPH. A similar number of Polish and Japanese patients suffered from psychiatric disorders (7.1% in Japan and 7.6% in Poland). In the presented study, depression was the main disorder, and all the patients received medications, primarily selective serotonin reuptake inhibitors. Whereas only 15.3% of Japanese CTEPH patients had a history of previous APE25, 80% of patients in our study had a history of APE, which is much closer to data presented in other large series of CTEPH patients320. Similar to the Japanese population, nearly 70% of Polish CTEPH patients were treated with at least one PH-specific medication at baseline. In comparison, the use of this treatment was slightly lower in France (62%)20 and much higher in Germany (92%)19.
According to the data captured by our registry, BPA treatment resulted in a significant improvement in functional capacity, biomarkers, and haemodynamics. However, the reduction in mPAP was not as remarkable (30.1±10.2 mmHg at short-term follow-up for 156 patients) as that reported in the Japanese registry, in which PAP reached near normal values (22.5±5.4 mmHg at follow-up for 196 patients)25. In the German data set, the final post-procedural mPAP was 33 mmHg19, and in the French study it was reported to be 31.6 mmHg20. Moreover, these less satisfying results in Europe have been achieved despite a higher number of median BPA procedures per patient (4.5 in Poland, 5 in Germany19 and France20 vs 4 in Japan25). The patients’ characteristics in the Japanese experience suggest less advanced CTEPH and fewer comorbidities. Other factors may have contributed to the differences observed in the procedural outcomes. Recently, a study comparing the vascular phenotypes of European and Japanese CTEPH patients on the basis of an analysis of surgical PEA specimens and corresponding plasma demonstrated additional factors that may be a determinant of differential treatment outcomes. Finally, differences in distal pulmonary vasculature involvement between the Japanese and European populations would be difficult to verify.
We noted fewer periprocedural complications after BPA treatment compared to the Japanese registry, with a lower rate of lung injury (6.4% in the Polish registry vs 17.8% in the Japanese registry25) and less severe deterioration requiring intubation and mechanical ventilation (0.8% in the Polish registry vs 5.5% in the Japanese registry25). Our results are closer to the experience reported by the German and French groups, in which lung injury occurred in 9.4%19 and 9.1%2026 of all sessions, respectively. This is important, especially in view of higher baseline PAP pressures and PVR, which were reported to increase the procedural risk of BPA. Brenot et al demonstrated that patients with lung injury had significantly higher baseline mPAP (OR 1.08, 95% CI: 1.039–1.130; p<0.001) and pulmonary vascular resistance20. Procedural success and risk of death may depend on lesion characteristics and BPA technique27.
This is another potential explanation of the higher complication rate reported in the Japanese registry, as Japanese teams enrolled patients earlier than the European centres, which could have benefited from cumulative experience with BPA. Alternatively, the higher complication rate may be due to more aggressive interventions performed by Japanese teams, which could also explain their higher haemodynamic efficacy.
Similar to the Japanese registry and other European centres, we observed low periprocedural (30-day) mortality (1.7% in the Polish registry vs 2.4% in the Japanese registry25, 2.3% in the French study20, and 1.8% in the German study19). In our registry, 4 patients died during the periprocedural period; 3 died within 24 hrs of BPA, 2 due to severe lung injury caused by vascular injury and 1 due to pulmonary oedema despite intubation and mechanical ventilation, and 1 patient died on the seventh day after BPA due to haemorrhagic necrosis in the lobe treated with BPA, which has been described elsewhere13. Fourteen patients died during the follow-up period, mostly due to infectious disorders (pneumonia, urosepsis) and deterioration of right ventricular failure.
To increase patient safety, exclusion of significant coronary artery disease before BPA treatment in elderly patients and patients with multiple risk factors for atherosclerosis is justified28. We found a high proportion of advanced coronary artery disease in patients aged >75 years who were successfully treated with BPA29.
We found that overall survival at three years was comparable to other BPA series (92.4% in the Polish registry vs 94.5% in the Japanese registry25 and 95.1% in the French study20). An indirect comparison to PEA results collected in the pre-BPA period and referring to operable patients is reassuring. In-hospital mortality of PEA was 4.7% in the multicentre CTEPH registry, though it was even lower in high-volume single centres30. Surgery decreased mortality with estimated survival of 93%, 91%, and 89% at 1, 2, and 3 years, respectively.
Limitations
This study has some limitations. First, this study was conducted partly as a retrospective single country registry. Second, 33% of patients in our registry presented with lesions accessible for PEA but were not operated on due to a high risk-benefit ratio and patient refusal. Though these subgroups represent a real-life target for BPA, this intervention may be less effective and riskier when performed in the presence of proximal CTEPH lesions. This may have had a significant impact on the final outcomes reported in our registry. Third, the study presented a short-term follow-up, with a small number of patients evaluated in the long term. Long-term outcomes of BPA treatment should be confirmed in a global multicentre prospective registry, which is currently ongoing (NCT03245268). Fourth, because of the limited number of patients and different distributions among centres, we could not analyse the data from each institution separately. Details on the BPA procedure varied between centres regarding the utilisation of intravascular imaging and pressure wire14. In addition, centres did not use the same protocol to describe lesion characteristics and the level of obstruction. The present data include all BPA procedures from the initial introduction at each PH referral centre. Thus, results may be different with more BPA experience, which would be reflected in different learning curves at each institution. Finally, we did not analyse the impact of PH-specific pharmacotherapy on BPA effectiveness, which would result in a better evaluation of the respective and potentially complementary roles of medical therapy and BPA.
Conclusions
In conclusion, we report the first multicentre registry in Europe, which confirmed that BPA is a safe and effective therapeutic option in patients with CTEPH who are not suitable for PEA. Our results acknowledge some of the differences in patient characteristics and outcomes of BPA treatment between Europe and Japan. However, we confirmed that BPA significantly improves symptoms, exercise capacity, biochemical parameters, and haemodynamics in inoperable CTEPH patients. Periprocedural mortality was low. Lung injury was the main periprocedural complication, but occurred at an acceptably low frequency. Long-term effects of BPA need to be adequately evaluated in a prospective, multicentre study.
Acknowledgements
We are indebted to Hiromi Matsubara, Shigefumi Fukui, Yu Taniguchi, Toru Satoh, and their groups for invaluable advice and support during the implementation of the BPA programme in Poland.
Conflict of interest statement
S. Darocha and G. Kopeć have received grants and personal fees from Janssen-Cilag, MSD, Bayer, and AOP Orphan. K. Jonas has received grants and personal fees from Janssen-Cilag and MSD. A. Araszkiewicz has received grants and personal fees from MSD and Bayer. A. Torbicki has received speaker’s and consultancy honoraria from Janssen-Cilag, Bayer and MSD. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.