Abstract
Aims: Balloon pulmonary angioplasty (BPA) improves haemodynamics and exercise capacity in patients with chronic thromboembolic pulmonary hypertension (CTEPH). However, even after BPA many patients still suffer from exertional dyspnoea. Our aim was to clarify the clinical validity of extensive revascularisation by BPA (ERBPA) beyond haemodynamic normalisation.
Methods and results: Thirty-five CTEPH patients with normalised or borderline mean pulmonary arterial pressure (mPAP) after BPA were retrospectively analysed. We evaluated the clinical efficacy of an ERBPA strategy in 15 patients (ERBPA group) by comparing with the natural course of 20 patients who could be followed without additional BPA (conventional BPA group). ERBPA reduced the number of pulmonary arterial segments with residual stenoses from 11.7±0.4 to 5.3±0.5 segments. Symptoms, six-minute walking distance, and VE/VCO2 slope were significantly improved in the ERBPA group but not in the conventional BPA group, which indicated that this improvement was due to ERBPA and not merely a natural progression after haemodynamic normalisation. Complications associated with ERBPA were fewer than those of the initial BPA therapy.
Conclusions: ERBPA targeting residual stenoses can safely ameliorate symptoms and exercise capacity by additional improvement of haemodynamics. The results encourage us to optimise the current BPA goal to be more aggressive.
Abbreviations
BPA: balloon pulmonary angioplasty
CTEPH: chronic thromboembolic pulmonary hypertension
ERBPA: extensive revascularisation of BPA
PEA: pulmonary endarterectomy
PVR: pulmonary vascular resistance
RHC: right heart catheterisation
RPI: reperfusion pulmonary injury
Introduction
Pulmonary endarterectomy (PEA) is the gold standard therapy for chronic thromboembolic pulmonary hypertension (CTEPH), and balloon pulmonary angioplasty (BPA) is an alternative treatment option for patients with distal-type CTEPH1. The first report (in 2001) about BPA by Feinstein et al2 showed significant reduction of mPAP from 42±12 to 33±10 mmHg. In 2012, a refined BPA was introduced achieving a decreased mPAP (24 mmHg)3. Recent studies have tended to show further aggressive reduction of mPAP (21~23 mmHg)1,4,5.
The indication for BPA is now recommended in the following two situations: 1) non-operable CTEPH2, and 2) residual pulmonary hypertension (PH) after PEA6. However, it is not yet clear how we should set the endpoint of BPA. Lewczuk et al reported that patients with mPAP over 30 mmHg had a poorer prognosis than patients with mPAP under 30 mmHg7. Moreover, we have experienced many patients who still suffer from persistent exertional dyspnoea accompanied by residual stenoses despite normalisation of mPAP. Persistent stenosis after PEA was reported to be a cause of persistent symptoms8.
The aim of this study was to clarify the efficacy and safety of extensive revascularisation by BPA (ERBPA) by evaluating haemodynamics, exercise capacity, symptoms, and complications. If this approach is proven to be effective, a new therapeutic endpoint will be established for patients with not only CTEPH but also chronic thromboembolism without PH.
Methods
The Ethics Committees in Kobe University Hospital accepted the study protocol.
EXTRACTION OF STUDY POPULATION
A total of 122 patients were diagnosed with CTEPH from July 1999 to July 2016 in Kobe University Hospital (Figure 1). Nineteen patients received medical management only. PEA was performed for 44 patients and BPA was performed for 59 patients. Twelve patients were unable to reach an mPAP value of less than 25 mmHg for several reasons: 1) refusal of further BPA due to severe complications at a previous session, 2) end-stage renal disease, 3) advanced age, 4) multiple unsuitable lesions for BPA, 5) existence of malignant cancer. From the initiation of BPA in March 2011, we set the endpoint as normalisation of mPAP defined as less than 25 mmHg (conventional BPA group). We modified the endpoint from haemodynamic normalisation to revascularisation of all remaining stenoses as much as possible regardless of mPAP from November 2014 (ERBPA group). Four patients in the ERBPA and eight patients in the conventional BPA group were excluded due to absence of follow-up right heart catheterisation (RHC). Finally, 20 patients were analysed as the conventional BPA group, and 15 patients as the ERBPA group.
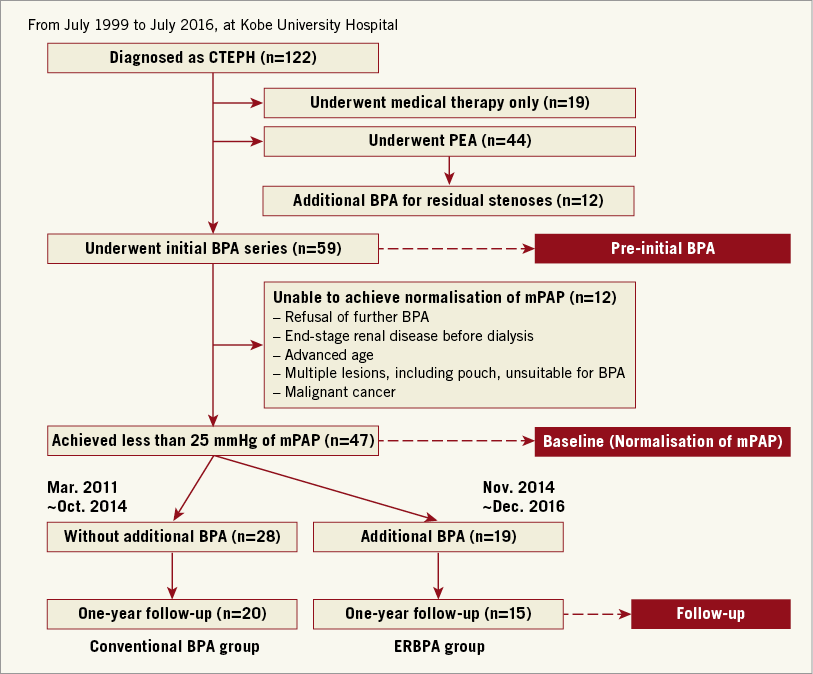
Figure 1. Study flow chart. The ERBPA (extensive revascularisation by BPA) group is compared with the conventional BPA group retrospectively.
BPA PROCEDURE
The BPA procedure was described in our previous reports1,9. We utilised mainly the femoral vein approach and inserted a 6 Fr guiding sheath into the main pulmonary artery. Through the guiding sheath we engaged a 6 Fr guiding catheter (Profit®; Goodman, Nagoya, Aichi, Japan) into the target sectional branch and passed a 0.014 inch guidewire (Athlete Bpahm®; Japan Lifeline, Tokyo, Japan). After we assessed the diameter and lesion type by using intravascular ultrasound (IVUS), we dilated vessel lesions with a 2.0-7.0 mm monorail balloon. In each hospitalisation we performed two sessions of BPA and RHC one week after the latest session to evaluate the efficacy.
CLINICAL PARAMETERS
Haemodynamics, exercise capacity, lung function, and WHO functional class were evaluated at three points: 1) pre-initial BPA, 2) baseline (when mPAP was normalised), and 3) follow-up (more than three months after the final procedure). During each pulmonary angiography procedure, vessel lesions were classified according to the Japan Circulation Society criteria: web, band, abrupt narrowing, complete vascular obstruction, and pouch. We counted the number of pulmonary arterial segments involving at least one lesion including subsegmental branches. Six-minute walking test and cardiopulmonary exercise test were performed to assess exercise capacity. Clinical events from baseline were monitored until December 2016.
OCCURRENCE OF REPERFUSION PULMONARY INJURY
We routinely performed chest X-ray and CT within 24 hours after each BPA session, and reperfusion pulmonary injury (RPI) was assessed by at least two cardiologists and one radiologist. Occurrence rates of haemosputum, non-invasive positive pressure ventilation (NPPV), and intubation were evaluated.
STATISTICAL ANALYSIS
Continuous variables were represented as mean±standard error. Differences between the groups were analysed by unpaired t-test. Differences between “baseline” and “follow-up” were statistically compared using the paired t-test. Chi-square tests were utilised for comparison between categorical variables. The Wilcoxon signed-rank test and Mann-Whitney test were used in cases of paired and unpaired comparisons for WHO-FC. A p-value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS statistics, Version 17.0 (SPSS Inc., Chicago, IL, USA).
Results
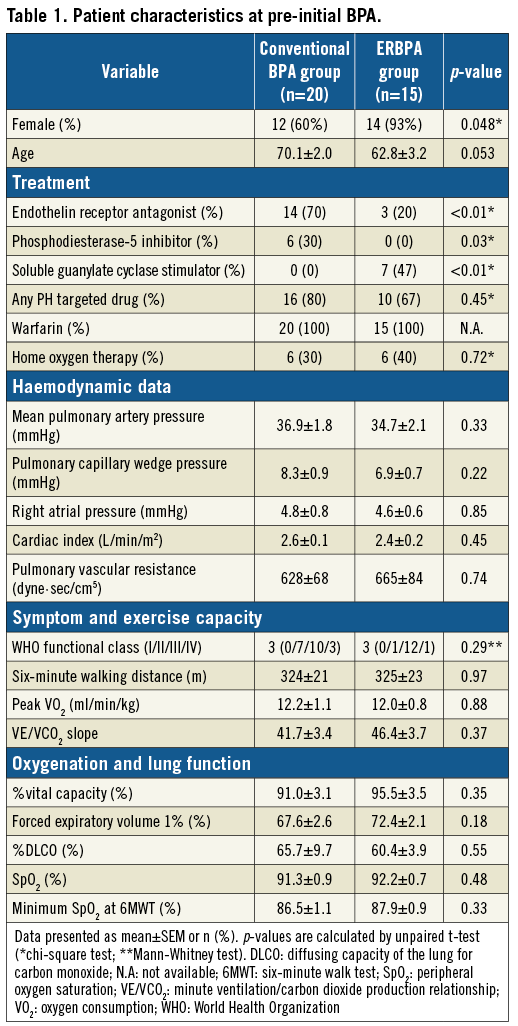
CHARACTERISTICS AT PRE-INITIAL BPA
Characteristics at pre-initial BPA are summarised in Table 1. Although the ERBPA group was female-dominant and younger on average than the conventional BPA group, there were no significant differences in haemodynamics, exercise capacity, symptoms, lung function, and oxygenation between the groups. All patients received more than six months of anticoagulant therapy. Soluble guanylate cyclase stimulator (sGCs) was first approved for CTEPH in January 2014 in Japan. As such, endothelin receptor antagonist (ERA) and phosphodiesterase type 5 inhibitor (PDE5i) as off-label drugs were more frequently prescribed in the conventional BPA group, whereas sGCs were more frequently prescribed in the ERBPA group. However, the percentage of patients with PH targeted drugs was similar between the groups.
ALTERATION OF CLINICAL PARAMETERS AND PROGNOSIS FROM BASELINE TO FOLLOW-UP
No cardiovascular-related events or death occurred from baseline except for a patient in the conventional BPA group who passed away due to acute myeloid leukaemia.
The time course of each parameter is shown in Figure 2, Table 2, and Table 3. The duration from pre-initial BPA to follow-up (conventional BPA vs. ERBPA: 70.7±4.9 vs. 65.2±8.0 weeks; p=0.55) (Table 2) and baseline to follow-up (conventional BPA vs. ERBPA: 51.7±4.9 vs. 52.1±6.5 weeks; p=0.96) was not different between the groups. From baseline to follow-up, an ERA in the conventional BPA group and a PDE5i in the ERBPA group were discontinued. Home oxygen therapy was initiated in two patients in the conventional BPA group and in four patients in the ERBPA group. In spite of minor alterations of the treatment, no statistical significance with regard to non-invasive therapy (PH targeted drug, warfarin, home oxygen therapy) was observed between the groups. The number of involved pulmonary arterial segments was significantly reduced only in the ERBPA group (11.8±0.4 vs. 5.3±0.6 segments; p<0.01) (Table 2), which provided significant improvement in haemodynamics (mPAP: 20.4±0.7 to 17.9±0.9 mmHg; p<0.01, pulmonary vascular resistance [PVR]: 348±39 to 234±18 dyne·sec/cm5; p<0.01) (Figure 2), exercise capacity (peak VO2: 14.2±1.1 to 17.3±1.2 ml/min/kg; p=0.05, and VE/VCO2 slope: 41.5±3.4 to 30.4±1.0; p=0.04) (Table 3, Figure 3). We were unable to observe improvement in resting cardiac index and lung function including diffusing capacity of the lung for carbon monoxide (%DLCO) and oxygenation parameters (SaO2: 94.1±0.8 to 94.8±0.9%; p=0.62) (Table 3). At the time of follow-up, all patients in the ERBPA group improved their WHO-FC with no patients remaining in a class of more than WHO-FC III (Figure 4). In contrast, five patients did not improve at follow-up and three patients remained in WHO-FC III in the conventional BPA group.
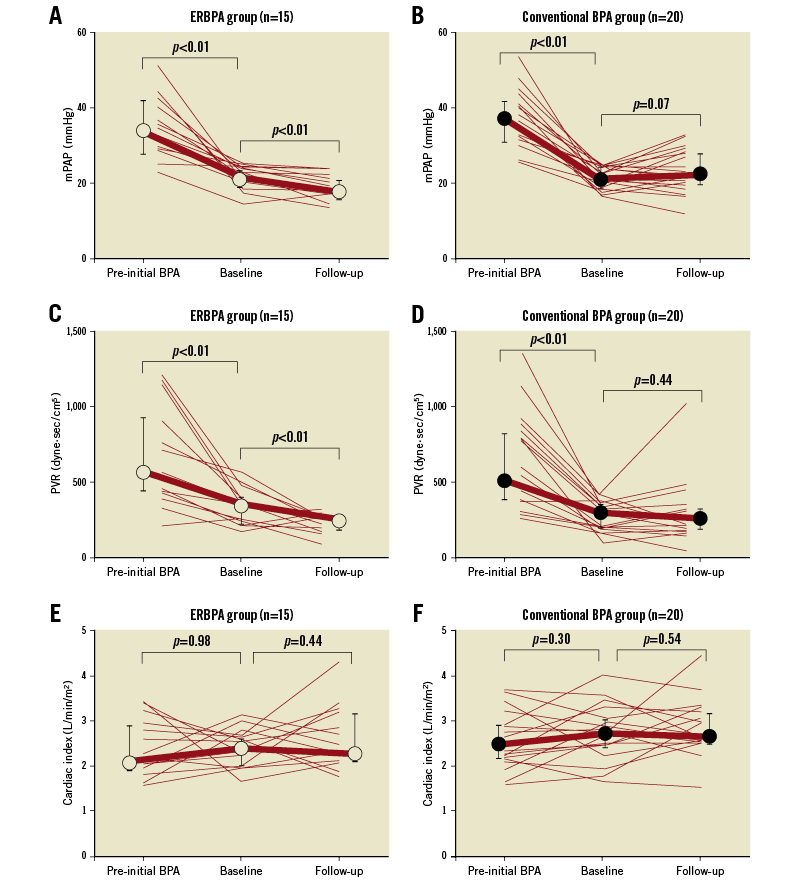
Figure 2. Time course of haemodynamic changes during the study period. Between baseline and follow-up, mPAP and PVR are significantly improved only in the ERBPA group, but not in the conventional BPA group. The values are expressed as median (○ or ●) and interquartile range (bar).
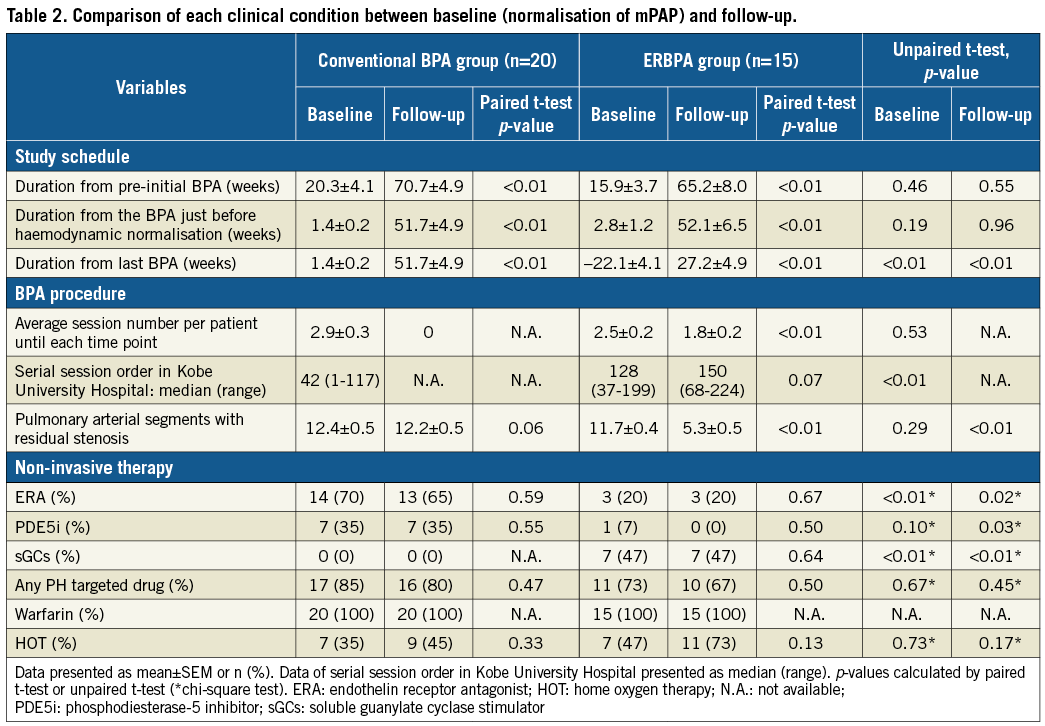
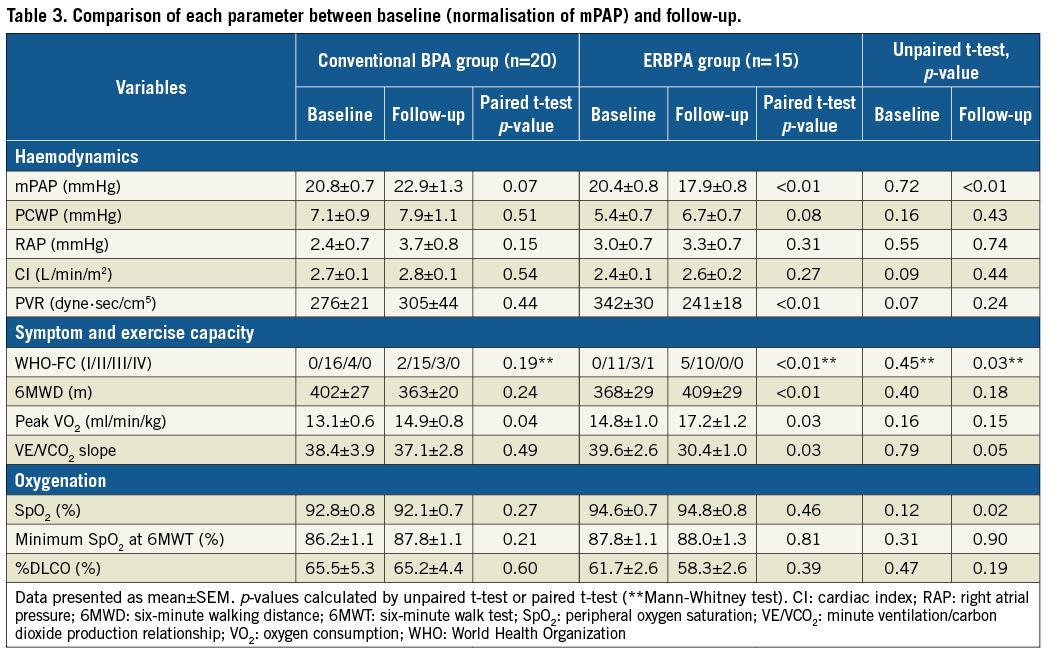
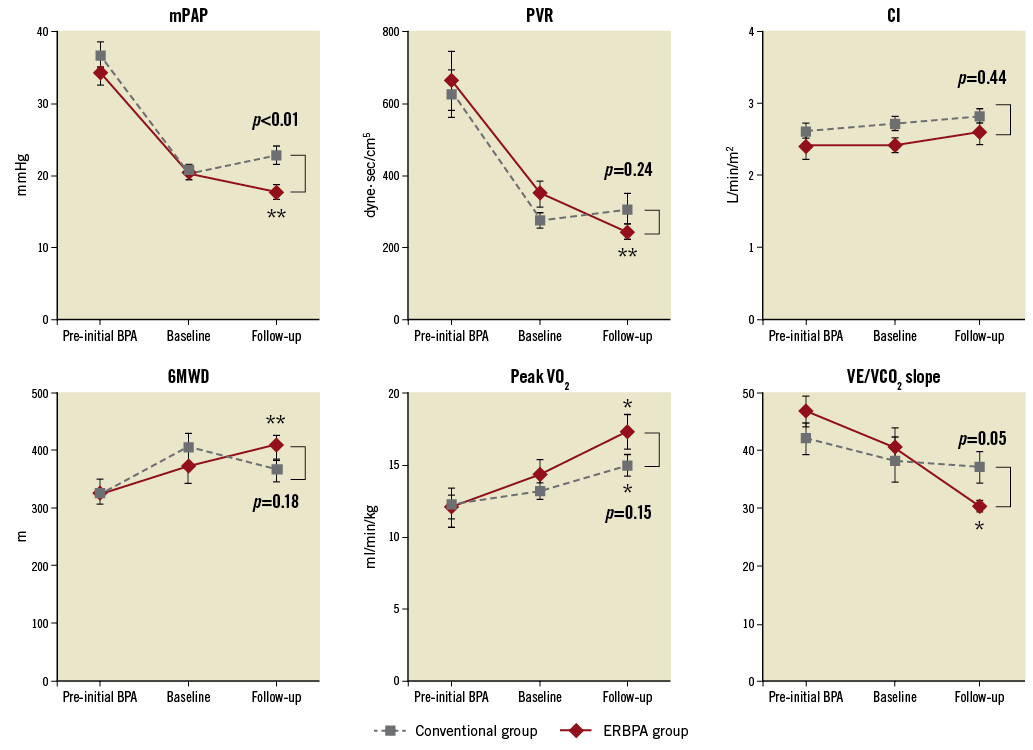
Figure 3. Comparison between ERBPA and conventional BPA groups in haemodynamics and exercise capacity. Despite no significant differences between the groups at pre-initial BPA and baseline, ERBPA significantly improves mPAP, PVR, 6MWD, peak VO2, and VE/VCO2 slope in contrast to the conventional BPA group from baseline to follow-up. * p<0.05 vs. baseline in the same group. ** p<0.01 vs. baseline in the same group.
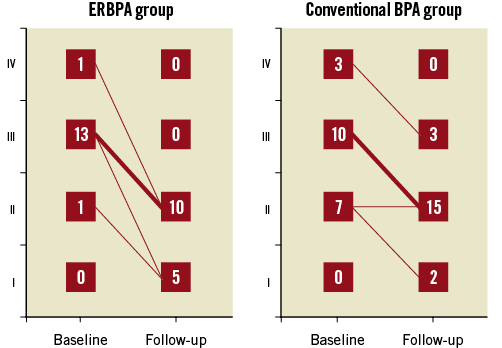
Figure 4. Changes in WHO functional class. The number of patients is expressed at each time point.
FEATURES OF TARGET LESIONS AND COMPLICATIONS WITH ERBPA
Table 4 shows a comparison of treated branches and complications between the initial BPA series (until normalisation of mPAP) and ERBPA (after normalisation of mPAP). The most frequently observed lesions were web type, and the distribution of lesion types was similar in both groups. We avoided treating pouch lesions because of the risk of wire injury. There was a significantly reduced incidence of RPI in ERBPA compared with initial BPA therapy. As a result, the incidence of haemosputum and necessity of NPPV were significantly lower in ERBPA, and there were also no instances of intubation and death with ERBPA.
A REPRESENTATIVE CASE OF ERBPA
A representative case of a 57-year-old female who underwent ERBPA for residual pulmonary arterial stenoses in the right upper lobes is shown in Figure 5. After we treated vessel lesions in bilateral lower lobes by initial BPA sessions twice, mPAP was normalised and perfusion deficits at the site reflected in the iodine map detected by dual energy computed tomography (CT) were found to have improved. After performing additional dilatation of the residual stenoses in the right upper lobe as ERBPA, the patient further improved in haemodynamics (mPAP 22.0 to 16.2 mmHg), exercise capacity (6MWD 350 to 430 m, peak VO2 12.9 to 16.2 ml/min/kg), and symptoms (WHO-FC II to I).
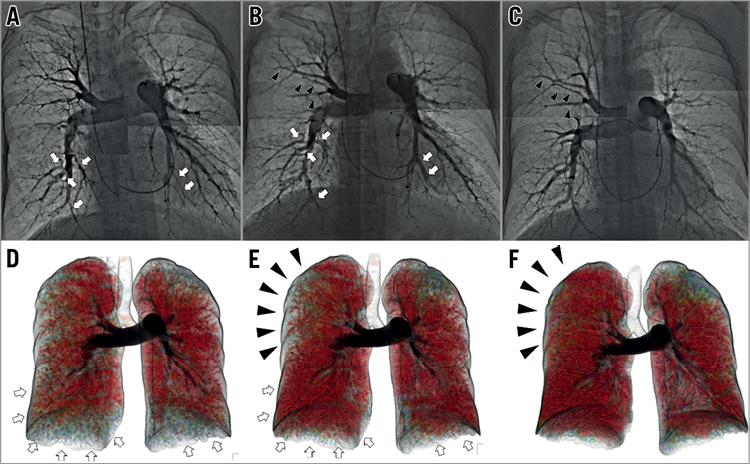
Figure 5. Pulmonary angiography and iodine map in dual energy CT in a representative case. At pre-initial BPA, perfusion deficits were observed at bilateral inferior and upper lobes (D). Normalisation of mPAP was achieved after two sessions of BPA to lower lobes (A & B, white arrows) resulting in improvement of perfusion (D & E, white arrows). ERBPA by the 3rd and 4th sessions of BPA was performed targeting the residual stenosis (B & C, black arrowheads) at right upper lobes, and improved the perfusion (E & F, black arrowheads).
Discussion
This is the first study clarifying the efficacy of ERBPA coupled with additional dilatation of the remaining stenoses after haemodynamic normalisation. ERBPA safely improved haemodynamics, resulting in expanded exercise capacity in contrast to no improvement in the conventional BPA group.
AN ADDED EXERCISE IMPROVEMENT RESULTED FROM ERBPA ABOVE NATURAL PROGRESSION
Previous reports have shown a natural progression of exercise capacity until two years after PEA10,11. We also observed significant improvement in peak VO2 and a slight improvement in VE/VCO2 slope in the conventional BPA group during the follow-up period (Figure 3). However, if we compare the ERBPA and conventional BPA groups at follow-up, the ERBPA group demonstrated a better VE/VCO2 slope, which is known to be a more specific marker for CTEPH12, than the conventional BPA group. During follow-up, significant improvement of haemodynamic parameters was observed only in the ERBPA group but not in the conventional BPA group. These data suggested that an added exercise improvement was indeed due to ERBPA and not merely a natural progression seen in the conventional BPA group after haemodynamic normalisation (Figure 3).
MECHANISM OF IMPROVED EXERCISE CAPACITY BY ERBPA
We could still detect residual stenoses in many pulmonary arterial segments even after mPAP was normalised. The average number of involved segments after haemodynamic normalisation was around 11-12 (Table 2), which is equal to two thirds of a total of 18 segments in the lung. This highlighted the fact that setting a value of the mPAP to be less than 25 mmHg alone is too passive a goal to enable full recovery of pulmonary blood flow. Residual stenoses will induce ventilation-perfusion mismatch, thereby promoting dead space ventilation. Even though there are no symptoms at rest, residual stenoses are apparent as dyspnoea when the ventilator requirement is increased upon exercise.
Furthermore, Bonderman et al reported that residual stenoses could be a cause of excessive elevation of right ventricular afterload at exercise13. They elegantly pointed out an abnormal pulmonary haemodynamic response to exercise in patients with persistent exertional dyspnoea even after successful PEA. PVR in the patients is increased although healthy subjects show decreased PVR during exercise. In other words, cardiac index (CI) at exercise is a more sensitive index to predict exercise capacity compared to resting CI. Although we observed the discrepancy of longitudinal changes between non-significant alteration of resting CI and progressive 6MWD increase after BPA (Figure 3), this discrepancy is acceptable because peak VO2, which reflects exercise CI, provided a convincing correlation with 6MWD. As such, the promotion of dead space ventilation and abnormal elevation of right ventricular afterload would be the pathophysiological mechanism derived by residual stenoses, which could be a cause of persistent exertional dyspnoea. The approach by ERBPA to enable full recovery of pulmonary perfusion regardless of mPAP could be a novel strategy to relieve the persistent symptoms.
SAFETY AND EFFICACY OF ERBPA
We clearly demonstrated that the occurrence of RPI was significantly reduced in ERBPA compared with the initial BPA therapy (Table 4). Previously, the suggested associated factors for RPI were lesion type5, a learning curve3, and haemodynamics2,9.
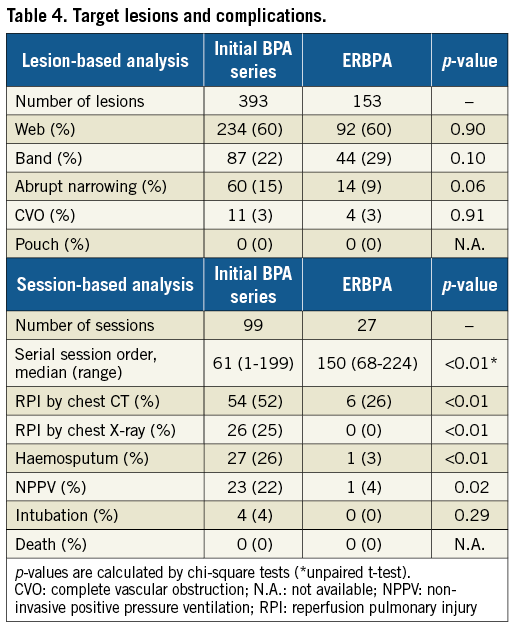
The lesions such as subtotal and total occlusion were reported to have a higher risk of wire injury than other lesions5 due to difficulty of wire passage and vulnerability of peripheral vessels. Our target had no significant differences in lesion type between ERBPA and the initial BPA series, suggesting that the reduced frequency of RPI incidence was free from lesion types of target.
Haemodynamic factors are another risk for RPI which frequently occurred in patients with over 35 mmHg of mPAP2. In addition, we have reported that the cut-off value for RPI is 19.5 mmHg of mPAP at a lesion distal to the stenoses9. We assumed that the pressure in ERBPA should be lower than in the initial BPA series. Although we could not rule out the effect of a learning curve, this may explain why the severity of RPI in addition to the frequency was significantly lower in the ERBPA group (Table 4).
THE EFFECT ON OXYGENATION OF ERBPA
Although the initial BPA series improved oxygenation, ERBPA alone could not induce further improvement in oxygenation both at rest and during exercise (Table 3). There are two possible reasons for this observation.
First of all, Aoki et al reported that BPA improved oxygenation by reducing intrapulmonary shunt4. A reduced degree of intrapulmonary shunt by BPA became more apparent when the patients had more severe haemodynamics. Certainly, the depressor effect of mPAP by ERBPA was slight compared to the initial BPA series. As a result, improvement of intrapulmonary shunt may be insufficient to contribute significantly to an improvement in oxygenation. The second possible reason is that exercise-induced decrease in oxygenation was paralleled by a decrease in mixed venous oxygen tension as a consequence of an insufficient cardiac output response13. Residual lesions even after ERBPA were still present in approximately five segments (Table 2), which may cause an insufficient increase in cardiac output and reduction in SvO2. The synergistic effect of the above factors hindered improvement of oxygenation at rest and during exercise. There is a possibility that further treatment of residual lesions might enable full recovery of oxygenation, but further investigations are warranted.
Limitations
There are some limitations of this study. Firstly, this is a retrospective and observational study in a single centre that necessitates some caution in the interpretation of data. As shown in Table 1, there were also some differences in patient characteristics including age and gender, as well as some discrepancy with regard to the duration of follow-up between the groups, introducing problems associated with a learning curve and possible confounding between the groups. The registered case number was not large enough. Furthermore, components of oral medication varied between the two groups. In particular, riociguat was prescribed more frequently in the ERBPA group. We cannot rule out the possibility that these factors may have influenced the results. Therefore, ideally the findings from this study should be confirmed in a multicentre prospective study.
Secondly, residual stenoses and obstructions remained in patients even after ERBPA. We could not always pass the guidewire through the hard ostial pouch lesions. In general, there are some technical difficulties with regard to the anatomical approach to the left upper lobe and distal lesions beyond subsegmental branches. Even though the final pulmonary blood perfusion was not complete, we would like to emphasise the importance of correcting lesions to the best of our ability, so as to enable substantial improvement of every patient’s symptoms and exercise capacity.
Thirdly, we did not have a strategy to prioritise target selection for ERBPA. It is difficult to assess accurately the volume of pulmonary vascular bed distal to the lesion. We treated the accessible lesions as much as possible. However, if we could precisely predict the treatable vascular bed volume depending on each target, the strategy of ERBPA could be more sophisticated.
Conclusions
We clarified that an ERBPA strategy significantly enhanced exercise capacity compared with the conventional BPA approach by improving haemodynamics, with fewer complications. It would be ideal if the new goal for patients with CTEPH is set to relieving residual stenoses regardless of mPAP.
| Impact on daily practice The present study demonstrated the therapeutic possibility of extensive revascularisation by BPA aiming for full recovery of pulmonary blood flow. The residual stenoses in pulmonary arteries could be a cause of exertional dyspnoea even after conventional invasive therapy. It is thus desirable to set therapeutic goals to dilate the remaining lesions in pulmonary arteries as much as possible for CTEPH. |
Conflict of interest statement
K. Nakayama has received research grants from Actelion Pharmaceuticals Japan Ltd. and Bayer Holding Ltd. K.I. Hirata has received research grants from Actelion Pharmaceuticals Japan Ltd., and Bayer Holding Ltd. The other authors have no conflicts of interest to declare.