Balloon pulmonary angioplasty (BPA) is efficacious in the treatment of chronic thromboembolic pulmonary hypertension (CTEPH)1,2. Lesions of CTEPH are categorised by their characteristic appearance on pulmonary angiography3. While there are studies using intravascular ultrasound (IVUS)-guided BPA for inoperable CTEPH1, there are currently no established procedures specifically for chronic totally occluded (CTO) lesions.
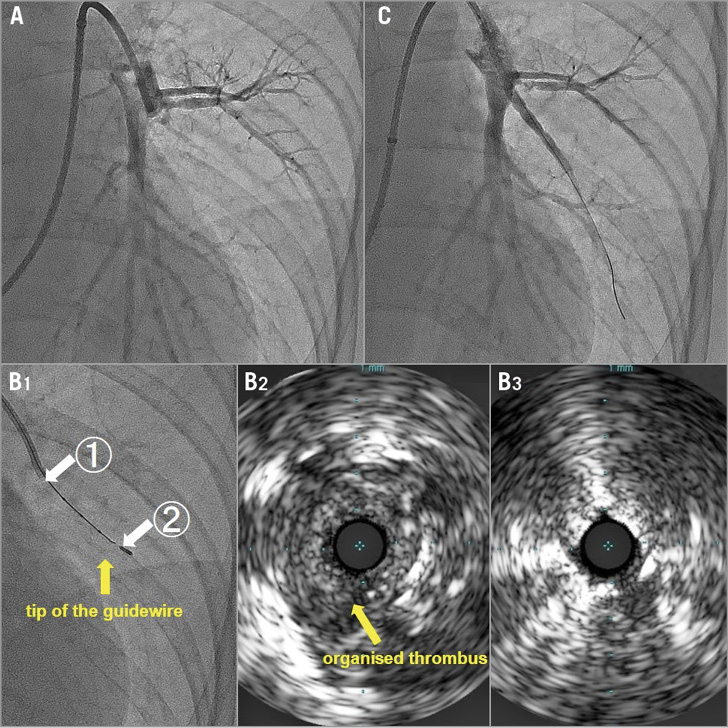
The patient was a 66-year-old female. Pulmonary artery angiography with a Profit 6 Fr JL4 guide catheter (Goodman, Aichi, Japan), anteroposterior straight view, showed CTO of the left inferior lingual artery (Panel A). A 190 cm guidewire (Chevalier® 14 tapered 30; Cordis, Cardinal Health, Tokyo, Japan) was advanced slightly into the organised thrombus while guiding with IVUS using an Eagle Eye® Platinum ST catheter (Philips, Amsterdam, the Netherlands) along the guidewire. We confirmed the location of the IVUS catheter within the organised thrombus (Panel B2, image of position ![]() on Panel B1) and continued to advance it while maintaining the position of the guidewire (Moving image 1, Moving image 2).
on Panel B1) and continued to advance it while maintaining the position of the guidewire (Moving image 1, Moving image 2).
When the location of the IVUS catheter in the true lumen of the vessel was confirmed, it was further advanced through the CTO into the distal true lumen (Panel B3, image of position ![]() on Panel B1). The lesion was then dilated with a 4 mm balloon catheter. With the preceding technique using IVUS, we could complete the BPA of the CTO (Panel C). No side effects were noted with this procedure.
on Panel B1). The lesion was then dilated with a 4 mm balloon catheter. With the preceding technique using IVUS, we could complete the BPA of the CTO (Panel C). No side effects were noted with this procedure.
The spherical tip of the IVUS catheter and the imaging distance of the tip of only 2.5 mm allowed the identification and advancement of the IVUS catheter through the true vessel. The risk of perforating the pulmonary artery is low using this technique. We could also reach the true lumen using this procedure despite poor peripheral blood flow immediately after the BPA. However, since the thickness of the layer of organised thrombus is unique to each lesion, the IVUS catheter may not pass through some lesions where the thrombus is too thick. The rigidity of the Eagle Eye catheter might also preclude its use in severely tortuous vessels, but its use in straight vessels makes it more suitable. The guidewire requires a certain degree of stiffness to support the IVUS catheter.
The authors have performed five cases using this procedure with a success rate of 80% and no significant morbidity or mortality. With careful patient selection, IVUS-guided BPA can serve as an alternative treatment of choice in approaching lesions with CTO in patients with CTEPH.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Preceding IVUS into the CTO lesion.
Moving image 2. IVUS image during the procedure.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Preceding IVUS into the CTO lesion.
Moving image 2. IVUS image during the procedure.