Abstract
Aims: We aimed to appraise the predictive accuracy of a novel and user-friendly risk score, the ACEF (age, creatinine, ejection fraction), in patients undergoing PCI for coronary bifurcations.
Methods and results: A multicentre, retrospective study was conducted enrolling consecutive patients undergoing bifurcation PCI between January 2002 and December 2006 in 22 Italian centres. Patients with complete data to enable computation of the ACEF score were divided into three groups according to tertiles of ACEF score. The primary endpoint was 30-day mortality. The discrimination of the ACEF score as a continuous variable was also appraised with area under the curve (AUC) of the receiver-operating characteristic. A total of 3,535 patients were included: 1,119 in the lowest tertile of ACEF score, 1,190 in the mid tertile, and 1,153 in the highest tertile. Increased ACEF score was associated with significantly different rates of 30-day mortality (0.1% in the lowest tertile vs. 0.5% in the mid tertile and 3.0% in the highest tertile, p<0.001), with similar differences in myocardial infarction (0.3% vs. 0.7% and 1.8%, p<0.001) and major adverse cardiac events (MACE, 0.5% vs. 1.2% and 4.3%, p<0.001). After an average follow-up of 24.4±15.1 months, increased ACEF score was still associated with a higher rate of all-cause death (1.3% vs. 2.4% and 11.0%, p<0.001), cardiac death (0.9% vs. 1.4% and 7.2%, p<0.001), myocardial infarction (3.4% vs. 2.7% and 5.7%, p<0.001), MACE (13.6% vs. 15.9% and 22.3%, p<0.001), and stent thrombosis (2.3% vs. 1.8% and 5.0%, p<0.001). Discrimination of ACEF score was satisfactory for 30-day mortality (AUC=0.82 [0.77-0.87], p<0.001), 30-day MACE (AUC=0.73 [0.67-0.78], p<0.001), long-term mortality (AUC=0.77 [0.74-0.81], p<0.001), and moderate for long-term MACE (AUC=0.60 [0.57-0.62], p<0.001).
Conclusions: The simple and extremely user-friendly ACEF score can accurately identify patients undergoing PCI for coronary bifurcation lesions at high risk of early fatal or non-fatal complications, as well as long-term fatality.
Introduction
Percutaneous coronary intervention (PCI) is a mainstay in the management of coronary artery disease. Whereas PCI for simple lesions is easily and safely accomplished in most cases, bifurcation lesions, especially when proximally located,1 are more technically demanding and may be associated with adverse events, at both early and long term.2-4
Risk prognostication in patients undergoing PCI has been the subject of several studies, leading to the development and recommendation of several different scores and approaches.5-7 Numerous variables have been proposed in such scores, including admission diagnosis, age, congestive heart failure symptoms, diabetes mellitus, dyslipidaemia, extent of coronary artery disease, gender, lesion complexity, neurologic function, peripheral artery disease, pulmonary disease, renal failure, salvage index, shock, smoking status, and thrombolytic therapy. However, all such scores appear complex, as they include several of the above clinical and procedural variables with individual weights and, occasionally, interaction terms, and thus are only occasionally used in clinical practice.
The parsimonious age, creatinine, ejection fraction (ACEF) score has been tested and validated in the setting of elective coronary artery bypass grafting (CABG), but its role in patients undergoing PCI, despite being very promising, has not been studied thoroughly.8-10 Indeed, the ACEF score appears inherently more appealing than most other available or foreseeable scores given its unique user-friendliness and immediacy. Moreover, no data are available on the usefulness of the ACEF score in patients undergoing bifurcation PCI.
The multicentre I-BIGIS study has already provided several important insights into the management of patients undergoing PCI for coronary bifurcation lesions given its very large sample and current stance.11,12 We hypothesised that the ACEF score can prove to be a very user-friendly yet informative predictive tool for cardiologists managing patients undergoing bifurcation PCI. We thus aimed to test the predictive accuracy of the ACEF score in patients undergoing bifurcation PCI enrolled in the I-BIGIS registry.
Methods
DESIGN
The present work stems from the I-BIGIS study, a large retrospective multicentre Italian registry of patients undergoing bifurcation PCI between 2002 and 2006, which has already been described in detail.11,12 This was a retrospective, observational clinical study sponsored by the Italian Society of Invasive Cardiology (SICI-GISE) and thus no extramural funding was used to support this work. All the Italian catheterisation laboratories constituting the SICI-GISE data set providers were invited to join the registry. Minimum requirements were the routine performance of PCI, DES availability, and presence of a dedicated procedural database throughout the study period. To avoid selection bias or incomplete data reports, centres unable to achieve a complete clinical form rate >90% were also not considered eligible for the registry.
PATIENTS AND PROCEDURES
Percutaneous coronary revascularisation of a bifurcation lesion of a major epicardial vessel (defined as presence of >50% diameter stenosis in a bifurcation with a 2.5-4.5 mm reference vessel diameter in the main branch [MB] and 2.25-4.5 mm in the side branch [SB]) was required for inclusion. Patients underwent blood draws for serum creatinine at admission and left ventricular ejection fraction was assessed by transthoracic echocardiography using the standard Simpson method during hospital stay. Treatment strategies were at the operator’s discretion. Patients were discharged on oral thienopyridines for 3-12 months plus aspirin indefinitely, depending on admission diagnosis as well as stent choice. Patients were followed by direct check of hospital charts, patient visit, phone interview, contact with referring physicians, and/or inspection of local civil registries.
For the purpose of this work, only patients with complete data enabling computation of the ACEF score were included (3,535 [81.9%] subjects out of an initial 4,314 enrolled). These patients had similar baseline and procedural features in comparison to those without complete data to compute the ACEF score. All subjects provided written informed consent and ethical committee approval was waived given the observational design.
Notably, given the number of centres and diversity of local databases we expected issues in data capturing and non-consecutive enrolment. Accordingly, only high-volume centres with detailed and dedicated databases were offered the chance to participate. These databases are used routinely for case reporting and thus capture all salient patient and procedural features, including bifurcation PCI. Thus, data capture was assumed adequate with a very high likelihood of consecutive enrolment. In addition, we systematically and repeatedly queried participating centres in cases of data discrepancies or significant temporal gaps in enrolment, which would have suggested non-consecutive and inhomogeneous data entry.
OBJECTIVES, ENDPOINTS AND DEFINITIONS
We aimed to appraise the predictive role of the ACEF score when exploited as a three-level category (lowest tertile of ACEF score, mid tertile of ACEF score, and highest tertile of ACEF score) and as a continuous variable. The primary endpoint of the study was 30-day mortality. Additional endpoints were long-term mortality, 30-day rate of major adverse cardiac events (MACE, i.e., the composite of death, myocardial infarction [MI], coronary artery bypass grafting [CABG], or target lesion revascularisation [TLR]), and long-term rate of MACE. Myocardial infarction was defined as Q-wave MI in the presence of new pathologic Q-waves on the electrocardiogram in two or more contiguous leads or non-Q-wave MI in the presence of an elevation of creatine-kinase level or its MB isoenzyme to three times or more the normal upper limit. Target lesion revascularisation was defined as any revascularisation procedure (angioplasty, stenting, or CABG) performed because of angiographic restenosis at the site of the treated bifurcation (within the stent or 5 mm proximal or distal to it) associated with clinical and/or objective evidence of inducible myocardial ischaemia. Stent thrombosis rate was assessed using the Academic Research Consortium definition as definite, probable, or possible, and as acute, subacute, late, or very late. Each patient could provide only one hard event per event type, thus avoiding any risk of tautology or redundancy. The ACEF score was computed according to Ranucci et al,8,9 as age (in years) divided by ejection fraction (in %) plus one (if serum creatinine ≥2.0 mg/dL).
STATISTICAL ANALYSIS
Continuous variables are reported as mean±standard deviation and categorical variables as n (%). Continuous variables were compared with analysis of variance for Gaussian variables and Kruskal-Wallis test for non-Gaussian variables (p<0.05 at Shapiro-Wilk test), and categorical variables with the chi-squared test. Logistic regression analysis was used to appraise discrimination (c statistic) of an ACEF-based model to predict 30-day events, as well as independent association with outcomes (reported as odds ratios [OR], with 95% confidence intervals), whereas Cox proportional hazard analysis was used to appraise discrimination (Harrell c-index) of the same model to predict long-term events, as well as independent association with outcomes (reported as hazard ratios [HR], with 95% confidence intervals). The proportional hazards assumption was checked both graphically and by means of scaled Schoenfeld residuals. Confidence intervals (CIs) for the Harrell c-indices were calculated using jackknife variance estimation by means of the “somersd” STATA command. Finally, calibration was appraised comparing observed and expected event rates. SPSS 19.0 (IBM, Armonk, NY, USA) and STATA 11.2 (StataCorp LP, College Station, TX, USA) were used for statistical analyses.
Results
From a total of 3,535 patients with ACEF scores (Figure 1), 1,119 were in the lowest tertile (ACEF score <1.090), 1,190 in the mid tertile (ACEF score between 1.090 and 1.380), and 1,153 in the highest tertile (ACEF score >1.380). Baseline features are reported in Table 1. Several features were significantly different among ACEF tertiles, including age, male gender, family history of coronary disease, hypertension, dyslipidaemia, smoking history, diabetes mellitus, chronic kidney disease, prior myocardial infarction, prior CABG, multivessel coronary disease, unprotected left main disease, ejection fraction, admission diagnosis, and admission to a low-volume centre (all p<0.05).
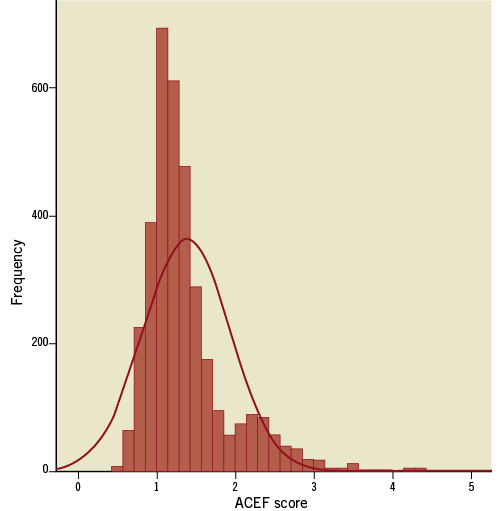
Figure 1. Cumulative distribution of the age, creatinine, and ejection fraction (ACEF) score.
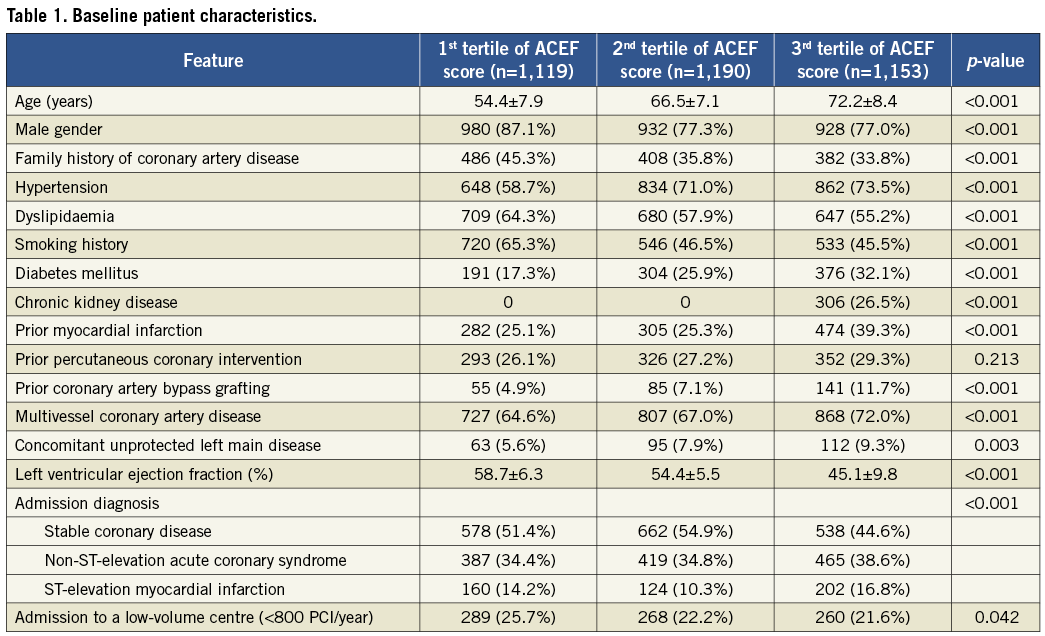
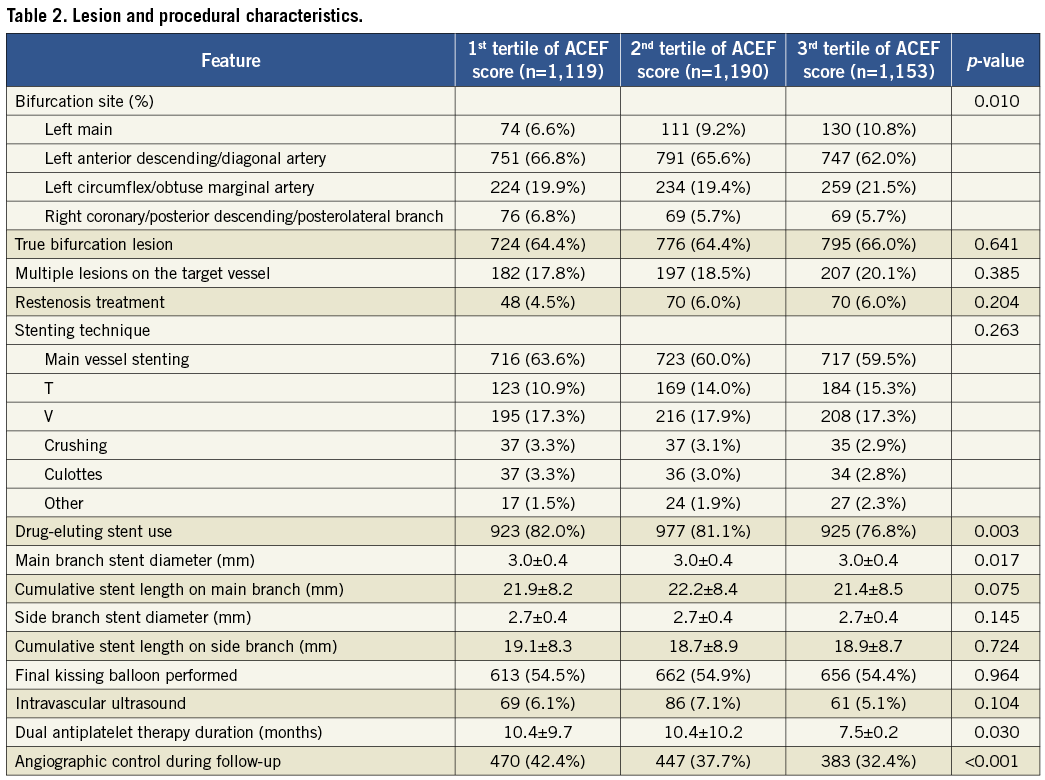
Lesion and procedural features are reported in Table 2. ACEF score tertiles differed significantly for several variables, including bifurcation site, drug-eluting stent use, MB stent diameter, dual antiplatelet therapy duration, and angiographic control during follow-up (all p<0.05).
Short-term clinical outcomes were different among ACEF score tertiles, with significantly higher 30-day rates in the highest tertile for death (0.1% in the lowest tertile, 0.5% in the mid tertile, and 3.0% in the highest tertile, p<0.001), MI (0.3%, 0.7%, and 1.8%, p<0.001), and MACE (0.5%, 1.2%, and 4.3%, p<0.001), with trends towards significance also for TLR (0.2%, 0.7% and 0.9%, p=0.065) and definite stent thrombosis (0.3%, 0.5%, and 1.0%, p=0.063). Accordingly, long-term (24.4±15.1 months) follow-up showed significant differences among ACEF score tertiles for death (1.3%, 2.4%, and 11.0%, p<0.001), cardiac death (0.9%, 1.4%, and 7.2%, p<0.001), MI (3.4%, 2.7%, and 5.7%, p<0.001), MACE (13.6%, 15.9%, and 22.3%, p<0.001), probable stent thrombosis (0.1%, 0.4%, and 0.8%, p=0.023), and possible stent thrombosis (0.4%, 0.4%, and 2.2%, p<0.001), and trends towards significance also for TLR (11.3%, 13.6%, and 14.0%, p=0.061) (Table 3).
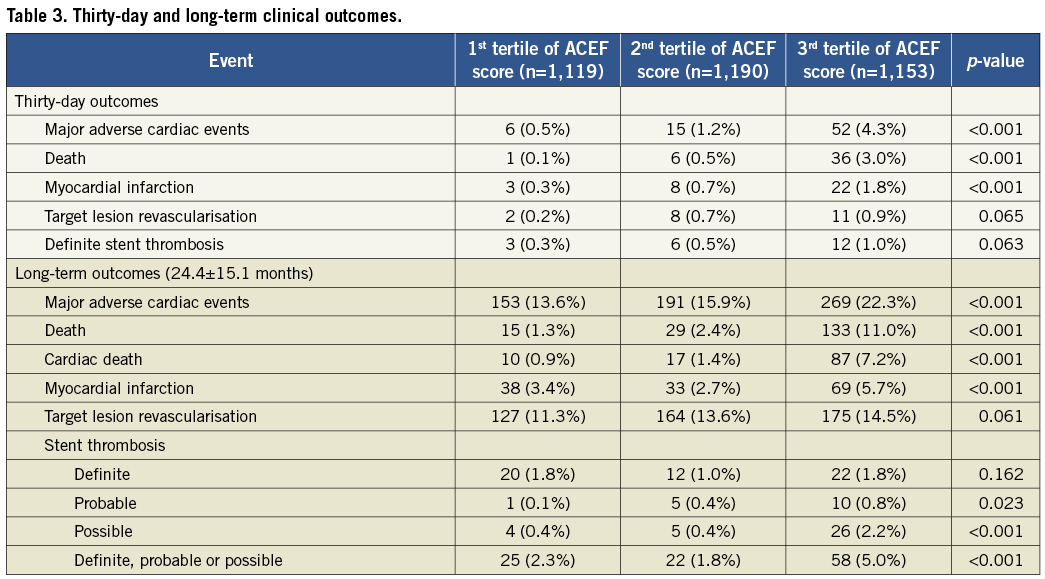
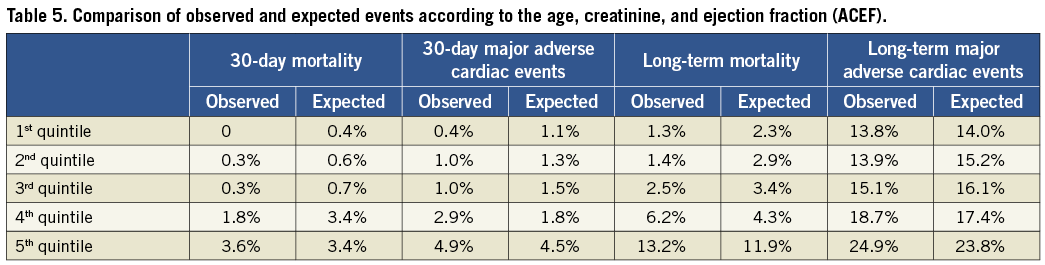
Formal appraisal of the predictive accuracy of the ACEF score showed satisfactory discrimination and calibration for 30-day mortality (c statistic=0.82 [0.77-0.87], p<0.001; Figure 2), 30-day rate of MACE (c statistic=0.73 [0.67-0.78], p<0.001; Figure 3), and long-term mortality (Harrell c-index=0.77 [0.74-0.81], p<0.001, Figure 4), whereas discrimination for long-term rate of MACE appeared only moderate (Harrell c-index=0.60 [0.57-0.62], p<0.001, Figure 5). Similar findings were obtained when distinguishing patients according to admission diagnosis (Table 4), despite some variability between predictive accuracy in stable coronary disease, non-ST-elevation acute coronary syndrome, and ST-elevation myocardial infarction.
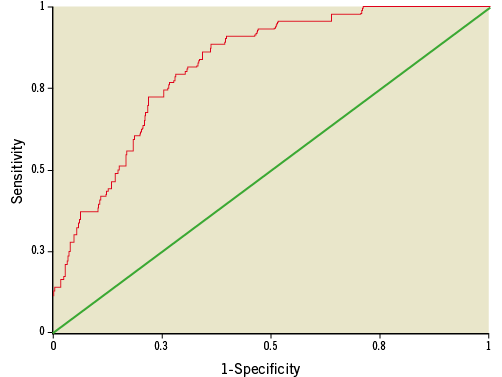
Figure 2. Receiver-operating characteristic curves of the age, creatinine, and ejection fraction (ACEF) score for 30-day mortality (area under the curve=0.82 [95% confidence interval 0.77-0.87], p<0.001).
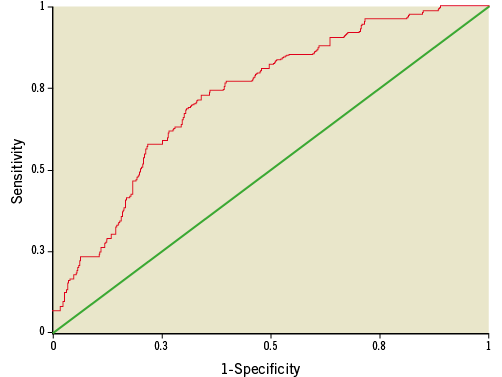
Figure 3. Receiver-operating characteristic curves of the age, creatinine, and ejection fraction (ACEF) score for 30-day major adverse cardiac events (area under the curve=0.73 [95% confidence interval 0.67-0.78], p<0.001).
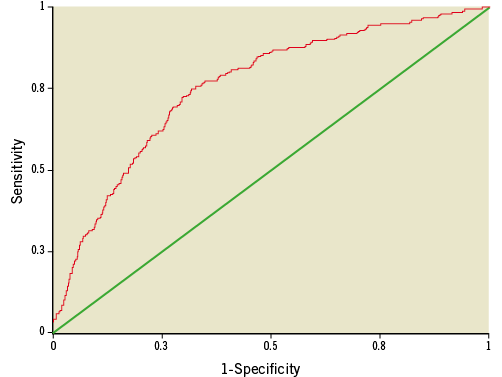
Figure 4. Receiver-operating characteristic curves of the age, creatinine, and ejection fraction (ACEF) score for long-term mortality (area under the curve=0.77 [95% confidence interval 0.74-0.81], p<0.001).
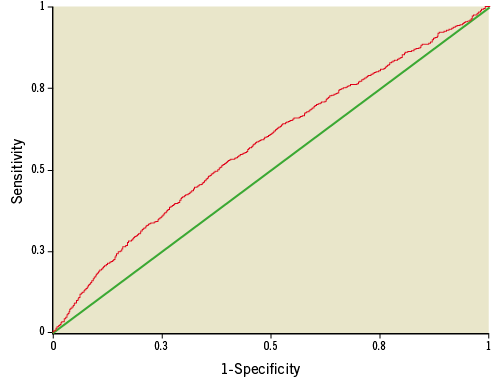
Figure 5. Receiver-operating characteristic curves of the age, creatinine, and ejection fraction (ACEF) score for long-term major adverse cardiac events (area under the curve=0.60 [95% confidence interval 0.57-0.62], p<0.001).
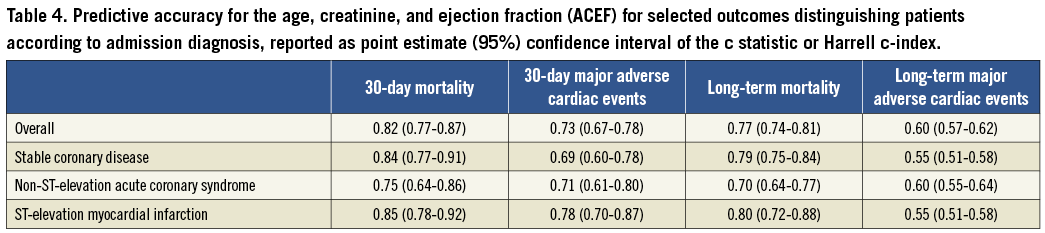
Exploiting the ACEF score as a three-level variable (i.e., according to tertiles) rather than as a continuous variable only mildly decreased its discrimination for 30-day mortality (c statistic=0.77 [0.72-0.82], p<0.001), 30-day rate of MACE (c statistic=0.71 [0.65-0.76], p<0.001), and long-term mortality (Harrell c-index=0.73 [0.69-0.76], p<0.001, Figure 4), whereas discrimination for long-term rate of MACE appeared only moderate (Harrell c-index=0.58 [0.56-0.60], p<0.001). Calibration was appraised by comparing expected versus observed event rates, showing satisfactory calibration, especially for mid and high ACEF scores and short-term events (Table 5).
We have previously reported that the most important independent predictors of events in the I-BIGIS study were age, creatinine, complex stenting strategy, DES usage, diabetes mellitus, ejection fraction, multivessel disease, PCI for in-stent restenosis, prior PCI, and prior CABG.11 We thus aimed to confirm our prior findings by appraising the independent prognostic role of the ACEF score adjusting for all the above factors (excluding age, creatinine, and ejection fraction). Indeed, in such multivariable models, the ACEF score was confirmed as an independent and significant predictor of 30-day mortality (OR=3.78 [2.68-5.32], p<0.001), 30-day MACE (OR=2.45 [1.84-3.25], p<0.001), long-term mortality (HR=2.66 [2.30-3.09], p<0.001), and long-term MACE (HR=1.48 [1.30-1.67], p<0.001).
Discussion
This work, originally reporting on the predictive accuracy of a simple and user-friendly prognostic score in subjects undergoing bifurcation PCI, has the following implications: a) PCI for coronary bifurcation lesions is generally safe and effective, but fatal and non-fatal adverse events do occur in a subset of patients; b) risk prognostication with the ACEF score is effective and accurate for both short-term and long-term outcomes; c) given such independent predictive accuracy, use of the ACEF score is thus recommended to inform clinicians and patients when bifurcation PCI is envisaged.
Coronary bifurcation lesions have been the subject of extensive research given their uniqueness and association with procedural failure, early complications, and late adverse events.13 Much evidence has thus accumulated on the lesion classification, techniques and devices.4,13,14 Several issues regarding bifurcation PCI have already been largely sorted out. First, the Medina classification has clearly come out as the most practical and informative one.13 Second, provisional T stenting clearly appears as the most cost-beneficial technique whenever feasible.15 Third, dedicated devices have not so far proved to be superior to second-generation DES. 4,14,16
Despite such collective scientific effort focusing on bifurcation PCI, no dedicated prognostic tools dedicated to patients with this peculiar type of coronary disease are available. Indeed, several clinical risk scores have already been developed and tested for unselected PCI patients (Table 6), such as the Mayo Clinic,17 the Michigan Cardiovascular Consortium,18 the National Cardiovascular Database Registry,19 the New York State Registry,20 the Society for Cardiovascular Angiography and Intervention,21 the STENT5, and the Toronto scores.22 Other tools are also available, with different scope and focus, which may include subtle patient features (e.g., presence of concomitant infections) or coronary anatomy (e.g., SYNTAX score).23
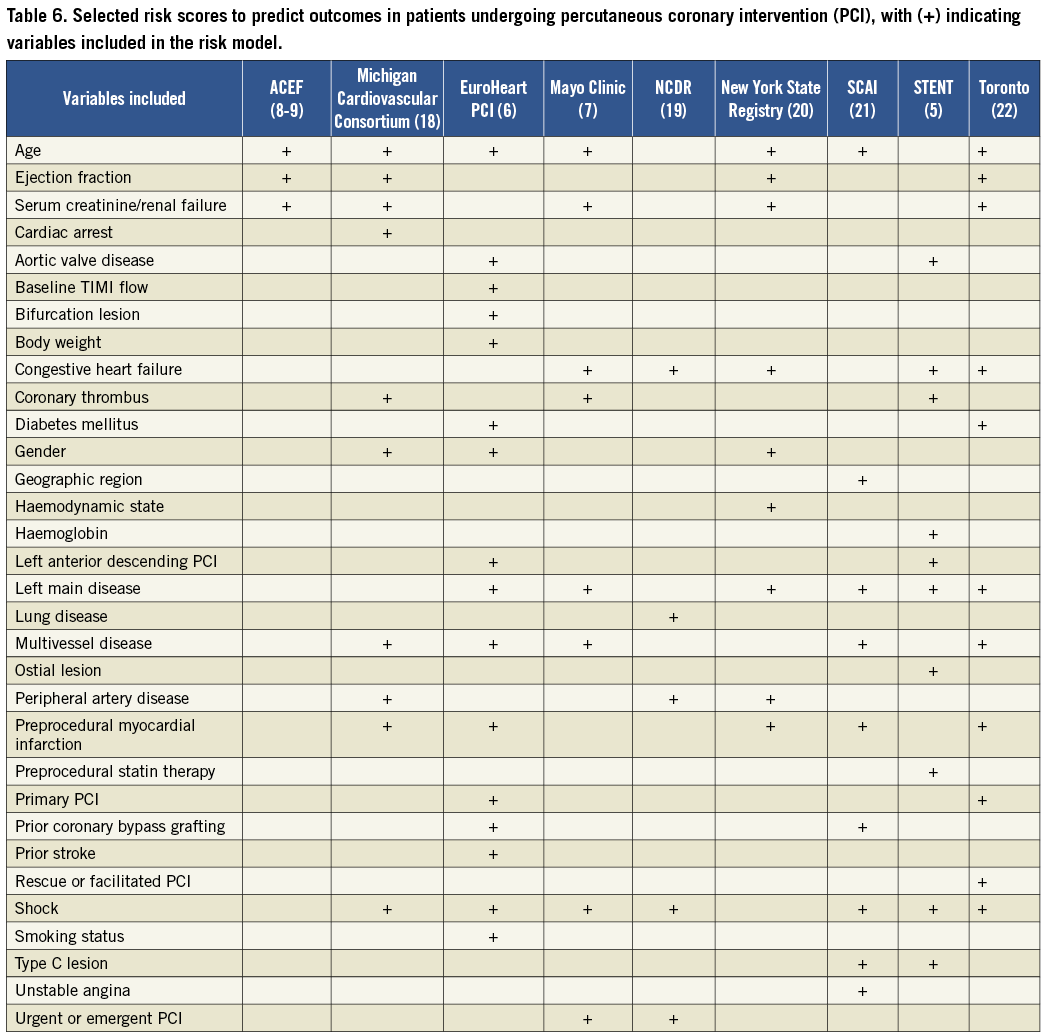
A quick glance at Table 6, which summarises the variables exploited by a selection of the available scores, clearly provides support to our current findings on the role of the ACEF score for risk prognostication in bifurcation PCI. Excluding age, ejection fraction and renal function, most variables are used only in a subset of the scores. Moreover, all scores require computing several variables, making them cumbersome and difficult to use in everyday practice. Besides user-friendliness, our findings show that the ACEF score has a satisfactory predictive accuracy for mortality at both short and long term and for non-fatal events at short term. The prognostic value of the ACEF score is only moderate for long-term non-fatal outcomes, but the reader should take into account the fact that long-term MACE are largely dominated by repeat revascularisations, which have an altogether different pathophysiology and clinical implications in comparison to death.
The favourable results on the predictive role of the ACEF score in bifurcation PCI hereby reported confirm recent data from the 1,208-patient sub-analysis of the LEADERS trial. Specifically, Wykrzykowska et al applied the ACEF score in an all-comers population and showed at 1-year follow-up higher rates for cardiac death, MI, TVR, MACE, and stent thrombosis in patients with higher ACEF scores (all p<0.05).10 The most relevant difference between the data reported by Wykrzykowska and colleagues and ours concerns different thresholds for tertiles. Whereas we divided our study population into three groups according to ACEF score <1.090, between 1.090 and 1.380, and >1.380, Wykrzykowska et al used the following cut-offs: ≤1.0225, between 1.0226 and 1.277, and >1.277. Several reasons can explain these differences, including different patient selection features, timing of cardiac function assessment, and assays for serum creatinine. Specifically, the LEADERS trial was indeed an all-comers study, but still a trial comparing two DES10. Accordingly, several patients with contraindications to DES implantation or prolonged dual antiplatelet therapy were not included in LEADERS. Conversely, our study is truly an all-comers retrospective registry including any patient with bifurcation PCI treated at participating centres.
Predictive accuracy of the ACEF score was indeed satisfactory, but not perfect. However, we should bear in mind that no risk prediction tool in biomedical science can be expected to have perfect accuracy (unless the corresponding data are fabricated). Moreover, if several additional variables (5, 10, or even 15) must be added to improve only slightly the predictive accuracy of a given score, the value of parsimony and the Pareto principle (according to which 80% of your overall prognostic yield comes from only 20% of your predictive variables) clearly and eventually favour the ACEF score, which includes only the three most important prognostic factors: age, systolic function, and renal function.8,9,24 On the other hand, in keeping with its original developmental context, the ACEF score is most likely better fitted to low-risk elective patients undergoing revascularisation procedures, where the cardiac event rate is low, the number of events recorded per year is limited, and the more complex risk model may be overfitted, rather than to acute settings.24 Despite this, practitioners who already rely on the more detailed and accurate risk scores (e.g., the Mayo Clinic score) should probably not abandon it to move to the ACEF score, which is not likely to outperform them. Conversely, cardiologists who have so far been wary of using any score can safely and comfortably adopt the ACEF score given its clinical usefulness and simplicity.
This work has limitations, however, as does any observational retrospective study. In addition, we did not perform multivariable adjusted analyses to prove the independent prognostic value of the ACEF score,25 as our goal was not to make the case for using the ACEF as an adjustment factor, but rather to support its broader use in everyday clinical practice. Another drawback of our study is the exclusion of the 18.1% of subjects originally enrolled in the I-BIGIS registry who had no complete data enabling computation of the ACEF score. Whereas the baseline and procedural features of these patients were similar to those of patients with complete data, point estimates and confidence intervals for the predictive accuracy of the ACEF score may have been expected to vary, albeit slightly, if these patients had also been included. In addition, information regarding complete revascularisation would of course have been of interest and prognostically relevant; however, collecting this piece of information or other details on multivessel PCI was beyond the scope of our work. The use of the ACEF score to guide management of patients undergoing bifurcation PCI cannot be supported or disproved by the present work. While we may speculate that predicting a patient risk of adverse events may change procedural strategy, further studies are required to appraise this specific scientific question. However, we may tentatively suggest that patients with high ACEF scores should be offered more aggressive medical therapies and risk factor modifications. Finally, comparing the prognostic role of the ACEF score with those of other scores was beyond the scope of our work. However, the parsimony principles stated above would tend to favour the ACEF score even if a more complex score appeared statistically more accurate.
In conclusion, the simple and extremely user-friendly ACEF score can accurately identify patients undergoing PCI for coronary bifurcation lesions at high risk of early fatal or non-fatal complications, as well as long-term fatality.
Conflict of interest statement
G. Biondi-Zoccai has consulted/lectured for Abbott Vascular, Boston Scientific, Cordis, and Medtronic. The other authors have no conflict of interest to declare.

