The treatment of female patients with coronary artery disease has traditionally been associated with an increased periprocedural complication rate and worse outcomes compared to male patients. In the early days of plain old balloon angioplasty there was a lower angiographic success rate and a higher complication and mortality rate in women than in men1. The introduction of bare metal stents (BMS) created hopes that this therapy would improve prognosis in this vulnerable population; however, clinical studies and meta-analyses consistently showed worse short-term outcomes in female patients and a higher incidence of death or myocardial infraction at 30-day follow-up2. The first-generation drug-eluting stents (DES) minimised neointimal proliferation and the incidence of restenosis and improved procedural outcomes in both genders. Studies comparing event rates in male and female patients implanted with paclitaxel- or sirolimus-eluting stents consistently showed improved short- and long-term prognosis compared to patients treated with BMS in both genders, highlighting the efficacy of these devices in the treatment of women3,4. However, despite the improved prognosis noted with the introduction of DES, the target lesion revascularisation (TLR) rate was significantly higher in women in the TAXUS IV study at one-year follow-up (7.6% vs 3.2%, p=0.030); these differences disappeared in studies with the second-generation DES where the incidence of TLR was similar in male and female patients (Figure 1),5.
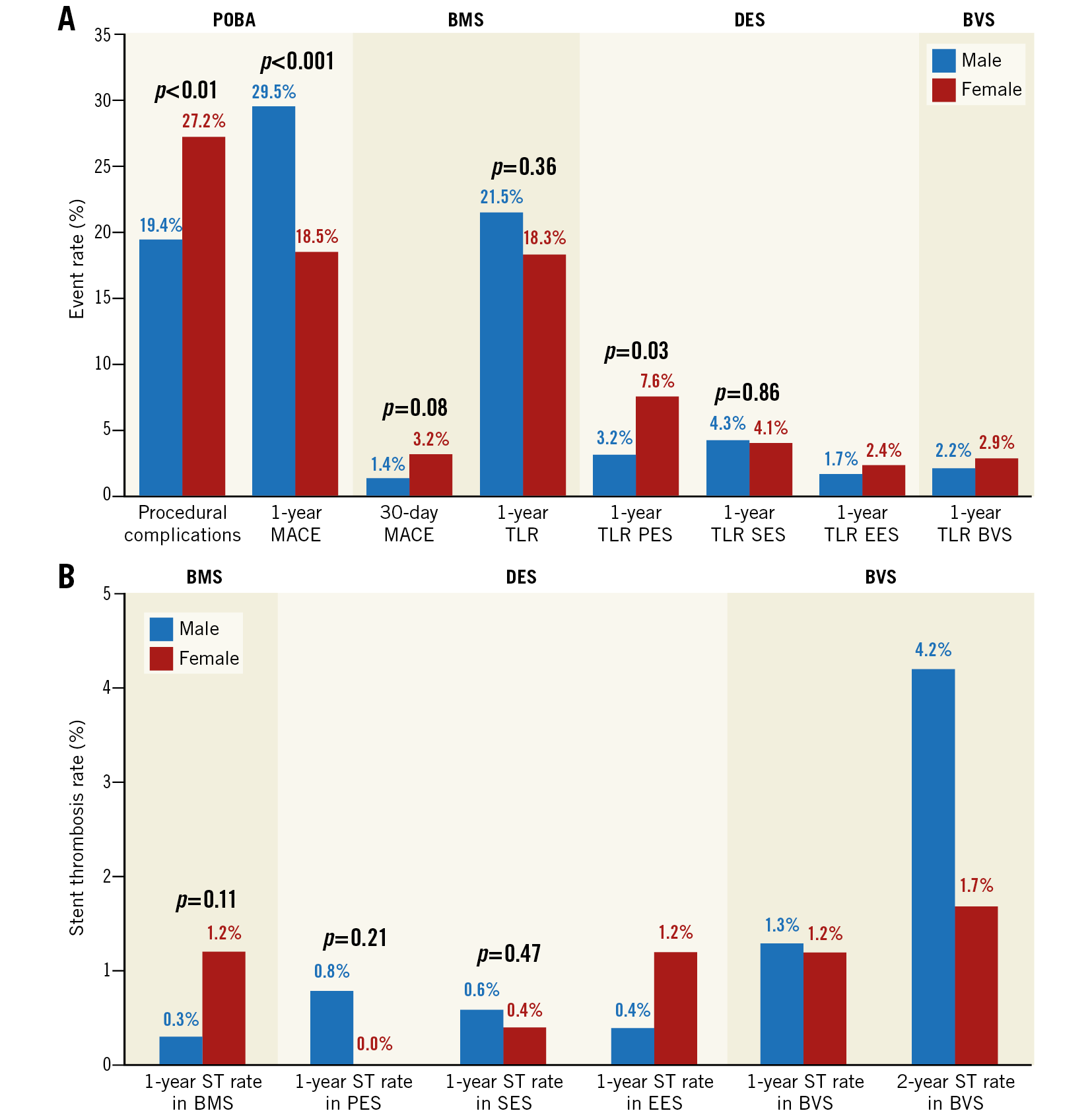
Figure 1. Clinical outcomes after percutaneous coronary intervention with different devices. A) Procedural complications, major adverse cardiovascular events (MACE), TLR and (B) stent/scaffold thrombosis (ST) rates following plain old balloon angioplasty (POBA), bare metal stent (BMS), paclitaxel-eluting stent (PES), sirolimus-eluting stent (SES), everolimus-eluting stent (EES) and Absorb BVS implantation in patients recruited in the study of Baquet et al9 in the NHLBI PTCA registry1, the TAXUS IV4 and AIDA15 randomised controlled studies and in the meta-analyses of Solinas et al3 and Shreenivas et al8.
Bioresorbable scaffolds were introduced in interventional cardiology to overcome the limitations of the metallic stents and improve long-term prognosis in patients undergoing percutaneous coronary intervention (PCI). The mechanical properties, design, strut thickness and configuration as well as the bioresorption process occurring following their implantation impacted on vessel morphology, physiology and biology – in a different manner from the metallic stents – and influenced the outcomes in male and female patients undergoing treatment with these devices6,7.
The first study that compared prognosis in male and female patients implanted with a bioresorbable scaffold (Absorb™ bioresorbable vascular scaffold [BVS]; Abbott Vascular, Santa Clara, CA, USA) included 3,389 patients recruited in the ABSORB II, ABSORB III, ABSORB China and ABSORB Japan studies and showed similar outcomes in the two groups8. However, in the study of Baquet et al9, published in the current issue of EuroIntervention, the authors for the first time demonstrated a gender effect on clinical outcomes at two-year follow-up, with females having a better prognosis than male patients.
The authors analysed data from 1,032 patients (259 women) treated with an Absorb BVS and reported a lower, but not statistically significantly different, incidence of target lesion failure (13.2% vs 17.9%, p=0.12), TLR (12.4% vs 7.5%, p=0.051) and stent thrombosis (1.2% vs 2.7%, p=0.20) in women, while in multivariate analysis female gender was an independent predictor of a lower incidence of TLR. The reported findings should be interpreted with caution; the small number of events reported, the differences in the baseline demographics between the two groups and the marginal differences in the event rates between male and female patients do not allow us to draw firm conclusions.
A possible explanation for the differences in the reported results of Baquet et al9 and Shreenivas et al8 is the differences in the baseline demographics and angiographic characteristics of the patients included in the two studies. Patients in the study of Baquet et al9 had more comorbidities and longer lesions than those included in the meta-analysis of Shreenivas et al8 in which the patients had a smaller reference vessel diameter. These differences should be attributed to the fact that high-risk patients are often underrepresented in randomised controlled studies but also to the bias reported by Baquet et al9 in the selection of patients who were implanted with an Absorb BVS, as in this study the interventional cardiologists preferred the use of scaffolds in large non-calcified vessels. Therefore, in contrast to previous reports, the reference vessel and minimum lumen diameter in this analysis were not different between male and female patients4, while the incidence of moderate/severe calcification which can affect procedural success and long-term outcomes has not been reported in the published results.
Intravascular imaging studies have demonstrated an increased calcific burden in female patients suffering from stable angina10 and, as a consequence, the incidence of severely calcified lesions is higher in female than in male patients recruited in clinical studies8. On the other hand, in acute coronary syndromes – a population that was underrepresented in the first stent studies – the calcific burden in culprit lesions is higher in males11. Plaque composition, especially an increased calcific burden, is a well-known predictor of TLR in metallic stents12 and is expected also to have prognostic implications in Absorb BVS, as the acute gain is smaller following implantation of this device13 that also has thicker struts which, in case of a fibrotic or calcific plaque, tend to protrude into the lumen, causing flow disturbances and a higher shear rate that predisposes to platelet activation and thrombus formation14. The differences in plaque composition between male and female patients may explain the numerically lower scaffold thrombosis rate noted in female patients in this study but also in the AIDA study in which 53.6% of the recruited patients were admitted with an acute coronary syndrome (Figure 1),15.
The above hypothesis, which is supported by the study of Baquet et al9, and suggests that there may be a possible prognostic benefit of the use of Absorb BVS in specific populations and clinical scenarios, requires confirmation by large-scale patient-level meta-analyses of registries and randomised controlled trials. Whether this benefit is also sustained in the long term also needs to be confirmed from the long-term follow-up data of the ABSORB studies.
Conflict of interest statement
The authors have no conflicts of interest to declare.