“We tend to overestimate the effect of a technology in the short run and underestimate the effect in the long run.”
Roy Amara’s law
Bioresorbable coronary scaffolds (BRS) have been developed to achieve stenosis dilatation and stenting while uncaging the coronary vessels from permanent metallic structures. Uncaging the vessels in order to allow restoration of physiology has become a significant unmet need, especially when dealing with complex multivessel or diffuse disease that requires long vessel segments to be stented. The timing, however, for introducing the disruptive bioresorbable technology could not have been worse. First-generation BRS were thrown into the arena to compete against second-generation drug-eluting stents (DES), the latter having largely overcome most of the limitations and inefficiencies affecting bare metal stents and first-generation DES during the past two decades. Current-generation best-in-class DES are remarkably effective, demonstrating high deliverability through severely diseased vessels, strong scaffolding properties, resistance to early, late and very late stent thrombosis, even with a shorter duration of dual antiplatelet treatment, and low recurrence rates even in the long term. Low rates of in-stent neoatherosclerosis and related late clinical events remain, perhaps due to the permanent presence of remnants of the initial drug-polymer platform, certainly associated with the failure of secondary prevention measures to eliminate disease progression.
Given this environment and following CE mark approval of the Absorb™ BVS (Abbott Vascular, Santa Clara, CA, USA) in 2011 and FDA approval in 2016, it took only a few years for the initial enthusiasm that followed the results of ABSORB trial cohorts A and B1,2 to fade away, culminating in the current removal from the market of the most studied and diffused BRS (Absorb BVS). The latter was driven by safety concerns raised by higher relative rates of scaffold thrombosis (ST) observed in registries and clinical trials, in comparison with current metallic DES3-5 (Ellis SG. Everolimus-eluting bioresorbable vascular scaffolds in patients with coronary artery disease. Presented at: American College of Cardiology [ACC] Annual Scientific Session, Washington, DC; March 18, 2017). In this context, this issue of EuroIntervention hosts a registry, a meta-analysis, the four-year follow-up results of a clinical trial, and a position paper that, taken together, reflect the current status of the field and the ongoing uncertainty regarding the future of polymeric BRS in interventional cardiology.
ABSORB UK Registry
The investigators of the ABSORB UK Registry present the one-year follow-up data on 1,005 patients treated using the Absorb BVS6.
Included patients represented on average 2.7% of all percutaneous coronary interventions (PCI) performed at the participating sites (range 0.2-7.3%). Considering that half of the treated stenoses were rather complex (47.4% B2/C lesions), the target lesion failure (TLF: cardiac death, target vessel [TV]-related myocardial infarction [MI], ischaemia-driven target lesion revascularisation [TLR]) rate reported at 3.2% is relatively low, as compared to previous reports3,5. This finding is associated with a careful implantation technique (predilatation in 97.5%, high-pressure post-dilatation at 17 atm in 94.9%) and a rather high use of intravascular imaging to guide PCI, by mostly very experienced operators. Procedural technique was pre-specified but designed prior to implementation of strict rules for “PSP”, namely predilatation, sizing and post-dilatation7. A simple “PSP” technique was applied in 65.8% of BVS cases, but was not shown to impact on any efficacy or safety outcome metric, unlike more recent reports8,9.
Dual antiplatelet therapy (DAPT) regime was extended to one year for the vast majority of patients (99.1%), despite the fact that patients with acute coronary syndrome (ACS) were less than half of the study population. Nevertheless, ST rates remained high (definite ST at 1.4%, definite and probable ST at 1.7%), similar to the rates reported in the ABSORB III randomised trial10. Interestingly, the only independent predictor of ST at one year by multivariable logistic regression remains small scaffold size (2.5 mm in diameter). These results confirm the findings by Ellis et al showing that reference vessel diameter <2.40 mm was associated with ST11.
Meta-analysis on midterm outcomes of seven randomised trials
The comparison to second-generation DES remains a source of disappointment and the main reason for the extended “trough of disillusionment” (Figure 1) that the BRS technology is currently facing. The meta-analysis by Cassese et al published in this issue of EuroIntervention is powered at 81% to detect a 25% relative difference in TLF and at 73% to detect a relative risk reduction of 50% in definite and probable ST. The analysis reaffirms a higher risk of TLF (odds ratio [OR] 1.35, p=0.0028, number needed to harm 38), target vessel MI (OR 1.68, p=0.008), and ischaemia-driven TLR (OR 1.42, p=0.007) for BVS vs. everolimus-eluting stents (EES)12.
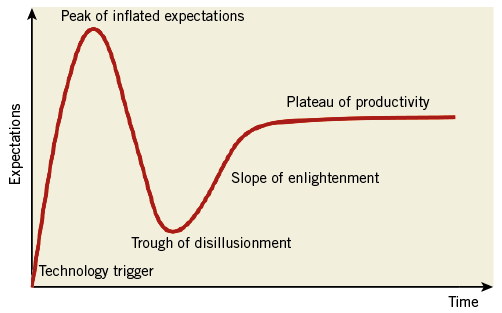
Figure 1. Gartner Hype Cycle diagram.
Particularly worrisome is the finding that definite and probable ST rates are fourfold higher for BVS beyond the first year following implantation, when one would expect to see the first beneficial effects of scaffold resorption. At the longest available follow-up, the number needed to harm was 63 (OR 3.24, p=0001). The majority of patients treated with BVS having a (very) late ST presented with ST-elevation MI at the time of re-admission, suggesting that the higher MI rate hereby reported is related – at least to a certain extent – to ST, rather than to minor periprocedural MIs.
Importantly, this meta-analysis based on aggregate data included three trials with follow-up at three years and provides risk estimates at three time points (at 12 and 24 months and at the longest follow-up) plus two landmark analyses (beyond 12 and 24 months). In the period beyond 24 months, TLF and ST rates remain higher for patients treated with BVS vs. EES; however, the difference is no longer statistically significant. Imaging studies4 have identified scaffold discontinuity, prolapsing dismantled struts and malapposition that occur at the moment of advanced stages of BVS resorption as the causes for these late unanticipated events.
ABSORB II at four years
The ABSORB II trial investigators report that, at four years of follow-up, TLF rates are no longer significantly different between BVS and EES (11.5% vs. 6.0%, respectively, p=0.063). In addition, no ST was observed between three and four years. They optimistically conclude that “a downturn of events was recorded beyond the expected resorption time”13.
This report, along with the 24-month landmark analysis by Cassese et al12, suggests that there is a light at the end of the tunnel. How long is the tunnel? Somewhere between three and four years, after a bioresorption delay that varies in the individual patient, based on plaque characteristics as well as on the mass of polymer to be digested. These hypothesis-generating but encouraging findings require consolidation by continued four-year follow-up data from larger trials. It should be cautiously noted that ABSORB II was not powered for clinical endpoints and that completeness of follow-up at four years was only 86% and 84% in the BVS and EES cohorts, respectively.
ESC-EAPCI Task Force on evaluation of bioresorbable technologies
Further to the publication of the earlier 2015 document that reviewed the proposed evaluation pathways for metallic DES14, an executive summary of the specific recommendations for the evaluation of bioresorbable scaffolds completes this series of articles15.
Even before BVS became unavailable, the Task Force recommended that BRS should not be preferred to conventional DES for clinical practice use15. A comprehensive evaluation of polymeric devices other than Absorb BVS and metallic bioresorbable scaffolds is provided along with a proposed non-clinical and clinical evaluation testing programme of new bioresorbable scaffolds. The Task Force proposes that CE-mark approval include a plan for post-market large-scale randomised clinical trials powered for clinical endpoints. Leads for improved outcomes have been identified through proper patient/lesion selection and standardised procedural technique. However, device iterations other than BVS with smaller scaffold footprint (reduced strut thickness and width), stronger mechanical properties, different material characteristics and bioresorption time, and alternative duration of drug release, are being evaluated and are undergoing extensive preclinical research and clinical evaluation.
Considering that larger companies have adopted a “watchful waiting” approach, it remains uncertain whether smaller entrepreneurs will be able to climb the “slope of enlightenment” and reach “the plateau of productivity” (Figure 1). Some of the late data presented in this series of articles should be seen as encouraging for continued investment and development. As stated by the Task Force, “… all other things being equal, a scaffold that disappears after its successful function in preventing recoil and constrictive remodelling is served is likely to be preferable to a conventional stent.”15.
Conflict of interest statement
W. Wijns reports receiving research grants to his previous institution from Abbott, MiCell, MicroPort and Terumo, and speaker fees from Abbott, Biotronik and MicroPort. S. Pyxaras has no conflicts of interest to declare.