Abstract
Bioresorbable scaffolds (BRS) were designed more than 30 years ago to overcome the disadvantages related to the permanent implantation of a metallic stent and, at present, a number of these devices have obtained a CE mark on the basis of midterm follow-up studies. However, although BRS have already been introduced into clinical practice, intensive research is ongoing worldwide to clarify their long-term safety and effectiveness. This type of research has captivated the interest of the cardiovascular community after the recent publication of long-term follow-up data from randomised trials demonstrating increased late scaffold thrombosis in the Absorb™ BRS (Abbott Vascular, Santa Clara, CA, USA). In this regard, any long-term follow-up data for BRS are of particular importance, especially when they originate from real-world patients, challenging lesions and scaffolds other than the Absorb GT1™, which is the only available BRS that has been evaluated in a controlled fashion so far versus the current standard, new-generation drug-eluting stents. The session “Long-term data of BRS” on the last day of EuroPCR 2017 (Paris, France) offered some very interesting data on what the global picture for the future of BRS could be.
Introduction
On the last day of EuroPCR 2017 in Paris, I had the privilege to chair with Antoine Lafont and Roberto Diletti a session on the long-term data of bioresorbable scaffolds (BRS). It was a fascinating session, with data that sometimes contradict themselves, but finally give a global picture of what the long-term data on BRS could be.
Presentations
First, we had a presentation by Ricardo Costa on the post-marketing evaluation of the Elixir DESolve® novolimus-eluting coronary BRS (Elixir Corporation, Milpitas, CA, USA) – DESolve Bioresorbable Scaffold: PMCF 2-year Clinical Results1. The bioresorption of this scaffold offers potentially important key differences as compared to other BRS. Specifically, this scaffold is characterised by an early degradation at six months, complete resorption in one year and a high fracture resistance with the ability to overexpand across an extended range of diameters. In this post-marketing registry of 102 patients – in which 51% had type C lesions – the scaffold thrombosis (ST) rate was 1% and the major adverse cardiac events (MACE) rate was 4%, while in the DESolve Nx study2 which included 126 patients –only 3% of whom had type C lesions– the rates of definite scaffold thrombosis and MACE were 0% and 7.4%, respectively. These results are good, showing safety and effectiveness at two years. However, it must be remembered that the ABSORB B1/B2 first-in-man study showed no scaffold thrombosis and a MACE rate of 9% at two years3. It is also worth mentioning that there is a newer iteration of this device, characterised by a reduced strut thickness (120 microns) with an abluminal round contour for improved embedment and an accompanying balloon with preferentially enhanced force transmission at the centre of the scaffold.
The second speaker was Javier Molina, from the Clinique Pasteur in Toulouse, France –BVS for the treatment of long coronary lesions: the Long-ABSORB registry4. This registry evaluated the use of the Absorb BRS to treat long lesions. Long lesions were defined by a length >20 mm or the need to use a stent longer than 28 mm. The mean stent length was 41.9 mm, ranging from 28 to 96 mm, with a mean number of stents per lesion of 1.7. The use of two or more stents was observed in 58% of the cases and OCT was used in 43% of the cases. From a technical point of view, predilatation was performed with a balloon-to-vessel ratio of 1:1 and the use of high-pressure post-dilatation was mandatory. If stent overlapping was used, the minimal overlapping technique was applied under stent boost fluoroscopy, which is a good additional trick for implantation in the case of long lesions. In this registry of 113 patients whom we assume were “consecutive” (although they were collected over a period of two years), there was one sudden death observed within one month, attributed to ST, and an additional ST (probable) at two years, with a cumulative rate of 1.77%. The cumulative rate of target lesion failure (TLF) was 9.7%. Either coronary CT or angiography was used for follow-up, which was obtained in 90% of the cases, showing in-stent restenosis in 5.3% of the cases at two years (Table 1). The investigators concluded that the use of BRS to treat long lesions is feasible and at two-year follow-up the rate of TLF was low. This registry showed good results, but it is always difficult to make the right interpretation in the absence of a comparator, a comment which also applies to the DESolve study.
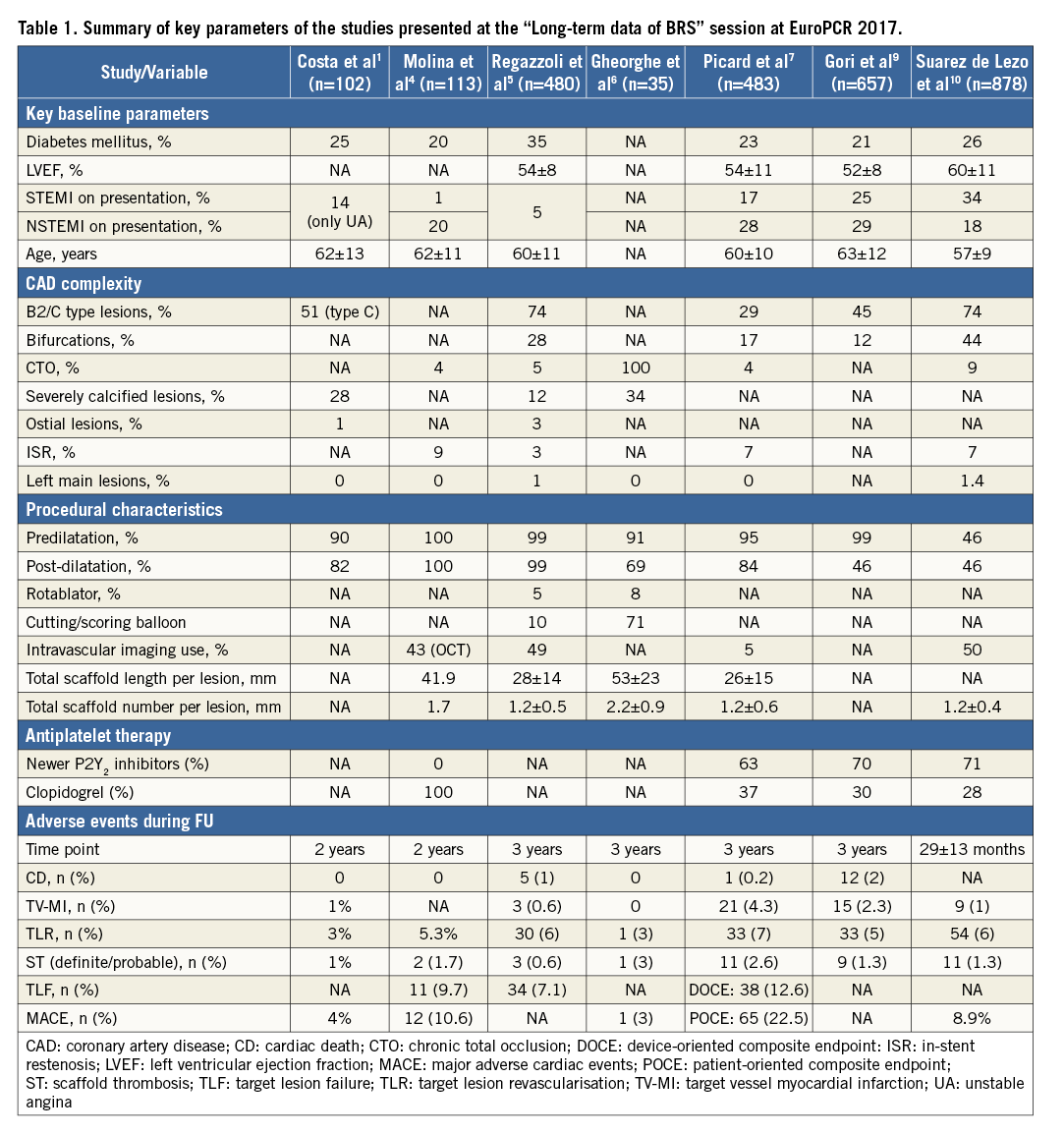
The third presentation was given by Damiano Regazzoli on behalf of three high-volume centres, San Raffaele University Hospital (Milan, Italy), Centro Cuore Columbus (Milan, Italy) and Fortis Healthcare (New Delhi, India) – Long-term follow-up of BRS implantation for complex coronary lesions: a multicentre experience5. In that study, a total of 480 patients with 762 lesions were enrolled between May 2012 and December 2014. What characterised these three high-volume centres was that a dedicated technique of BRS implantation was applied from the beginning. This dedicated technique encompassed aggressive predilatation for preparation of the lesion, in order to avoid balloon indentation and to allow complete BRS extension. There was liberal use of intravascular imaging in large and small vessels for scaffold sizing, and post-dilatation was mandatory with high pressures and non-compliant balloons. The baseline demographics clearly indicate that they were dealing with a complex population, including 35.6% diabetic patients, and complex lesions, including significant percentages of bifurcations, chronic total occlusions, restenosis, ostial and severely calcified lesions. Scoring, cutting balloon or rotablator was used in more than 15% of the cases, the total scaffold length per patient was 44±28 mm, and the total scaffold number per patient was 1.9±1. Post-dilatation was performed in nearly all patients (99.1%) and the post-dilatation pressure was 22±3.6 atm. As mentioned earlier, intravascular imaging was used in almost half of the patients. What is absolutely remarkable in this retrospective study is that the TLF rate was 7.1% at three years, with 1% cardiac death and only 0.6% definite/probable ST, which means three patients out of this cohort of 480 patients and 762 lesions (Table 1). Interestingly, they mentioned in their presentation a rate of 13.1% for any revascularisation, even including staged procedures. These results are absolutely remarkable and could sustain comparison with a comparator such as the XIENCE stent (Abbott Vascular). Of course, the comparator was not there and, as in every registry, the data might be less reliable than in a truly randomised trial, with monitoring and adjudication of the events by an independent critical events committee. In their slides, the number of patients being lost to follow-up was not tabulated. Nevertheless, these results strongly suggest the impact of the implantation technique. I wish this experience could be duplicated in a randomised approach with, as mentioned above, a guarantee of correct collection of the data. However, Antonio Colombo and his team have accustomed us to the correctness of their data and, in contrast to some other presentations in this session, the results were outstanding and are an indirect argument for the importance of the technique of implantation.
The fourth presentation was from the combined group of the Hospital de Sant Pau y de la Santa Creu and the Bellvitge University Hospital, both in Barcelona, Spain, with Antonio Serra as senior author - Long-term follow-up of late-acquired incomplete stent apposition in CTO treated with BRS6. That study concerned a small series of 35 patients with chronic total occlusions (CTO) followed for three years. They presented the J-CTO score of these patients: 25% with a score of 0, 48% score 1, and 27% score ≥2. It is interesting that this series used non-compliant balloons, cutting balloons and rotablator in 20%, 71.4% and 8.6%, respectively. A mean number of 2.2 scaffolds was implanted per lesion, the total scaffold length was 52.9 mm, and the post-dilatation with non-compliant balloon was 0.5 mm greater than the vessel size and performed in 69% of the patients. At three-year follow-up, there was one ST (2.8%) and 11.4% in-scaffold re-occlusion (Table 1). In addition, these authors looked at the process of late acquired malapposition that has been repeatedly described in the literature following drug-eluting stent use in CTO. In this regard, it was very interesting to see that, in their series, the transient, late acquired malapposition observed at one year with OCT disappeared at long-term follow-up (three years) (Figure 1).
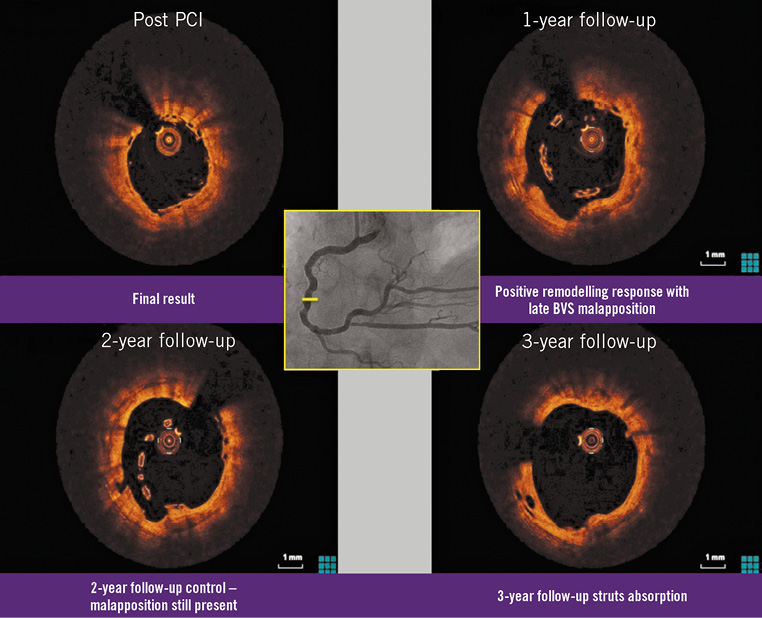
Figure 1. Imaging follow-up with OCT of a BRS implanted in the mid RCA, immediately post implantation and then yearly, demonstrating late malapposition at one year which was resolved at three years with the absorption of the struts. Adapted from: Long-term follow-up of late-acquired incomplete stent apposition in CTO treated with BRS. Gheorghe et al6.
The fifth presentation was by Fabien Picard, from the group of Jean-Francois Tanguay, at the Montreal Heart Institute, Montreal, Canada. They reported a series of 483 patients with 580 lesions, collected between May 2013 and June 2015 – Long-term follow-up of late-acquired incomplete stent apposition in CTO treated with BRS7. As many registries do, it was claimed that they enrolled and treated an all-comer population, but that statement has to be taken “with a grain of salt” as it is somewhat unlikely considering the large number of patients treated at the Montreal Heart Institute during this period. There must have been some selection, as in all these registries, related to the experience and the seniority of the operators. Nevertheless, the population is extremely well documented and the statistical analysis is appropriate. Almost 40% of these patients had multiple vessel disease and there was quite a large proportion of STEMI (17%) and NSTEMI (28%). Sixty-three percent of these patients were using either ticagrelor or prasugrel and only 37% of the patients were using clopidogrel. Looking at the procedural characteristics, it is clear that there was a very limited use of intravascular/intracoronary imaging, in contrast with the Milan experience, but post-dilatation was performed in a high proportion of patients (84%), which is an important point considering the multivariate analysis performed on this group. The nominal size of the scaffold diameter was 3.01±0.39 mm. At three years, the rate of the device-oriented composite endpoint (DOCE) was 12.6% and that of definite or probable ST 2.6% (Table 1). Of the 11 ST, three were early, two late and six very late, which is always a concern and corresponds, more or less, with the numbers seen in the ABSORB II study8, dealing with a much easier population. What was striking in the present series and is puzzling is the increase in DOCE and the patient-oriented composite endpoint (POCE) between 24 months and 36 months. The percentage rose from 7.6% to 22.5% for POCE and from 4.5% to 12.6% for DOCE. The rate of definite or probable ST increased from 1.1% to 2.3% and 2.6% from one to two and three years, respectively. In the univariate analysis, only the presence of in-stent restenosis at baseline had a significant p-value for the prediction of adverse outcome. In the multivariate analysis, no significant predictors were identified. This was the case for post-dilatation and ACS, which failed to reach statistical significance, despite the interesting observation that ACS had a hazard ratio of 0.55 (95% CI: 0.27-1.14) (Figure 2).
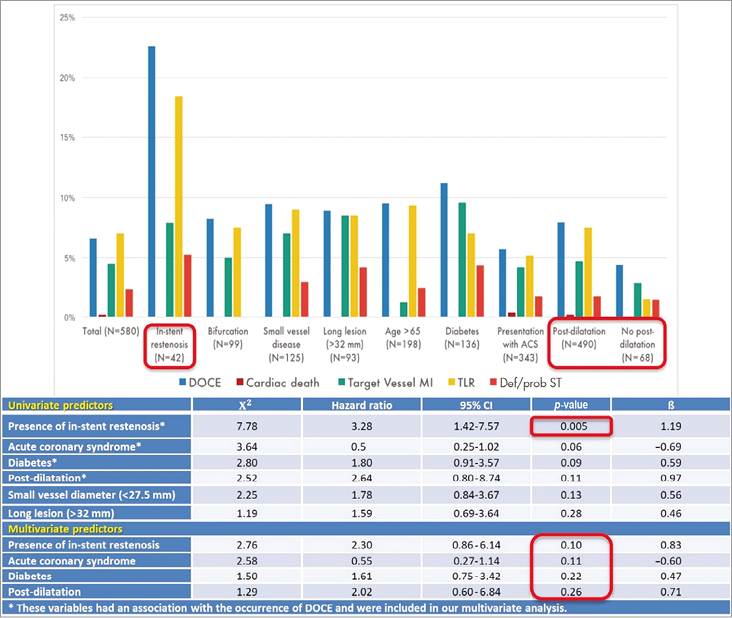
Figure 2. Rates of adverse cardiac events in various subgroups (upper panel) and results of the univariate and multivariate Cox regression analysis of predictors of these events during follow-up (lower panel). Adapted from: Mid to long-term clinical outcomes of everolimus-eluting bioresorbable vascular scaffold to treat all-comer patients. Picard et al7.
So, in conclusion, no lesion or procedural parameter was an independent predictor of DOCE or ST, and post-dilatation which was used in 84% of the cases was not a predictor of good outcomes in this cohort. In the limitations of this study, the researchers mention the retrospective, non-randomised character of the study, the operator-dependent techniques of overlap and post-dilatation, the low use of intravascular imaging and the non-blinded assessment of clinical events and angiograms.
The sixth presentation was from Tommaso Gori, on the long-term safety of BRS in complex lesions, including ostial lesions, bifurcations, long lesions and chronic total occlusions, patients with diabetes mellitus, ACS and thrombotic occlusions - Bioresorbable everolimus-eluting vascular scaffolds for type B2/C coronary lesions: a three-year follow-up study9. Data on the short and midterm safety of BRS in complex lesions have already been published by this group, so in the current presentation they looked at the outcomes up to 1,050 days. In a population of 657 patients, they divided the population into patients with complex lesions (B2 and C, n=297) and those with simple lesions (A and B1, n=360). They presented comparative MACE rates and Kaplan-Meier estimates of survival free from scaffold thrombosis and restenosis for these two groups, before and after one year. Furthermore, using Kaplan-Meier analysis, in a somewhat simplistic fashion, they concluded that the treatment of the B2/C lesions without appropriate implantation technique was associated with an increased incidence of scaffold thrombosis and restenosis at three years, implying that the improper implantation rather than the biologic characteristics of the lesion may determine the outcome of patients (Figure 3). The main discussion was how the distinction between correct and incorrect implantation was made; obviously there was no multivariate analysis or appropriate propensity analysis but just a (retrospective?) distinction between correct and incorrect implantation technique. During the discussion, the panel mentioned that reviewers may be quite critical about this approach and that with an appropriate propensity technique their message could be much clearer than with the univariate analysis.
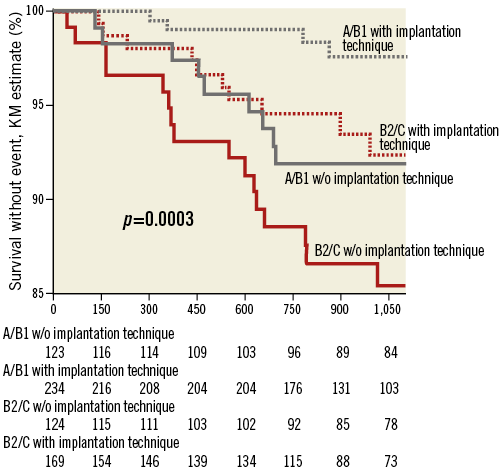
Figure 3. Impact of implantation technique and lesion complexity on the long-term survival free from scaffold thrombosis in patients undergoing percutaneous revascularisation with BRS. Adapted from: Bioresorbable everolimus-eluting vascular scaffolds for type B2/C coronary lesions: a three-year follow-up study. Gori et al9.
The last presentation was given by José Suarez de Lezo, on behalf of the Corpal group, working in Cordoba and Las Palmas de Gran Canaria, Spain - Everolimus eluting BRS. Impact of lesions complexity on clinical outcome and predictors of adverse cardiac events at long term follow-up10. This group collected 878 patients with 1,065 lesions; there was a three-year follow-up in 270 patients with 374 lesions. In the baseline characteristics, it is remarkable to note that 34% of the patients presented with STEMI and the BRS length was not particularly long (24.5±12.4 mm). What was surprising in that presentation was that 54% of the implantations were direct implantations, in other words there was no predilatation. They used intracoronary imaging in about 50% of the cases, half with OCT and half with IVUS, and more than 71% of the patients were treated with new P2Y2 inhibitors, while 28.6% were treated with clopidogrel. They had an average follow-up of 29±13 months and the global MACE rate was 8.9%. During follow-up, four late and seven very late ST (definite/probable) were observed (Table 1). In the predictors of BRS thrombosis, they incriminated in a univariate analysis diabetes mellitus, low ejection fraction, use of clopidogrel and the presence of bifurcation lesions. In terms of survival free from ST, the worst group was the one with direct BRS implantation and post-dilatation, with a rate of 4.4%. It is remarkable that direct stenting without post-dilatation demonstrated a low rate of ST (0.87%) (Figure 4, Figure 5).
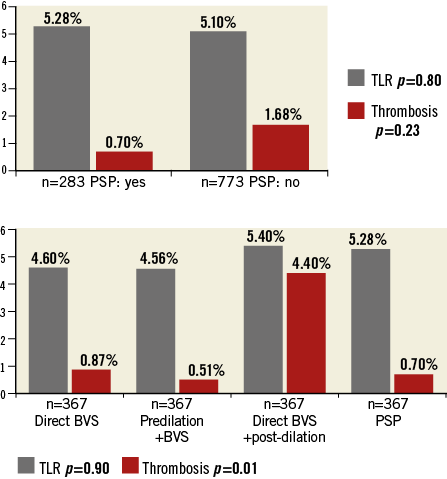
Figure 4. Impact of implantation technique on adverse cardiac events during follow-up. Rates of TLR and scaffold thrombosis in groups formed according to the technique used during BRS implantation. PSP: predilate, size and post-dilate; TLR: target lesion revascularisation. Adapted from: Everolimus eluting BRS. Impact of lesions complexity on clinical outcome and predictors of adverse cardiac events at long term follow-up. Suarez de Lezo et al10.
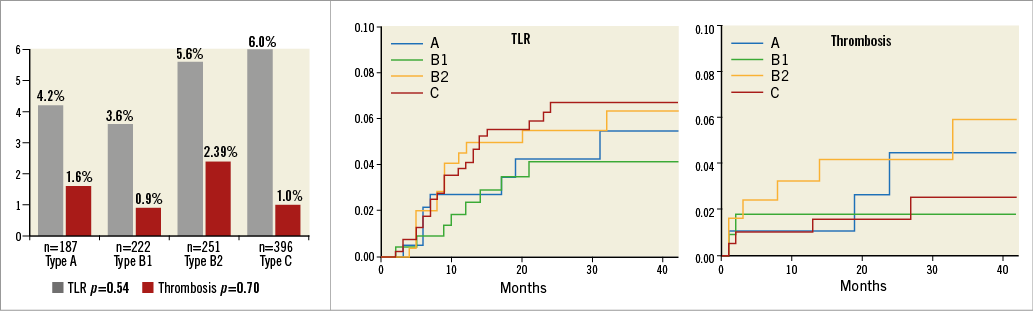
Figure 5. Impact of lesion complexity on adverse cardiac events during follow-up. Rates of TLR and scaffold thrombosis according to the type of lesion (left panel) and Kaplan-Meier curves of time to events for groups formed according to lesion complexity (right panel). Adapted from: Everolimus eluting BRS. Impact of lesions complexity on clinical outcome and predictors of adverse cardiac events at long term follow-up. Suarez de Lezo et al10.
This observation suggests that, if you do not prepare the lesion properly, and you insert your BRS and realise that you have not achieved full expansion, then the post-dilatation will not correct the problem in this subgroup. That would explain why this group had the worst outcome. Conversely, if it is a soft lesion, probably the direct BRS might do the trick, but this remains unpredictable and thus unsafe. At that point of the meeting, there was a long discussion about the appropriate moment to perform the intravascular imaging and a kind of consensus in the auditorium emerged, indicating that preparation should be first. When the preparation is adequate with full deployment, then the sizing should be performed, preferably with OCT, and only then should the scaffold be implanted. This is because the function of the scaffold is to tackle the disruption/dissection of the predilated/prepared lesion, not to dilate non-dilatable lesions. So, although they had no multivariate analysis and the statistical approach was rather simplistic, they concluded that diabetes mellitus, the use of clopidogrel, low ejection fraction and direct implantation followed by balloon post-dilatation increased the risk of BVS thrombosis. Further statistical treatment of these data should be conducted.
Conclusions
These two- to three-year follow-up reports seem to be heterogeneous; we went from the best result to the worst result and obviously the populations recruited were probably not really all-comers, real-world, consecutive patients, taking into account the large number of patients treated by these operators in the interventional suites during a period of one to three years and the relatively limited number of patients included in these registries. In the absence of a comparator, every number looks good, but the major finding of the randomised trials has been the exceptional track record of the XIENCE stent. The general impression was nevertheless that a very good technique plays a role and, from that point of view, the Milan group somewhat overshadowed the other series by their exceptional results. History has shown us many times that Antonio Colombo and his group were right in terms of treatment, using either bare metal or drug-eluting stents or now BRS. When this series is submitted to a peer review process, a combination of critical comments will certainly emerge but nevertheless on that day I learned a lot and I suspect that, with improved BRS technology and careful BRS implantation, probably monitored and guided by OCT, we will reach the “promised land”, which is not for tomorrow but for the day after.
Conflict of interest statement
P W. Serruys and Y. Onuma are members of the international advisory board for Abbott Vascular. A. Katsikis has no conflicts of interest to declare.