Abstract
Aims: Women and men suffering from coronary artery disease differ in their risk profiles. We sought to investigate the impact of sex on two-year outcomes after BVS implantation in routine clinical practice.
Methods and results: Sex-based analysis of clinical outcomes was carried out by pooling the individual patient data of the ISAR-ABSORB and KUM-ABSORB registries performed in four high-volume tertiary centres in Munich. Of the total of 1,032 patients, 259 (25.1%) were women. The primary composite endpoint of death, target vessel myocardial infarction (TV-MI) and target lesion revascularisation (TLR) up to two years occurred in 13.2% of women and 17.9% of men (p=0.12). Compared to men, women experienced numerically lower rates of TLR and definite or probable BVS thrombosis – 7.5% vs 12.4% (p=0.051) and 1.2% and 2.7% (p=0.20), respectively. Independent predictors of increased risk for TLR were use of smaller size BVS (HR 1.28, 95% CI: 1.02-1.62), while being a woman was a protective factor (HR 0.59, 95% CI: 0.35-1.00).
Conclusions: BVS used in a routine setting tend to perform better among women compared to men, which might be partially related to the lower complexity of their coronary artery disease.
Introduction
The recent evidence shows an attenuation of angiographic and clinical performance of the Absorb™ everolimus-eluting poly-L-lactic bioresorbable vascular scaffold (BVS) (Abbott Vascular, Santa Clara, CA, USA) particularly at longer term after its implantation1,2. Suboptimal implantation technique, BVS size selection and BVS resorption-related phenomena such as intraluminal scaffold dismantling, discontinuity and restenosis are considered the most plausible mechanisms for these findings3,4,5,6,7. In addition, BVS implantation in coronary vessels smaller than 2.25 mm and treatment of longer lesions have emerged as predictors of adverse outcomes3,8,9.
Among patients with coronary artery disease (CAD), women present with significantly smaller coronary vessels and less extensive and complex CAD compared to men10,11. However, there is a large body of scientific evidence demonstrating that women derive the same benefit from drug-eluting stent technology as men12,13. The sex-related performance of the BVS compared to everolimus-eluting stents (EES) has been investigated in a meta-analysis of four randomised trials enrolling very selected patients with stable CAD11. Its findings suggest a consistent relative treatment effect of BVS and EES for the two-year incidence of device- and patient-oriented cardiovascular outcomes in women and men11. However, data about the sex-related performance of BVS after implantation in a relatively unselected population are still lacking. Therefore, the aim of the current study was to assess the impact of patient sex on two-year outcomes after BVS implantation in routine clinical practice.
Methods
STUDY POPULATION AND PROCEDURE
We included all patients undergoing BVS implantation due to symptomatic CAD between September 2012 and July 2015 at four high-volume tertiary centres in Munich. The indication for percutaneous coronary intervention (PCI) was based on clinical symptoms and presence of significant angiographic CAD. The decision for selecting the BVS was left up to the operators. In general, less calcified lesions located in relatively large vessels were preferably treated.
Implantation of the Absorb everolimus-eluting poly-L-lactic BVS was carried out after mandatory lesion preparation (predilatation performed in 95% of the lesions). The BVS placement was carried out according to the manufacturer’s recommendations. The decision about post-dilatation and more aggressive lesion preparation was made at the operators’ discretion. If necessary, intravascular imaging was performed to optimise the post-interventional results. Antithrombotic treatment consisted of 250 mg iv aspirin, heparin 70-100 IU/kg and loading with an ADP receptor antagonist according to the clinical presentation and bleeding risk. After PCI, a maintenance aspirin dosage of 80-100 mg daily and additional clopidogrel 75 mg, or prasugrel 5-10 mg or ticagrelor 90 mg twice daily for six to 12 months (according to the clinical status at the index PCI) was recommended.
CLINICAL AND ANGIOGRAPHIC DATA MANAGEMENT
Per standard clinical practice, targeted medical history, physical examination, 12-lead ECG, laboratory tests (including cardiac biomarkers) at admission and at least 12 hours after PCI were performed. Clinical follow-up was performed at 1, 6, 12 and 24 months after PCI by phone call or at an out-patient clinic in case of symptom recurrence. A repeat angiogram was performed in 44.0% (n=114) of women and 43.7% (n=338) of men, either if clinically indicated or upon the recommendation of the referring physician, considering the fact that BVS is a new technology. All data collected at index PCI and thereafter were prospectively entered into the institutional database, based on a predetermined data set, by trained staff. Afterwards, data from the KUM-ABSORB and ISAR-ABSORB registries were transferred to the central clinical data management centre (ISAResearch Centre, Munich, Germany).
The quantitative coronary angiography (QCA) was performed off-line using the automated edge detection system software QAngio, version 7.3 (Medis medical imaging systems, Leiden, the Netherlands). The contrast-filled non-tapered catheter tip was used for calibration. Since the BVS is not visible, the platinum markers located 1 mm inside the BVS edges were used for orientation. Therefore, the position of stent markers in the QCA program were 1 mm outside the proximal and distal platinum markers. In-BVS and in-segment analyses (5 mm proximal and distal to the BVS margin) were performed. Interpolated reference vessel diameter and the following standard parameters were computed: reference diameter, in-lesion and in-segment minimal lumen diameter, in-lesion and in-segment percentage diameter stenosis.
ENDPOINT DEFINITION
The primary endpoint of this analysis was target lesion failure (TLF) – a composite of death, target vessel myocardial infarction (TV-MI) or ischaemia-driven target lesion revascularisation (TLR) at two years post index PCI. Secondary endpoints were the individual components of the primary endpoint as well as stent thrombosis rates according to ARC criteria at two-year follow-up. Major adverse cardiac events (MACE) were defined as a combination of death, any MI or any revascularisation. Myocardial infarction was defined according to the third universal definition14.
STATISTICAL ANALYSIS
The population was divided into two groups according to sex. Differences between groups were checked for significance using the Welch two-sample t-test or the Wilcoxon rank-sum test (continuous data) or the chi-square or Fisher’s exact test where the expected cell value was <5 (categorical variables). A two-tailed p-value <0.05 was considered to be statistically significant. Continuous data are presented as mean (standard deviation). Categorical data are presented as counts or proportions. Event rates were calculated according to the Kaplan-Meier method. Variable selection for the multivariate model was performed using the least absolute shrinkage and selection operator (LASSO) regression method provided in the R package glmnet after entering all baseline and procedural characteristics as candidates. A Cox proportional model was applied after entering a cluster term to account for the frequent presence of multiple treated lesions in the same patient. Statistical software, R statistics, Version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria) was used for analysis.
Results
PATIENT CHARACTERISTICS
Of the total 1,032 patients enrolled in this study, 259 (25.1%) were women. No significant differences between women and men were identified except for women being older and presenting less frequently with multivessel disease and complex lesions (Table 1, Table 2).
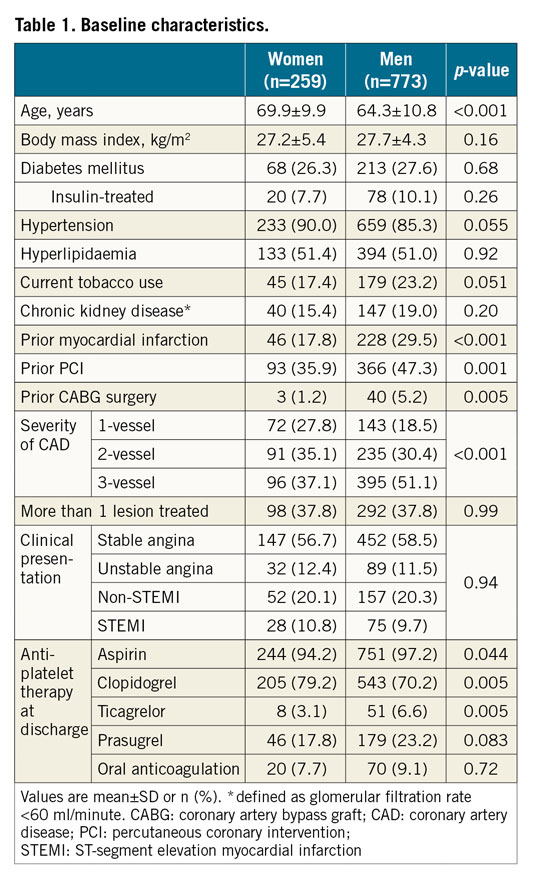
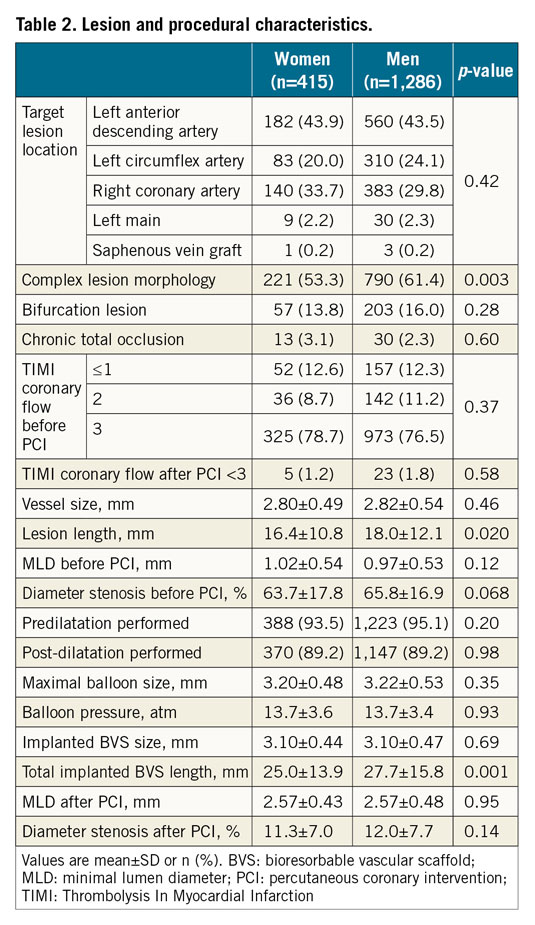
In total, 1,701 lesions were treated with BVS, 415 of them in women. No significant differences regarding lesion and procedural characteristics between women and men were observed except for a lower rate of complex lesions, shorter lesion and consecutively shorter stented segments among women (Table 2).
CLINICAL OUTCOMES
At two-year follow-up, no gender-specific differences in mortality were observed (p=0.79) (Figure 1, Table 3). The cumulative incidence of TLF (primary endpoint) was 13.2% in women and 17.9% in men at two years post index PCI, p=0.12 (Figure 2). Furthermore, TLR occurred less frequently among women compared to men (12.4% vs 7.5%, p=0.051). At one-year landmark analysis, there was a non-significant absolute difference of 2.7% in the TLF rate favouring women, which persisted between one and two years (∆TLF rate 2.3%). Similar figures were observed regarding TLR rates - ∆TLR rate of 2.3% within the first year and 3.0% between one and two years favouring women (Figure 3). Numerically lower rates of definite or probable BVS thrombosis were observed among women (Table 3, Figure 2).
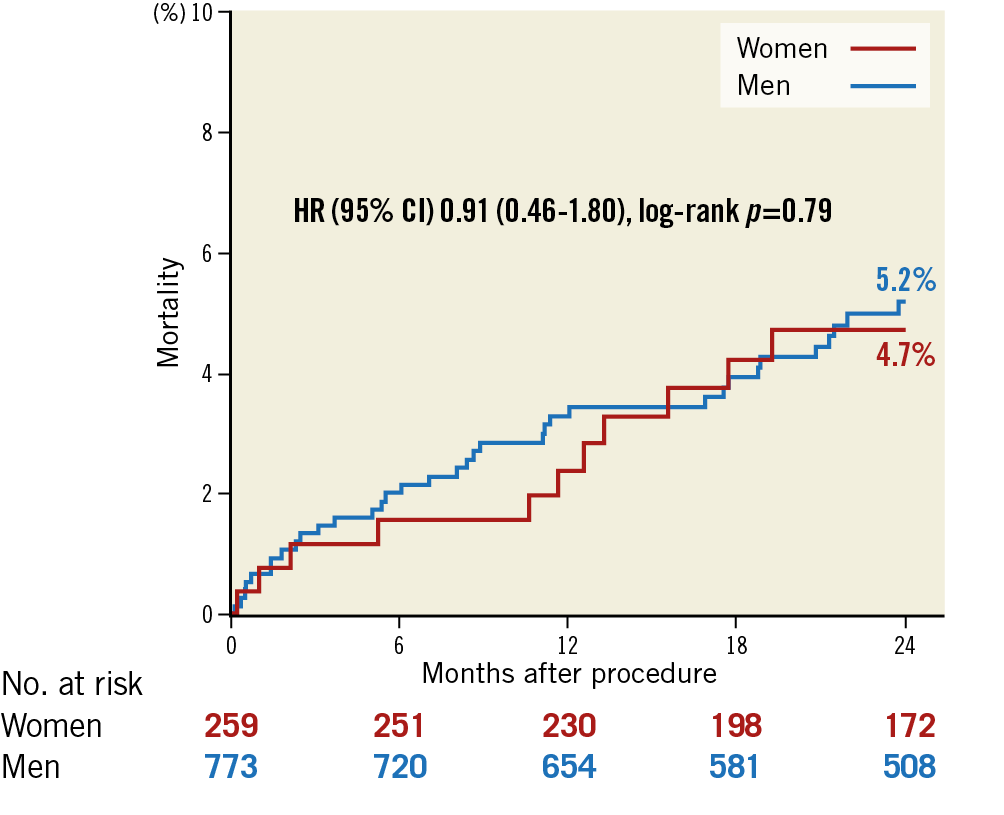
Figure 1. Mortality among women and men at two years after BVS implantation. CI: confidence interval; HR: hazard ratio
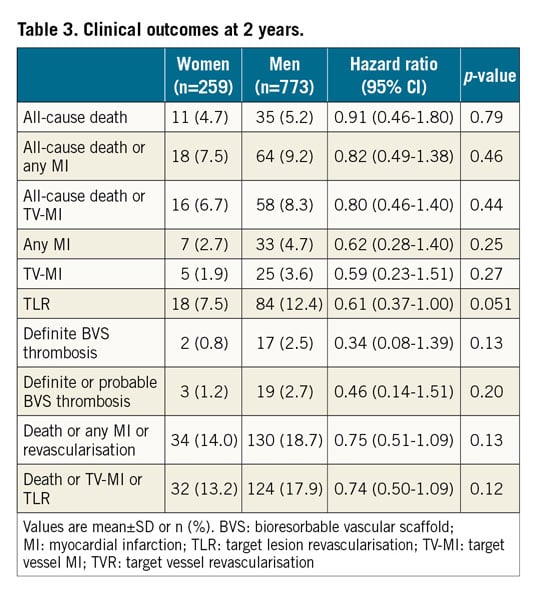
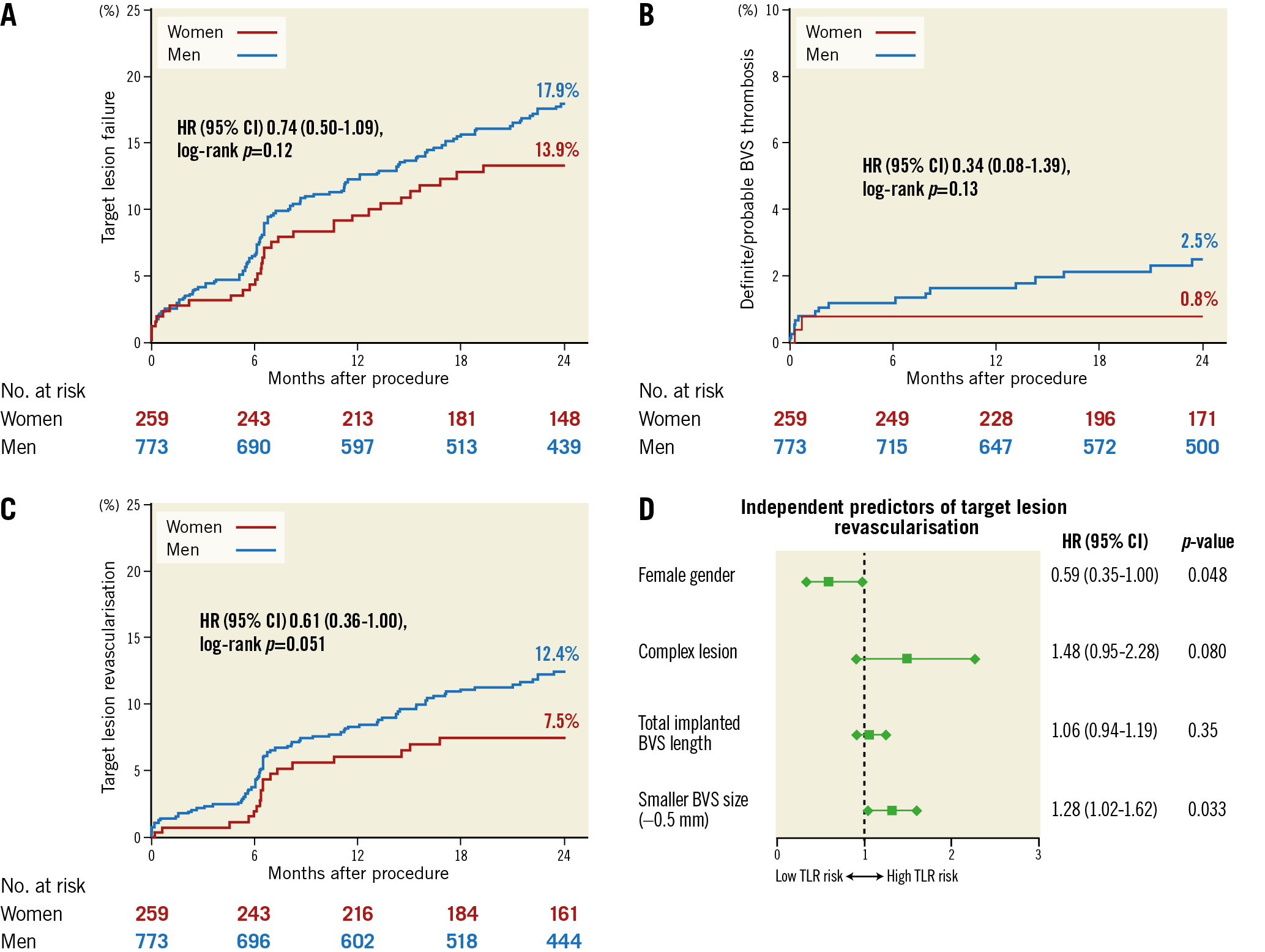
Figure 2. Clinical outcomes according to sex and independent predictors of target lesion revascularisation at two years after BVS implantation. A) Target lesion failure. B) Definite or probable BVS thrombosis. C) Target lesion revascularisation. D) Independent predictors of two-year TLR. BVS: bioresorbable vascular scaffold; CI: confidence interval; HR: hazard ratio
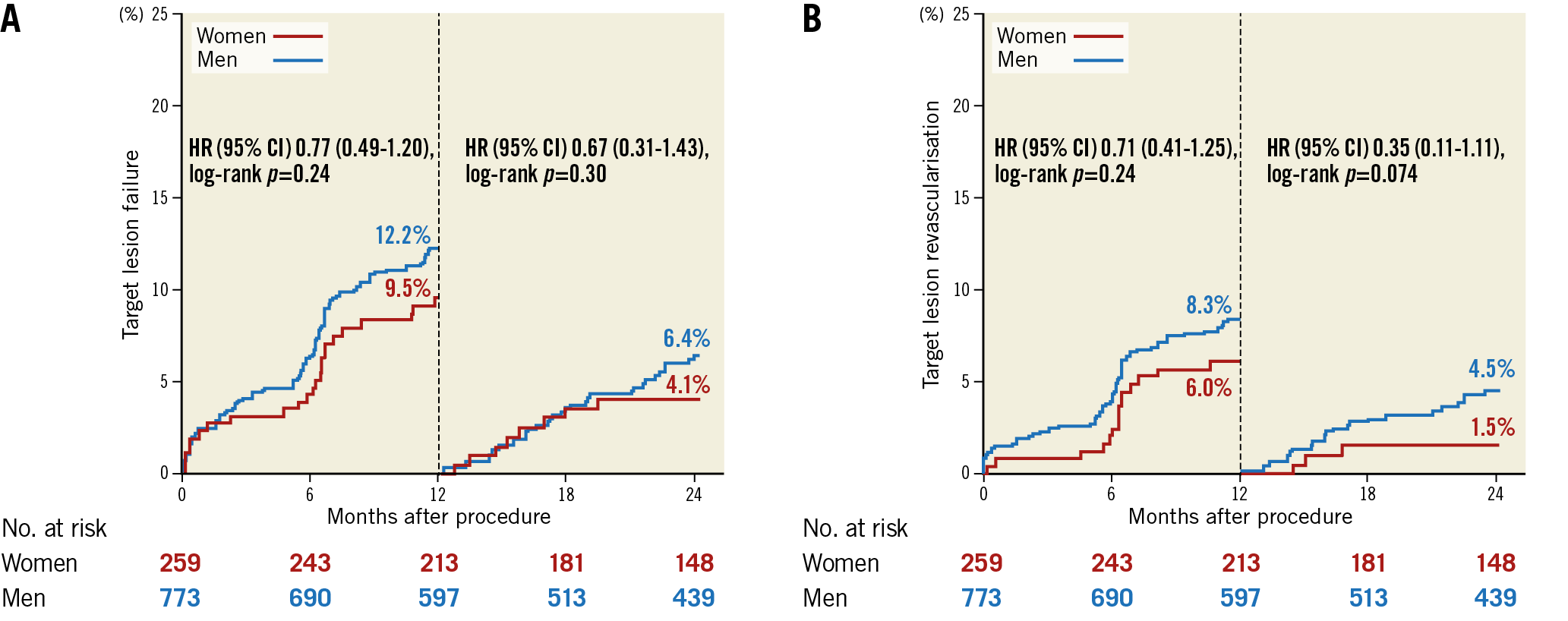
Figure 3. One-year landmark analysis for target lesion failure and revascularisation. A) Target lesion failure. B) Target lesion revascularisation. CI: confidence interval; HR: hazard ratio
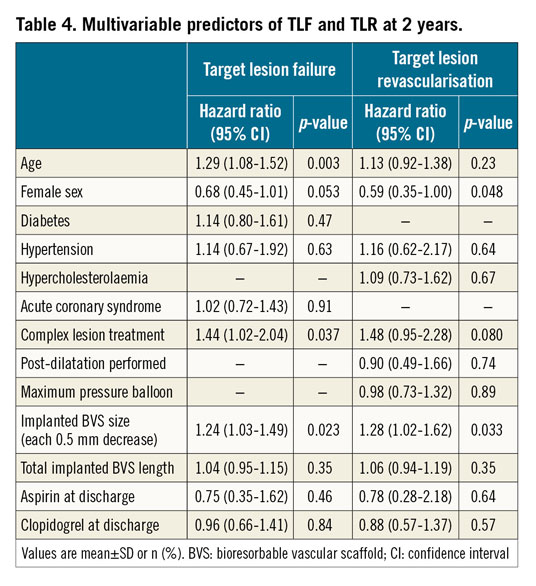
The selection of variables to be entered into the multivariable Cox proportional analysis for assessment of independent predictors of TLR and TLF was performed by the LASSO method, considering all variables from Table 1 and Table 2. Additionally, antiplatelet treatment at discharge was forced into the model. Age, complex lesion and implantation of small size BVS independently predicted two-year TLF, while two-year TLR was independently predicted by female sex and small size BVS (Table 4, Figure 2).
Discussion
The main findings of our study are: 1) at two years after BVS implantation, there are no sex-related differences in mortality and combined device- and patient-oriented clinical outcomes; 2) compared to men, women undergo repeat revascularisation numerically less frequently, driven by their lower risk of BVS thrombosis; 3) implantation of small size BVS was identified as an independent predictor of higher TLF and TLR risk; whereas 4) female sex is protective particularly for TLR.
Sex has been constantly reported to play an important role in outcomes after invasive diagnostic and therapeutic procedures among CAD patients10,12,15. Older age, higher aggregation of comorbidities, presence of frail and small size arteries prone to dissection and other vascular complications, increased bleeding risk as well as underuse of evidence-based treatment have frequently been identified as predictors of poorer outcomes among women compared to men13,15. On the other hand, women derive the same benefit from PCI and drug-eluting stent technology as men10,12,16. In a meta-analysis of randomised trials comparing BVS to EES, Shreenivas and colleagues reported a consistent relative treatment effect of BVS and EES for the two-year incidence of device- and patient-oriented cardiovascular outcomes in women and men11. In this very selected population of stable CAD patients, the incidence of TLF after BVS implantation was identical among women and men (8.9%)11. On the other hand, in our study women had a 26% lower risk of two-year TLF compared to men (13.2% vs 17.9%, p=0.12). These different findings are driven by the poorer baseline profile of patients included in our study, particularly among women – mean age 69.9 years vs 65.4 years; MI at presentation 31.0% vs 3.9%; multivessel CAD 72.2% vs 26.9%; treated vessel size 2.8 mm vs 2.6 mm; treated lesion length 16.4 mm vs 12.7 mm; total scaffold length 25.0 mm vs 19.0 mm. They reflect the constantly reported differences in patient selection policy among registries and randomised trials, particularly in the BVS era17. An overall two-year TLF rate after BVS implantation of between 3.2% and 20.8% reported in different randomised trials and registries is in line with our findings18,19.
An increased risk of BVS thrombosis at short- and long-term follow-up has been reported in registries and randomised trials1,2,8,20. The observed two-year BVS thrombosis rates of 1.2% among women and 2.7% among men are amongst the lowest reported in the BVS literature2,11. This is partially owing to the large size of the treated vessels, mandatory lesion preparation and the 95% rate of post-dilatation in our study.
Sex has not been shown to impact on the risk of thrombosis after implantation of metallic coronary stents with or without drug coating10,12,13. Our study suggests that BVS-treated women might be at lower risk of BVS thrombosis compared to their male counterparts. Within the BVS-treated patients of the above-mentioned meta-analysis and of the Amsterdam Investigator-Initiated Absorb Strategy All-Comers trial, the cumulative incidence of two-year BVS thrombosis was 1.3% and 1.7%, respectively, among women, and 2.0% and 4.2%, respectively, among men2,11. Furthermore, both these studies demonstrated a borderline interaction between sex and device type for the occurrence of two-year thrombosis, suggesting an increased risk of thrombosis with BVS compared to EES only among men. In our study, women experienced no BVS thrombosis between one and 24 months after PCI.
BVS are designed to overcome the limitations of DES technology – the ongoing device-related events even one decade after PCI21. Contrary to expectations, ongoing device-related events are observed up to three years after poly-lactic acid-based BVS implantation1,8. BVS elastic recoil due to the lower radial strength of poly-lactic acid-based BVS3,22, and ongoing inflammation accompanying the resorption process which promotes thrombosis and neoatherosclerosis might explain these findings7,23,24. The TLR rates in our study were 7.5% among women and 12.4% among men, which differ from rates reported in selected stable populations of randomised trials, 3.7% vs 4.8%, respectively11. In our relatively unselected population, the risk of ischaemia-induced TLR was 30% lower among women compared to men; the amount of this risk reduction doubles beyond the first year. Female sex emerges as the only independent predictor of TLR risk after BVS implantation.
We can only speculate about the possible mechanisms for this sex-related difference in BVS thrombosis and restenosis. First, the physical and design features of the BVS platform play an important role in vessel wall apposition and integration of BVS23,25,26. Women have less complex and calcified as well as shorter lesions which facilitates BVS sizing, placement and vessel wall apposition. Second, intraluminal scaffold dismantling and discontinuity during the resorption process leads to protrusion of strut fragments into the vessel lumen promoting thrombus formation3,4,5,23. Since this tissue is most probably inflammation-triggered fibrin deposition, it leads to impaired neointimal BVS strut coverage, late malapposition and neoatherosclerosis formation. Although there are no data about sex-related differences in vascular response to BVS implantation, a large animal study demonstrated temporal sex-related differences in the extent and timing of resolution of inflammation and fibrin clearance after DES implantation24.
Study limitations
Despite including all patients receiving BVS at our institutions, the current findings might be influenced by patient selection bias during decision making for BVS. Since women naturally present with smaller vessels, they might have been more frequently affected by the selection process. Intravascular imaging was only used in a very small percentage of patients and might have provided further information about the mechanisms of scaffold failure. Furthermore, although we report two-year outcomes of more than 1,000 patients, follow-up beyond the complete resorption time of BVS (three to four years) is needed to investigate the role of sex on the resorption process more fully.
Conclusions
BVS used in the routine setting tends to perform better among women compared to men, which is only partially related to the lower complexity of their coronary artery disease. However, larger patient cohorts and follow-up beyond the BVS resorption time are required to confirm the observed sex-related differences.
|
Impact on daily practice The observed lower incidence of repeat revascularisations and lack of late BVS thrombosis among women compared to men might suggest that women undergoing PCI for less complex lesions located in large coronary vessels are more suitable for BVS technology. |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Conflict of interest statement
J. Mehilli has received institutional grants from Abbott Vascular and Edwards Lifesciences and lecture fees from Abbott Vascular, Edwards Lifesciences, Boston Scientific, Biotronik, BMS and Terumo. A. Kastrati has submitted patent applications for drug-eluting stent technologies. R. Byrne has received lecture fees from B. Braun Melsungen, Biotronik, and Boston Scientific, and institutional research grants from Boston Scientific and HeartFlow. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.