Abstract
Aims: The aim of this study was to evaluate the safety and efficacy of percutaneous closure in patients with a ruptured sinus of Valsalva aneurysm (RSVA).
Methods and results: A total of 29 patients with RSVA were retrospectively enrolled in our study. All patients were successfully treated by percutaneous closure and had a complete closure at discharge; however, two patients had a trivial procedure-related aortic regurgitation (AR) after the procedure. On a mean follow-up of 29.7±23.8 months (range 1-83 months), the two procedure-related AR disappeared three months and two years after the procedure, respectively. Trivial residual shunt was found in one patient, sinus of Valsalva aneurysm ruptured again in one patient and trivial to moderate AR was found in two patients during the follow-up.
Conclusions: In appropriately selected patients with RSVA, percutaneous closure is an attractive alternative to surgery with high technical success and good short-term and midterm outcomes; however, long-term follow-up is mandatory.
Abbreviations
AR: aortic regurgitation
BAV: bicuspid aortic valve
IE: infectious endocarditis
LA: left atrium
LVEDD: left ventricular end-diastolic dimension
LVEF: left ventricular ejection fraction
MR: mitral regurgitation
MPA: main pulmonary artery
NCS: non-coronary sinus
NYHA: New York Heart Association
PDA: patent ductus arteriosus
RA: right atrium
RCA: right coronary artery
RCS: right coronary sinus
RSVA: ruptured sinus of Valsalva aneurysm
RV: right ventricle
SOVA: sinus of Valsalva aneurysm
TTE: transthoracic echocardiography
VSD: ventricular septal defect
Introduction
Sinus of Valsalva aneurysm (SOVA) is a rare congenital heart disease caused by congenital deficiency of muscular or elastic tissue in the aortic wall of the sinus of Valsalva. It is more prevalent in Eastern compared to Western populations and usually occurs in adolescence or early adulthood1. Patients with unruptured SOVAs are usually asymptomatic; however, once it ruptures into one of the heart chambers, it may cause aorta to heart chamber shunt with significant haemodynamic consequences and various symptoms, such as chest pain, palpitation, dyspnoea or even death. It may result in high mortality if left untreated, but it has a good prognosis after treatment; therefore, it requires immediate recognition and treatment. Surgical repair is the traditional treatment for ruptured sinus of Valsalva aneurysm (RSVA) and has a low mortality rate. However, since the first reported case of percutaneous closure of RSVA by Cullen et al in 1994 using a Rashkind umbrella device2, some case reports and case series related to this technique have been reported with encouraging follow-up results, and percutaneous closure has been an attractive alternative to surgery in appropriately selected patients3-6. However, to date, both large-scale and long-term follow-up results for this technique are scarce. Thus, in this study, we report our experience of RSVA in 29 patients to evaluate the safety and efficacy of percutaneous closure over a period of 83 months.
Materials and methods
PATIENTS AND DEVICES
From April 2005 to November 2015, a total of 29 patients with RSVA were treated by percutaneous closure in our hospital. Informed written consent was obtained from all patients. Additionally, another six patients with RSVA treated by percutaneous closure in our hospital were not included in the current study due to missing medical records and very limited information (containing only name, sex, age, rupture size and location and occluder type and size). Two kinds of occluder were used in this study: one was a domestic patent ductus arteriosus (PDA) occluder (Lifetech Scientific Co., Ltd., Shenzhen, China); the other was a domestic ventricular septal defect (VSD) occluder (Starway Medical Technology, Inc., Beijing, China). They are both made of nitinol wire mesh and are self-expanding.
PROCEDURE
Under local anaesthesia, the femoral arterial and venous introducing sheaths were inserted into the right femoral artery and vein percutaneously. A 5 Fr pigtail catheter was introduced into the left ventricle and aorta. Then, in the long axial oblique view and right anterior oblique view, the aortogram was carried out to delineate the origin, the rupture site, the size of opening and the anatomy of the RSVA (Figure 1A, Figure 1B, Figure 2A). The aortic and mitral insufficiency was also assessed. Based on the measurement of the aortogram, the appropriate occluder was selected. Next, an arteriovenous wire loop was established from the right femoral artery to the right femoral vein via the RSVA. Under the guidance of fluoroscopy and echocardiography, the occluder was introduced from the venous route and was deployed in the opening of the RSVA. Then the aortogram was repeated to confirm the occlusion of the RSVA and no significant AR resulting from the occluder. When the aneurysm originated from the right coronary sinus (RCS), selective right coronary arteriography was performed to make sure the ostium of the right coronary artery (RCA) was not affected. Once the position was confirmed as being acceptable, the occluder was finally released from the delivery cable (Figure 1C, Figure 2B, Moving image 1, Moving image 2).
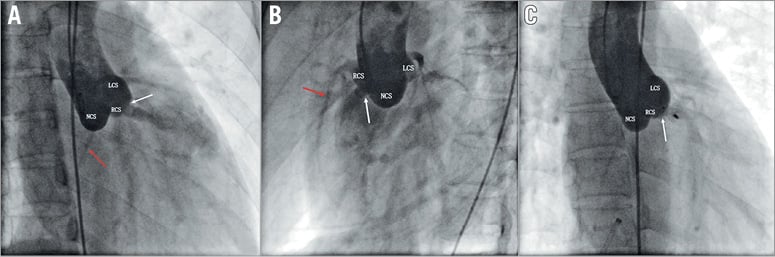
Figure 1. The right anterior oblique and long axial oblique views showing a right coronary sinus aneurysm rupturing into the right ventricle (A & B) and complete occlusion after device implantation (C) (white arrow: rupture site or device; red arrow: right coronary artery).
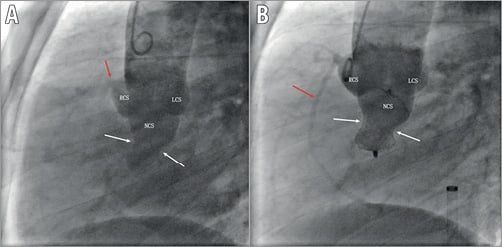
Figure 2. The long axial oblique view showing a non-coronary sinus aneurysm rupturing into the right atrium. The size of opening of the RSVA was about 14 mm (A). Complete occlusion with an 18/16 mm PDA occluder (B) (white arrow: rupture site or device; red arrow: right coronary artery).
FOLLOW-UP
All patients were advised to avoid strenuous activities, pay attention to rest and prevent colds. They received aspirin 200 mg once daily for six months after the procedure. They were followed at our outpatient clinic with physical examination, chest radiography and transthoracic echocardiography (TTE) postoperatively. Procedure-related AR was defined as the occurrence of any grade of new AR or worsening by more than one grade of pre-existing AR.
Results
BASELINE CLINICAL CHARACTERISTICS
The detailed baseline characteristics of the 29 patients are summarised in Table 1. There were 15 males and 14 females aged 13-72 years (mean±SD 38.8±15.4 years). Most patients (25/29) were in New York Heart Association (NYHA) Class I or II, three in Class III and one in Class IV (Figure 3). A continuous machinery-type murmur was heard at the left sternal border in all patients. Ten patients were asymptomatic; the major symptoms in the other patients were chest pain (13/29), palpitation (9/29), dyspnoea (8/29), oedema of both lower extremities (6/29), cough (3/29), dizziness (2/29) and headache (1/29). Three patients had a history of previous cardiovascular surgery, including surgical repair of VSD (1/29, 11 years ago), percutaneous closure of PDA (1/29, 10 years ago) and surgical repair of aortic dissection (DeBakey type II) (1/29, four years ago). Associated lesions were VSD (2/29), bicuspid aortic valve (BAV) and mild AR (1/29), moderate mitral regurgitation (MR) (1/29), mild pericardial effusion (1/29) and trivial to mild AR (8/29). TTE revealed RSVA from the RCS into the right ventricle (RV) in seven and right atrium (RA) in 12 and right atrium and ventricle (RAV) in one, and non-coronary sinus (NCS) into RA in eight and RV in one (Figure 4). The diameter of the opening of the RSVA ranged from 3 to 14 mm (mean 6.4±2.4 mm) as measured by TTE or angiography.
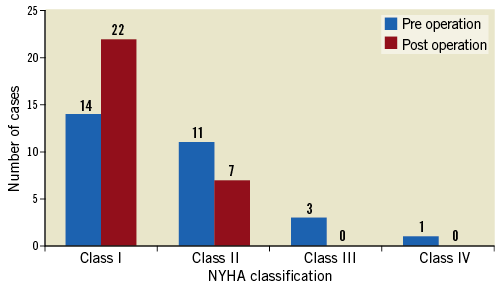
Figure 3. NYHA classification of patients at baseline and at the time of last follow-up (p=0.005).
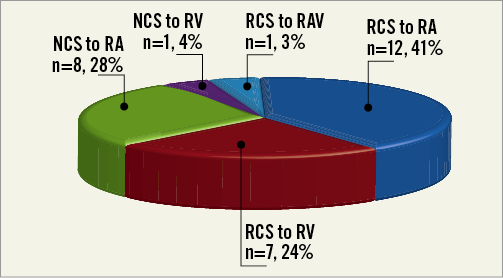
Figure 4. The characteristics of the ruptured and drainage sites for RSVA. NCS: non-coronary sinus; RA: right atrium; RAV: right atrium and ventricle; RCS: right coronary sinus; RV: right ventricle
PROCEDURAL OUTCOMES AND FOLLOW-UP EVALUATION
The detailed clinical results are summarised in Table 1. All of the 29 patients had successful occlusion of the RSVA, with PDA occluders used in 28 patients and a VSD occluder in one patient. The size of the selected occluder was 2-8 mm (mean 4.3±1.7 mm) larger than the diameter of the opening of the RSVA which was measured by TTE or aortic root angiography. No procedure-related death, myocardial infarction, bleeding or haematoma, embolisation, or other complications occurred during the operation except that two patients had a trivial procedure-related AR after the procedure (cases 4 and 9). They were discharged one to nine days (mean 2.6±1.9 days) after the procedure with improved symptoms. Trivial to mild residual shunt was found in two patients but disappeared the next day and the fourth day before discharge, which was confirmed by TTE (cases 3 and 13). All patients had a complete closure at discharge.
On a mean follow-up of 29.7±23.8 months (range 1-83 months), 22 patients were in NYHA Class I and seven patients were in Class II (p=0.005) (Figure 3). The two procedure-related AR disappeared three months and two years after the procedure, respectively. Trivial to moderate AR was found in two patients at one- and at three-month follow-up (cases 11 and 22). Trivial residual shunt was found in one patient after six months of follow-up (case 21). Notably, one severe complication occurred in case 26: the patient complained of chest pain and dyspnoea for one month after six years of follow-up. TTE revealed a new rupture in the same sinus of Valsalva. The rupture size was about 4 mm; no history of infection or AR was recorded in the electronic medical records. This patient was subsequently referred for surgical repair. No other complications, such as haemolysis, infectious endocarditis (IE), device embolisation or death, were found during the follow-up period.
Echocardiography results shown in Figure 5 indicate, in general, a trend towards decreasing left ventricular end-diastolic dimension (LVEDD) and left atrium (LA) size, and no obvious trend towards decreasing right ventricle (RV) and main pulmonary artery (MPA) during the follow-up. It is noteworthy that there was a trend towards decreasing left ventricular ejection fraction (LVEF) in the early stage after the operation, but LVEF gradually increased to the pre-operation level during the follow-up.
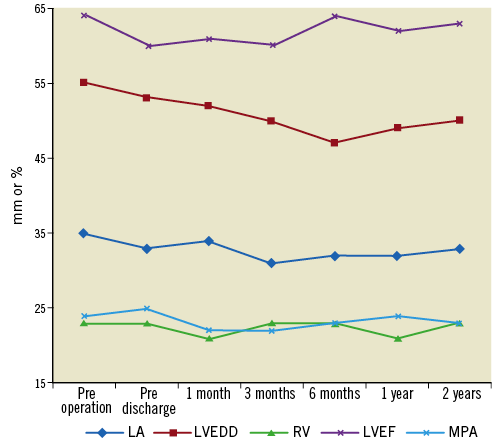
Figure 5. Echocardiographic results pre operation and change during follow-up after the procedure.
Discussion
SOVAs are rare cardiac anomalies which may be congenital or acquired, comprising 0.1% to 3.5% of all congenital cardiac defects7. Over the past two decades, with the advances in intervention techniques, percutaneous closure has been validated as being a safe and effective alternative to surgery in appropriately selected patients; however, evaluation in multicentre studies, with larger sample size and longer follow-up, is mandatory3-6,8-11. To the best of our knowledge, this is the largest case series of patients with RSVA undergoing percutaneous closure. In the current study, we retrospectively analysed the safety and efficacy of percutaneous closure in 29 patients with RSVA with a mean follow-up of about 30 months. The results indicate that percutaneous closure is a safe and effective procedure in appropriate patients with RSVA. All patients had successful occlusion of the RSVA and complete closure at discharge, with improved symptoms. There was no procedure-related mortality and there were no other major complications. Three minor complications, including trivial to moderate AR (2/29) and trivial residual shunt (1/29), and one severe complication (new rupture of SOVA) occurred, and internal diameters of the LA and LVEDD were restored during the follow-up. In our experience, the operative technique of percutaneous closure of RSVA is not very complicated; however, appropriately selected patients and suitable devices are vital to achieve good clinical outcomes.
PATIENT SELECTION
RSVA is frequently combined with other cardiac lesions such as VSD, AR or BAV8,12. It is generally accepted that RSVA combined with VSD is a contraindication to percutaneous closure4,13. However, in this study, two patients had RSVA combined with VSD: one was subarterial while the other was perimembranous. These were successfully treated by percutaneous closure, while the VSDs were left untreated due to the small defect size (only 2 mm). Therefore, we suggest that RSVA combined with VSD might not be an absolute contraindication to percutaneous closure, especially when the VSD size is small and depending on the VSD location. Liu et al8 suggest that patients with RSVA combined with subarterial VSD should be referred for surgical repair, while those with RSVA combined with perimembranous VSD could be considered eligible for percutaneous closure. Thus, more cases are needed to confirm the indications of percutaneous closure for RSVA combined with VSD. Three patients with AR preoperatively remained unchanged and preoperative AR had disappeared in five patients during the follow-up period. One patient with BAV and mild AR was successfully treated by percutaneous closure; the pre-existing AR did not progress or regress during the follow-up. Therefore, RSVA combined with trivial to mild AR is not a contraindication to percutaneous closure. There may be benefits from this procedure due to remodelling of the sinus following endothelialisation8. Besides, RSVA combined with moderate MR and mild pericardial effusion may also be eligible for percutaneous closure as indicated by this study.
Percutaneous closure of RSVA may be especially appropriate for patients with previous surgical repair or interventional therapy. In this study, three patients had previous cardiovascular surgery (cases 9, 14 and 27). They were all successfully treated by percutaneous closure and avoided the risk of thoracotomy or a second thoracotomy. For patients with poor cardiac function (NYHA Class III and IV) but without anomalies requiring surgical repair, who need to be treated, percutaneous closure might be a better choice because of its advantages of less trauma and haemorrhage and rapid recovery. In case 22, the size of the opening was 14 mm, and an 18/16 mm PDA occluder was successfully deployed to close the lesion; however, mild AR occurred one month after the operation and progressed to mild-to-moderate AR 58 months after percutaneous closure. Thus, we suggest that a size of opening less than 10 mm may be more appropriate for the percutaneous closure method. In particular, in cases 21 and 24, the RCS had three and two rupture sites, the sizes of the openings were 7-8 mm and 4-6 mm, and they were closed with a 14 mm VSD occluder and a 10/8 mm PDA occluder, respectively. However, in case 21, trivial residual shunt occurred six months after the procedure. Therefore, we should be very careful to determine which method (surgical repair or percutaneous closure) should be used in these kinds of patients. RSVA with multiple rupture sites may not be an absolute contraindication to percutaneous closure6; however, surgical repair may be a better choice, so more cases are needed to confirm the indications or contraindications of percutaneous closure in patients with RSVA involving multiple rupture sites.
DEVICE SELECTION
Selection of a suitable device is essential for the efficacy of percutaneous closure of RSVA; however, no device has yet been specially designed for this rare anomaly. Since the first reported case of percutaneous closure of RSVA by Cullen et al2 in 1994 using a Rashkind umbrella device, various case reports have been published using PDA occluders, VSD occluders and AMPLATZER™ septal occluders (ASO; St. Jude Medical, St. Paul, MN, USA), etc.3,4,8,11,14. However, PDA occluders are believed to be the most suitable for percutaneous closure of RSVA, because the RSVA commonly has a “windsock” appearance, with a broader aortic end. It has been reported that PDA occluders are the most commonly deployed and have proved to be safe and effective3-5,9,15. Of 29 successful patients in this study, 28 patients were occluded with PDA occluders and only one patient with multiple rupture sites was occluded with a VSD occluder. It is believed that the size of occluder should be 1-4 mm larger than the diameter of the aortic opening of the RSVA4,13. In this study, the mean diameter of the rupture opening was 6.4±2.4 mm, and the size of the selected occluder was 2-8 mm (mean 4.3±1.7 mm) larger than the diameter of the opening of the RSVA. We consider that it is a rational strategy to upsize the device for a relatively larger rupture opening because of the relatively flimsy margin5. However, two principles should be adhered to, namely (i) the device should be firmly attached to the rupture site, and (ii) there should be no impairment to adjacent structures, such as the aortic valve and the opening of the coronary artery.
COMPLICATIONS
To date, reports concerning complications after percutaneous closure of RSVA are scarce. Residual shunt, haemolysis, procedure-related AR and failure to deploy are important complications of percutaneous closure in patients with RSVA which have been described in the literature so far3-5,8,9,14. Three kinds of complications occurred in this study, comprising AR, residual shunt and recurrence of RSVA. To the best of our knowledge, this is the first reported case of recurrence of RSVA in the literature. This might be due to the pre-existing deficiency of the sinus of Valsalva involved and progression during the follow-up, or the tendency to multiple rupture due to congenital deficiency. Residual shunt is probably due to the cardiac erosion or slight displacement of the device. AR occurrence could be due to: (i) the traction on the aortic annulus due to device weight, especially when the size of defect is large and an oversized device is used, (ii) structural change of the sinus or slight deformity of the cusps due to the device implanted in the aortic sinus, or (iii) an acute increase in the systemic vascular resistance as a result of disconnection of a low resistance pulmonary circuit from the systemic circulation16.
Limitations
This study demonstrates good results of percutaneous closure of RSVA; however, this study also has some limitations. First, this is a single-centre, retrospective study. Some data could not be found in the electronic medical records, such as Qp/Qs, pulmonary artery pressure before and after the procedure, and the distance between the defect and the opening of the right coronary artery. Some patients did not have strict follow-up after the operation. This study would have been more powerful and informative if these data had been available, so the experience and results of our single-centre study may not be universally representative. Second, this study is a relatively large series of percutaneous closure of RSVA with a mean follow-up of about 30 months. The short-term and midterm clinical outcomes are encouraging, but long-term outcomes are still not very clear; therefore, a larger sample size with a long-term follow-up is mandatory.
Conclusions
In appropriately selected patients with RSVA, especially in those with isolated RSVA, a size of opening less than 10 mm, single rupture site, trivial to mild AR and previous cardiovascular surgery, percutaneous closure is a safe and effective alternative to surgical repair with high technical success and encouraging short-term and midterm outcomes; however, long-term follow-up evaluation is mandatory.
| Impact on daily practice 1. The operative technique of percutaneous closure in patients with RSVA is not very complicated; however, appropriately selected patients and suitable devices are vital to achieve good clinical outcomes. In our experience, patients with isolated RSVA, a size of opening less than 10 mm, single rupture site, trivial to mild AR and previous cardiovascular surgery are eligible for percutaneous closure. There is no uniform standard for device selection; different consideration should be given for each patient. The general principle is that the device should be as small as possible on the premise that the device is very stable and efficient for the RSVA. 2. Although the short-term and midterm follow-up clinical results are encouraging, long-term follow-up is still necessary. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. The procedure of percutaneous closure during the operation (case 3).
Moving image 2. The procedure of percutaneous closure during the operation (case 22).