Abstract
Aims: To evaluate the safety and efficacy of percutaneous closure (PC) using modified double-disc ventricular septal defect (VSD) occluders in patients with ruptured sinus of Valsalva aneurysm (RSVA).
Methods and results: Between 2005 and 2012, 25 patients were enrolled in our study for attempted PC. There were five patients (20%) with RSVA combined with VSD and two (8%) with aortic regurgitation (AR). The median age was 45 years (24-74 years). The QP/QS was 2.4±0.6 (1.6-4.0). The median diameter of lesions was 6 mm (4-8 mm) while the median size of occluders was 8 mm (6-12 mm). Twenty-three patients (92%) underwent PC successfully. Occluders were retrieved in two patients within one week. Trivial residual shunts developed in three and mild occluder-related AR occurred in five at discharge. During a median follow-up of 19 months (6-96 months) all trivial residual shunts vanished and mild occluder-related AR disappeared in four out of five patients. The proportion of patients in NYHA Class III/IV was reduced from 72% at baseline to 12% at the time of last follow-up (p<0.001).
Conclusions: In selected patients with RSVA, PC using modified double-disc occluders may become a valuable alternative to surgery with encouraging immediate outcomes and midterm results.
Introduction
Ruptured sinus of Valsalva aneurysm (RSVA), a rare cardiac lesion, is usually caused by a congenital deficiency of muscular and elastic tissue in the aortic wall of the sinus of Valsalva or acquired after infective endocarditis, atherosclerosis, and aortic dissection1. The incidence of RSVA is relatively higher in adolescence and adulthood in Asian countries compared to Western countries2. More frequently, aneurysm of the right coronary sinus (RCS) or non-coronary sinus (NCS) is involved and ruptures into the right ventricle (RV) or right atrium (RA)3,4. Rupture is often of abrupt onset and causes chest pain, acute heart failure and even sudden death.
Surgical repair has been the mainstay of therapy with relatively low mortality5,6. However, some problems limit the application of surgical treatment: for instance, severe haemodynamic instability increases the risk of operation, a patch leak requires a second operation. Percutaneous closure (PC) of RSVA was first reported by Cullen in 1994 using a Rashkind device7. Since then, Amplatzer occluders and similar devices have been reported, mainly as case reports or small series8-11. To gain greater knowledge, we undertook this multicentre study to assess the immediate outcomes and midterm follow-up results of PC using modified double-disc ventricular septal defect (VSD) occluders in patients with RSVA.
Methods
PATIENT SELECTION
Consecutive patients with RSVA in five institutions from 2005 to 2012 were included in our study. Patients were considered candidates for PC if they had the European system for cardiac operative risk evaluation II (EuroSCORE II) >20%, or if surgery was deemed to be of excessive risk. The EuroSCORE II calculator is online at http://www.euroscore.org/calc.html. The following indication criteria were used: (i) age >18 years; (ii) maximum diameter of the ostium ≤12 mm by echocardiography; (iii) EuroSCORE II >20%; (iv) patients associated with other cardiac defects amenable to PC.
A total of 25 patients were enrolled for attempted PC. Transthoracic echocardiography (TTE) was routinely performed before the procedure. In some cases, transoesophageal echocardiography (TEE) was used to improve visualisation of the anatomy. The ethics committees of five hospitals approved the study and the choice of PC was discussed with the patient and valid informed consent was obtained.
CLOSURE DEVICE
The occluders used were modified double-disc VSD occluders (Shanghai Shape Memory Alloy Ltd, Shanghai, China), which were designed based on the Amplatzer occluder and had been widely used for selected VSD in China12. Three types of occluders were used in the study: small-waist double-disc, muscular and asymmetric occluders. The diameter of the small-waist double-disc occluder is different in the left (aortic) and right side disc (Figure 1A). The diameter of the left disc is 8 or 12 mm larger than that of the waist, while the right disc is 4 mm larger than that of the waist (A4B2 or A6B2 occluder). The waist length of the occluder is 3.5 mm. The muscular occluder is used for RSVA with a tubular shape (Figure 1B). The length of its connecting waist is 10 mm. The diameters of the left and right discs are 10 mm and 6 mm larger than that of the waist, respectively (mA5B3 occluder). The asymmetric occluder is used for the coexistent VSD (Figure 1C). The diameter of its left disc is 6 mm larger than that of the waist. The left disc extends towards the apex and no superior margin extends towards the aorta. The waist length of the asymmetric occluder is 3.5 mm. The above modified double-disc occluders were approved by the State Food and Drug Administration (SFDA) of China in 2003, and received CE mark in 2008.
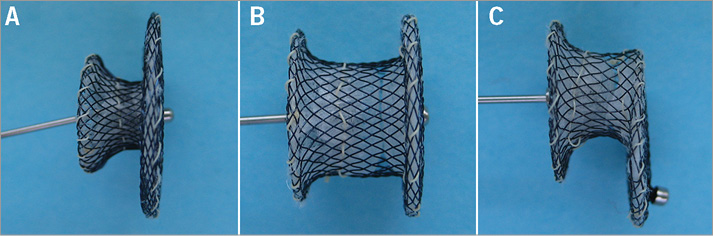
Figure 1. Three types of modified double-disc occluders used in the study. A) Lateral view of the small-waist double-disc occluder. B) Lateral view of the muscular occluder. C) Lateral view of the asymmetric occluder.
PERCUTANEOUS DEVICE IMPLANTATION
PC was performed under fluoroscopic and TEE guidance as described before13. Unfractionated heparin (100 IU/kg) and antibiotic prophylaxis were injected intravenously before the procedure. Right heart catheterisation was performed to assess the ratio of pulmonary to systemic flow (QP/QS) and obtain haemodynamic data in the RV and pulmonary artery. Aortic root angiography was performed using a 6 Fr pigtail catheter to observe the size, shape and opening of the RSVA (Moving image 1). An arterial-venous wire loop was established from right femoral artery, ascending aorta, RSVA, RV, RA, inferior vena cava and right femoral vein. A 9 to 10 Fr delivery sheath was placed into the ascending aorta across the lesion over the loop.
We chose an appropriately sized occluder which measured 2 to 4 mm larger than the entrance diameter of the RSVA. The selected occluder with its attached delivery cable was then inserted through the delivery sheath from the venous route, and its aortic disc was deployed in the ascending aorta. A gentle traction was exerted on the delivery cable to confirm seating of the left disc on the aortic side without slippage into the RSVA. Then the rest of the occluder was deployed on the right side across the lesion (Moving image 2). The device was released after making certain that there was no significant aortic regurgitation (AR), tricuspid regurgitation or encroachment on coronary arteries (Moving image 3, Moving image 4).
After the procedure, all patients were transferred to general wards and administered aspirin 3 mg/kg per day for six months. TTE and electrocardiography were performed one week later and patients were routinely assessed at one, six and 12 months after the procedure and yearly thereafter. The residual shunt was defined as trivial (<1 mm colour jet width), small (1-2 mm colour jet width), moderate (3-4 mm colour jet width) or large (>4 mm colour jet width) by TTE14. Valve regurgitation was evaluated by colour Doppler flow imaging in a standard way.
Statistical analysis
All continuous variables are expressed as mean values and standard deviation or median with range as appropriate, and discrete variables are presented as percentages. Univariate analysis was performed by the Student’s t-test and chi-square test or Fisher’s exact test. A p-value <0.05 was considered statistically significant. The data were analysed with statistical software SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
Results
PATIENT CHARACTERISTICS
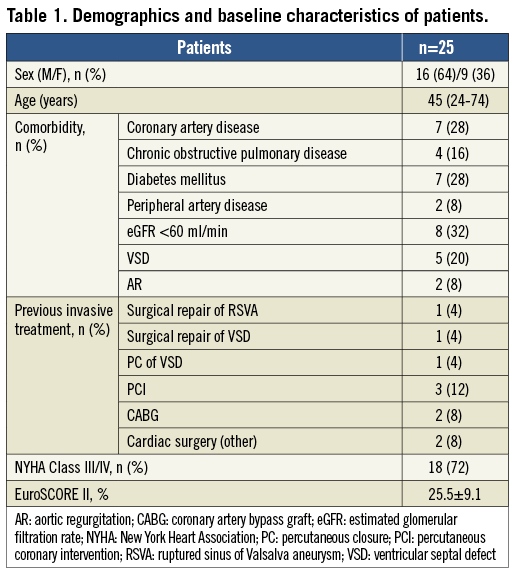
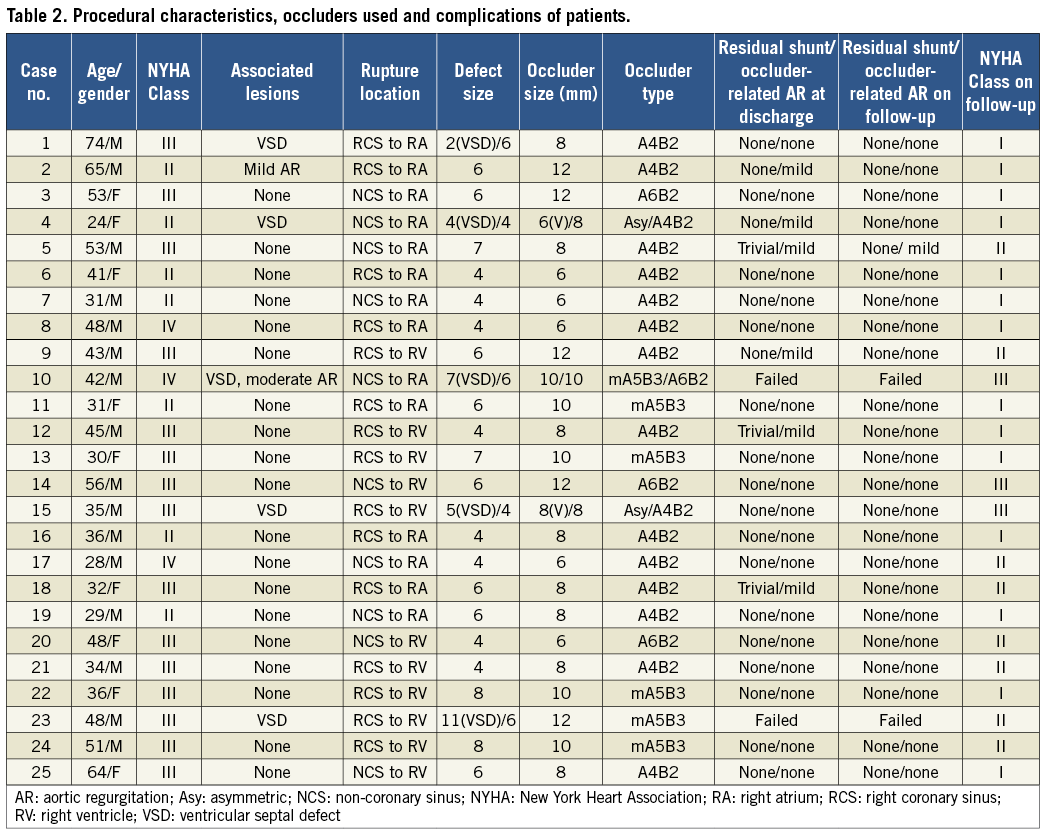
Baseline characteristics of patients are summarised in Table 1. The median age of 25 patients was 45 years (24-74 years). Major symptoms were chest pain in 14 (56%) and dyspnoea in 19 patients (76%). There were five patients (20%) with RSVA combined with VSD and two (8%) with AR. The mean EuroSCORE II was 25.5%±9.1%.
PROCEDURAL OUTCOMES
Procedural outcomes are summarised in Table 2. Echocardiography revealed RCS ruptured into RA in seven (28%) and RV in eight (32%), while NCS ruptured into RA in seven (28%) and RV in another three patients (12%). PC was successfully performed in 23 out of 25 patients (92%).
There were five patients (cases 1, 4, 10, 15 and 23) with RSVA combined with perimembranous VSD. Two (cases 4 and 15) were successfully treated for RSVA and VSD concomitantly (Figure 2). In case 1, combined with a small perimembranous VSD (less than 3 mm in diameter), the patient was only treated for RSVA. In cases 10 and 23, occluders were initially deployed successfully; nevertheless, severe haemolysis developed postoperatively.
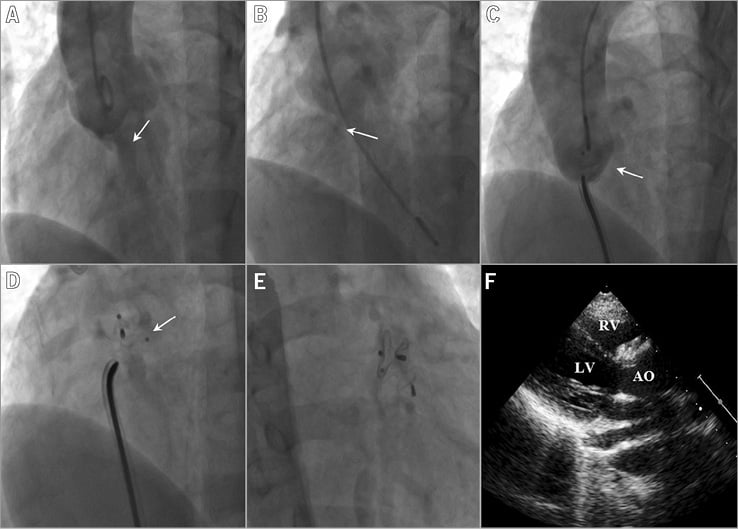
Figure 2. Angiography and echocardiographic evaluation in case 4 showing an RSVA combined with a VSD. A) Angiography reveals the shunt jet crossing the ruptured site (white arrow). B) Angiography reveals the shunt jet from left to right ventricle (white arrow). C) An A4B2 occluder (white arrow) for RSVA is deployed. D) An asymmetric occluder (white arrow) for VSD is deployed. E) Fluoroscopy reveals two occluders for RSVA and VSD are implanted successfully. F) Echocardiography also reveals two occluders for RSVA and VSD are well positioned. AO: aorta; LV: left ventricle; RSVA: ruptured sinus of Valsalva aneurysm; RV: right ventricle; VSD: ventricular septal defect
In case 9 the patient had previously undergone surgical repair of perimembranous VSD. At one-week follow-up, the shunt from left ventricle (LV) to RV disappeared but the shunt from RCS to RV was found by TTE. The patient was successfully treated for RSVA using a 12 mm A4B2 occluder. In case 13 the patient had previously undergone PC of VSD using a symmetric occluder. Seven years later she had a ruptured site of RCS into RV and was treated using a 10 mm mA5B3 occluder.
In case 6 the patient had a giant RSVA from RCS to RA, measuring 41×34 mm at the maximal echocardiographic diameters15. The giant sac was adjacent to the tricuspid valve. TTE revealed that the entrance diameter was 4 mm, and a 6 mm A4B2 occluder was deployed successfully.
In case 24 the patient had a patch leak following surgical repair of RSVA 20 years before. He presented with palpitations during a 20-year follow-up. Two occluders including one Amplatzer duct occluder (ADO) and one muscular occluder were used to close the leak two years before. With the moderate residual leak still existing, a third 10 mm mA5B3 occluder was implanted and the residual shunt finally vanished (Figure 3).
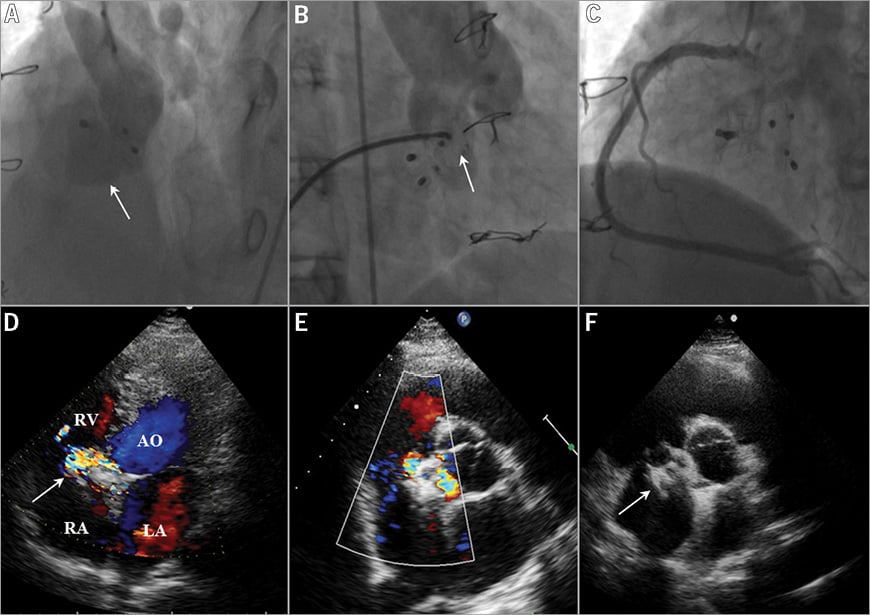
Figure 3. Angiography, coronary arteriography and echocardiographic evaluation in case 24 showing a patch leak following surgical repair of RSVA 20 years before. A) Angiography reveals the residual shunt jet crossing the ruptured site (white arrow) following surgical repair and two-occluder implantation of RSVA. B) The third muscular A5B3 occluder (white arrow) for RSVA is deployed successfully. C) Right coronary arteriography is performed to make certain that the implantation of three occluders does not interfere with the opening of the right coronary artery. D) Echocardiography reveals residual shunt from right coronary sinus into right ventricle (white arrow) with turbulent colour flow across following surgical repair and two-occluder implantation of RSVA. E) Following implantation of the third occluder, there is a complete closure with no colour flow. F) Echocardiography reveals three occluders (white arrow) for RSVA are implanted successfully. AO: aorta; LA: left atrium; RA: right atrium; RSVA: ruptured sinus of Valsalva aneurysm; RV: right ventricle; VSD: ventricular septal defect
COMPLICATIONS DURING HOSPITALISATION
Trivial residual shunts at discharge were noticed by TTE in three patients. Five patients developed de novo mild occluder-related AR at discharge. In case 2 the patient with mild AR preoperatively remained unchanged at discharge.
Three occluders were retrieved in two patients (cases 10 and 23) within one week after PC for severe haemolysis. In cases 10 and 23, angiography revealed very large and long funnel RSVA combined with VSD. PC of RSVA was undertaken using a muscular and an A6B2 occluder in case 10 and a muscular VSD occluder in case 23. Moderate residual shunt occurred immediately and severe haemolysis developed four hours and eight hours after the procedure. They had not recovered after conservative treatment for one week and finally converted to surgery (Figure 4).
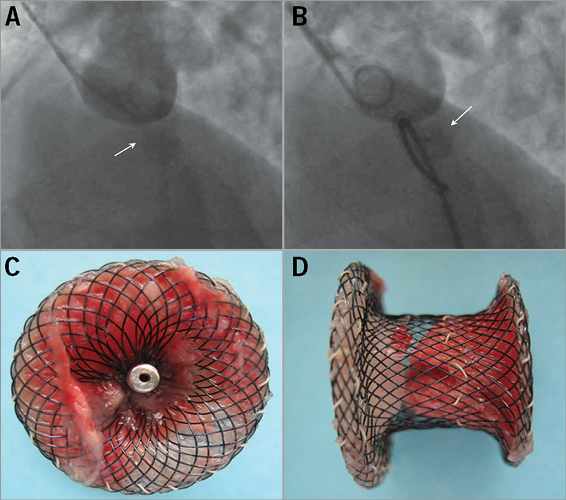
Figure 4. Angiography and the removed occluder in case 23 presenting with severe haemolysis. A) Angiography in case 23 reveals the shunt jet crossing the ruptured site (white arrow) before the procedure. B) A muscular A5B3 VSD occluder is deployed with moderate residual shunt (white arrow). C) Front view of the removed muscular occluder. D) Lateral view of the removed muscular occluder. VSD: ventricular septal defect
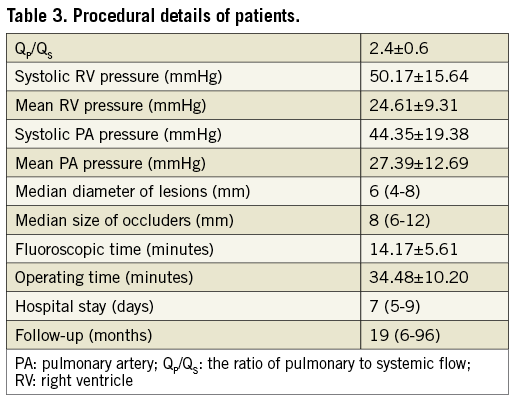
PROCEDURE DETAILS
Procedure details are summarised in Table 3. The QP/QS was 2.4±0.6 (1.6-4.0). The median diameter of lesions measured by echocardiography was 6 mm (4-8 mm). The median size of occluders used was 8 mm (6-12 mm). No patient was transferred to the intensive care unit or required blood transfusion after device deployment.
FOLLOW-UP EVALUATION
No deaths, device embolisation, de novo residual shunts or AR occurred during a median follow-up of 19 months (6-96 months). Trivial residual shunts disappeared in all patients during the follow-up. Mild occluder-related AR disappeared in four out of five patients and remained unchanged in case 5.
At baseline, NYHA functional Class was II in seven patients, III in 15 and IV in three. At the most recent follow-up, 14 patients were in NYHA Class I and eight in NYHA Class II (Figure 5). Three patients with combined coronary artery disease were still classified in NYHA Class III. The proportion of patients in NYHA Class III/IV was reduced from 72% at baseline to 12% at the time of last follow-up (p<0.001).
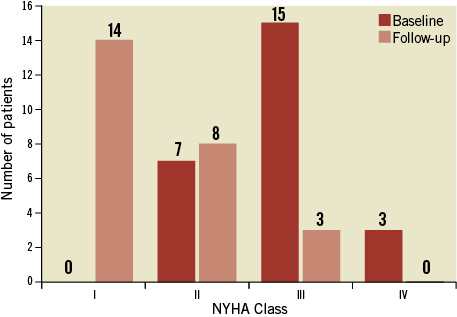
Figure 5. New York Heart Association (NYHA) classification of patients at baseline and at the time of last follow-up.
Discussion
RSVA is a life-threatening event and requires immediate intervention. Open surgical repair is a widely accepted procedure with relatively low mortality. However, in some patients with high risk of operation, the surgical approach is limited and successful PC is increasingly being reported. In the present study, we evaluated the immediate outcomes and midterm follow-up results of PC using modified double-disc occluders for RSVA in a large multicentre series of patients with a EuroSCORE II of >20%.
Safety and effectiveness of percutaneous approach
The efficacy and safety of ADO in PC of RSVA have been confirmed previously. A success rate has been reported between 90% and 100% during a midterm follow-up16,17. Unlike the previously reported studies, we utilised the modified double-disc occluders, which have been widely used in perimembranous VSD in China12. The shape of this occluder recovers well after release and does not occupy enough space to affect aortic valve function. The total occlusion rate using modified double-disc occluders was 92% during the median follow-up of 19 months. The proportion of patients in NYHA Class III/IV was reduced from 72% at baseline to 12% at the time of last follow-up (p<0.001). Our experience suggests that PC using modified double-disc occluders can also be performed successfully in these high-risk patients achieving encouraging outcomes.
Case and occluder selection
PC of RSVA may be especially appropriate for cases with previous surgical repair. In our study, one case (case 9) of RSVA occurred after surgical repair of VSD and another case (case 24) of patch leak developed following surgical repair of RSVA. Both of them resolutely refused the second sternotomy. In case 9, the shunt from RCS to RV was found at one-week follow-up after surgical repair of VSD. It was considered as iatrogenic RSVA and an A4B2 occluder was deployed to close the lesion successfully. In case 24, we used three occluders to close the residual leak successfully. To our knowledge, this is the first reported case that has applied three occluders to close the residual leak after surgical repair. Implantation of three occluders had the potential of interfering with the opening of the right coronary artery and cusps of aortic valves. Occluders could only be released after an adequate position was obtained on the basis of aortic root angiography and selective right coronary arteriography.
Our results also showed that the presence of giant RSVA did not prevent occluder closure. In case 6, the patient was diagnosed as having a giant sac (41×34 mm) of the RCS to RA. The giant sac was successfully treated using an A4B2 occluder15. The postoperative follow-up was uneventful and subsequent TTE showed a satisfactory closure of the giant RSVA. To the best of our knowledge, this is the largest size recorded in a patient with RSVA undergoing PC successfully.
The most frequent coexistent cardiac lesion in RSVA is VSD, which has been reported between 25.8% and 55%18,19. It is widely accepted that RSVA combined with VSD is a contraindication to PC17. Encouraged by the excellent outcomes of PC of isolated RSVA, we offered PC for the selected RSVA combined with VSD using a small-waist double-disc occluder and an asymmetric occluder, respectively. The small-waist matches with the entrance diameter of the RSVA. Its left disc is large enough to extend and does not occupy enough space to affect aortic valve function. The right disc of the occluder can cover the exit of the RSVA completely. The asymmetric occluder, also named the zero eccentricity occluder was shown to be suitable for the VSD with its rim close to the aortic annulus20. In cases 4 and 15 the orifices of RSVA and perimembranous VSD were successfully obliterated using A4B2 occluders and asymmetric occluders, respectively. Therefore, we suggest that RSVA combined with VSD might not be an absolute contraindication to PC. RSVA with perimembranous VSD could be considered eligible for PC. After making certain that there was neither interference between two occluders nor an effect on aortic valve function on the basis of echocardiographic and angiographic evaluation, occluders could be released to close the lesions of RSVA and VSD. However, in RSVA combined with subarterial VSD, patients should resolutely be referred for surgical correction. However, more cases are needed to confirm the indications of the percutaneous approach for RSVA combined with VSD.
Next to VSD, AR is another commonly associated lesion and occurs in 17% to 75%21. In the present study, patients with RSVA combined with severe AR were excluded. Two patients with associated mild and moderate AR were enrolled for attempted PC. In case 2 the patient with mild AR preoperatively remained unchanged after the procedure and the mild AR had disappeared at the time of last follow-up. In case 10, the patient with moderate AR was converted to surgical retrieval due to severe haemolysis after the procedure. Therefore, RSVA with moderate AR might be more appropriate for simultaneous surgical repair and aortic valve repair or replacement. Besides, progressive AR is also a crucial factor influencing prognosis22. In our study, five patients developed de novo mild occluder-related AR. This might have been due to the slight deformity of the aortic cusps related to the occluder or the sudden increase in afterload caused by disconnection of the low resistance pulmonary circuit. Mild AR disappeared in four out of five patients and remained unchanged in case 5 during the follow-up. We speculated that the chronic adaptation to the increased afterload or remodelling of the sinus following endothelialisation could result in lesser traction on the cusps by the occluder and the recovery of aortic valve function.
Serious complications
Serious complications of PC for RSVA in our study were rare. Severe haemolysis occurred in two patients. In cases 10 and 23, angiography revealed very large and long funnel RSVA combined with VSD shunt. Two muscular occluders and one A6B2 occluder were deployed for RSVA, and moderate residual shunt occurred immediately. The occurrence of haemolysis might be due to the unsuitable selection of occluders and high pressure flow from the VSD. With moderate residual shunt occurring during the procedure, one should withdraw the occluders and convert the patients to surgery immediately.
Limitations
Our study demonstrated good results of PC of RSVA in patients with a high risk of operation; nevertheless, it had some limitations. First, it was a retrospective study and the follow-up duration was short. The endothelialisation of the occluder could make surrounding tissue stronger but it may not halt the progression of the malformation or the risk of further fistula formation. There exists the risk of repeated rupture for the presence of abnormal tissue. Second, randomised trials assessing the efficacy of the antiplatelet treatment after PC have not been carried out. In our study, postprocedural aspirin was prescribed for about six months to prevent systemic clot formation. No patient developed occluder embolisation or infective endocarditis during the follow-up.
Conclusions
The immediate outcomes and midterm follow-up results of PC using modified double-disc occluders in patients with RSVA were inspiring in the present multicentre study. The percutaneous approach for RSVA is an attractive alternative to surgery in patients with a high risk of operation. PC may also be appropriate for cases with previous surgical repair. Besides, RSVA with perimembranous VSD could be considered eligible for percutaneous treatment. In order to refine the patient selection for the percutaneous approach, we would like to undertake a multicentre study to compare the percutaneous and surgical treatment of RSVA in the future.
| Impact on daily practice Ruptured sinus of Valsalva aneurysm (RSVA), a rare cardiac lesion, is a life-threatening disease and requires immediate treatment. Surgical repair for RSVA has been the mainstay of therapy with relatively low mortality. Unfortunately, it also carries some risk of serious complications and is limited in patients with high risk of operation. However, over the past ten years, it has been increasingly reported that percutaneous closure for RSVA is an attractive and successful alternative to surgery in patients with RSVA. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Aortic root angiography was performed to observe the size, shape and opening of ruptured sinus of Valsalva aneurysm.
Moving image 2. The occluder was inserted through the delivery sheath and deployed across the lesion.
Moving image 3. Repeat angiography showed that there was no residual flow.
Moving image 4. The occluder was released and well positioned.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Aortic root angiography was performed to observe the size, shape and opening of ruptured sinus of Valsalva aneurysm.
Moving image 2. The occluder was inserted through the delivery sheath and deployed across the lesion.
Moving image 3. Repeat angiography showed that there was no residual flow.
Moving image 4. The occluder was released and well positioned.