Abstract
Aims: Renal denervation (RDN) with radiofrequency (RF) is being used to treat resistant hypertension (rHTN). As 15-30% of treated patients are non-responders to RDN, we investigated whether RDN with cryoenergy can serve as a second-line option.
Methods and results: Ten non-responder patients (mean age 55 years, six male) with rHTN were treated with cryoenergy for RDN. In order to qualify as non-responders, patients had to show systolic 24 hr ambulatory BP (ABP) ≥150 mmHg (median ABP 183/102 mmHg, median office-based BP [OBP] 191/108 mmHg) despite treatment with ≥4 different antihypertensive drugs (mean 6), and further not show a reduction of systolic ABP ≥10 mmHg at ≥3 months after RDN with RF. The three/six/12-month follow-up (FU) comprised clinical and biochemical evaluation, OBP and ABP measurement. Additionally, at six months, duplex sonography was performed. Cryoablation with a 7 Fr cryoablation catheter (Freezor® Xtra; Medtronic, Minneapolis, MN, USA) was performed in all patients without complications (four applications in both renal arteries, every four minutes, temperature –75°C). At three, six, and 12 months we found a reduction in systolic OBP of –41/–47/–61 mmHg (n=10/7/6; p=0.044 for all), diastolic OBP of –18/–14/–34 mmHg, systolic ABP of –38/–35/–52 mmHg (n=9/7/6, p=0.014 for all), and diastolic ABP of –20/–13/–18 mmHg (p=0.043 for all), respectively. During FU, no complications occurred and the renal function remained unchanged.
Conclusions: The significant reduction in systolic OBP and ABP observed qualifies RDN with cryoenergy as an effective second-line therapeutic option in non-responders to RDN with RF.
Introduction
Arterial hypertension (HTN) is one of the most important modifiable risk factors for cardiovascular morbidity and mortality1,2. In recent decades, the use of antihypertensive drugs has revolutionised the therapy of HTN. However, about 50% of patients show suboptimal control of their blood pressure (BP), despite adequate pharmacological (drug combinations) and non-pharmacological treatment (i.e., lifestyle modification, avoidance of interfering substances). These patients are at increased risk for cardiovascular events3,4. If pharmacological therapy (with at least three antihypertensive drugs including a diuretic in appropriate doses) fails to reduce the office-based BP (OBP) to below 140/90 mmHg, patients are considered to suffer from drug-resistant HTN2,5. The prevalence of drug-resistant HTN has been estimated to range between 8% and 13% of all antihypertensive drug-treated patients6. The catheter-based renal denervation (RDN) technique with radiofrequency (RF) has been developed as a new treatment option for drug-resistant HTN. The reasons for the rather rapid introduction of this method in the therapy of drug-resistant HTN were the reported high efficiency and safety of the procedure. The effectiveness of this technique in lowering BP was demonstrated in the landmark studies Symplicity HTN-1 and HTN-2, and also in the EnligHTN-1 study by using special RF ablation catheters7-9. More recently, it was shown that endovascular ultrasound or even a standard electrophysiology (EP) catheter can also be used effectively for RDN10-13. In 2014, the results of Symplicity HTN-3, the first blinded study with the largest number of patients treated with RDN, were published. Disappointingly, this study did not show differences in systolic BP reduction between treatment and control groups14. However, in the context of the study characteristics and the way it was conducted, there are several concerns about inexperienced operators in the field of RDN (most operators performed only three or fewer than three RDN procedures), the study population with a high number of Afro-Americans (who respond better to sham procedure than to RDN), and the medical treatment of the patients (not truly on stable antihypertensive drug treatment)15. Thus, one should be cautious before invalidating the previous RDN studies because of one negative trial such as Symplicity HTN-3. The conclusion should rather be that more, well-conducted, randomised clinical trials are needed before a definite conclusion about the beneficial effect of RDN in the treatment of HTN can be drawn. On the other hand, according to the results of different trials, including Symplicity HTN-3, RDN seems to be safe7,8,12,14,16. Procedure-related complications of catheter-based RDN therapy were rare, even during long-term follow-up (FU)17,18. Nevertheless, even in the positive studies, 15-30% of treated patients are non-responders (defined as failure to achieve a decrease in systolic OBP >10 mmHg) to this therapy7,8,12,16,19,20.
Animal studies which our group conducted with the aim of exploring alternative energy sources demonstrated that RDN with cryoenergy was more effective in reducing the density of neurofilament (NFL)-positive nerves in the renal artery than RF current21,22. The reduction of these NFL-positive nerves is a surrogate marker for the attenuation of sympathetic hyperinnervation23. Based on these findings, the aim of the current study was to investigate whether cryoablation of the renal artery as second-line therapy is effective in lowering the BP in non-responders to RDN with RF.
Methods
PATIENT SAMPLE
Non-responders to RDN with RF were included in our study. More specifically, in order to qualify as non-responders, patients had to show a mean systolic BP ≥150 mmHg in the 24 hr ambulatory blood pressure (ABP) measurement despite medical treatment with at least four antihypertensive drugs including a diuretic (except in one patient with end-stage renal disease), and also not show a reduction of the mean ABP ≥10 mmHg at ≥3 months following RDN therapy. None of the patients had untreated obstructive sleep apnoea (OSAS), primary hyperaldosteronism, renal artery stenosis, pheochromocytoma, Cushing’s syndrome, aortic isthmus stenosis, aortic regurgitation or other secondary causes of arterial HTN.
STUDY PROCEDURE
Baseline evaluation of patients comprised clinical history, review of medication, physical examination, basic blood chemistries (including serum creatinine and proteinuria), OBP and ABP measurement. All patients were treated with cryoenergy for second-line RDN. RDN with cryoenergy has been described in detail previously24. Briefly, renal angiography via left femoral access was performed, using a Judkins Right (JR4) catheter (Cordis, Johnson & Johnson, Warren, NJ, USA) to exclude renal artery stenosis (defined as narrowing of the renal artery lumen by 50% or greater)25. After puncture of the right femoral artery, we introduced a 7 Fr 6 mm tip cryoablation catheter (Freezor® Xtra; Medtronic) into the renal artery without using a guiding sheath (Figure 1). By reducing the temperature to approximately –75°C for four minutes, four cryoablation lesions were created in both renal arteries, consecutively. Advancing or withdrawing and rotating the catheter in a stepwise manner separated the lesions longitudinally as well as rotationally after each cryo application. During the ablation, we continuously monitored the temperature. Follow-up assessments were performed at three, six and 12 months during visits to our out-patient clinic. Clinical and biochemical evaluation, as well as OBP and ABP measurement were carried out at baseline and at each FU visit, whereas renal duplex sonography was performed at baseline and at six-month FU. The local ethics committee approved the treatment protocol and all patients provided written informed consent.
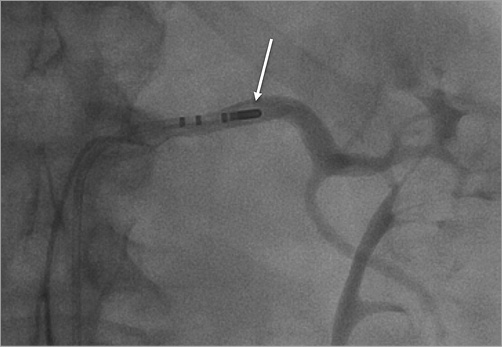
Figure 1. Renal angiography during cryoablation in the left renal artery shows typical ice ball formation on the catheter tip (white arrow). Focal renal artery irregularities occurred immediately following the cryoablation in six patients which were not flow-limiting at procedure termination.
STATISTICAL ANALYSIS
Central tendencies of BP changes are reported as median and variations as quartiles. The non-parametric Friedman test was used to analyse the differences in median systolic or diastolic OBP and ABP between baseline and FUs. Subsequent single comparisons between baseline and three-month FU were conducted by Wilcoxon signed-rank tests, utilising a Bonferroni correction for repeated testing (for a nominal 0.05 level the actual significance level was set at p<0.025). The statistical analyses were computed with SPSS statistical software (SPSS Inc., Chicago, IL, USA).
Results
STUDY POPULATION
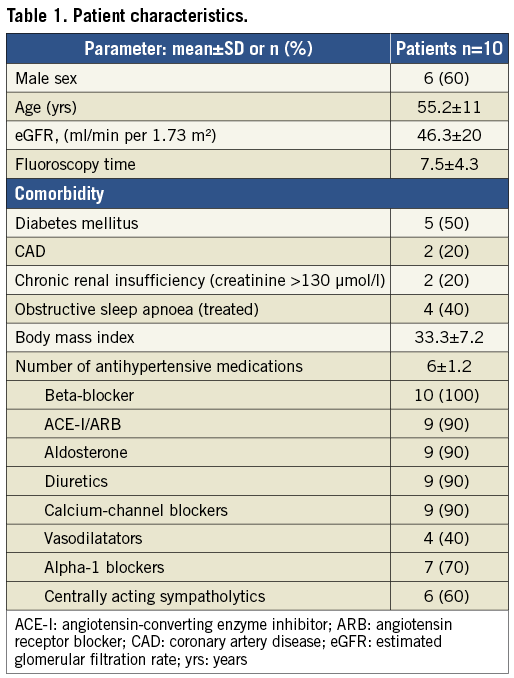
In this study, 10 patients (mean age 55 years, six male) with severe drug-resistant HTN (median OBP 191/108 mmHg, median ABP 183/102 mmHg) despite treatment with ≥4 different antihypertensive drugs (mean 6) in maximal doses, at least three months (more specifically: three patients after three months, three patients after six months, one patient after nine months, and three patients after 12 months) following a previously performed RDN procedure with RF current were treated with cryoenergy for second-line RDN. All of the patients insisted on their adherence to the antihypertensive drug treatment. Some of our patients had a severe comorbidity (five patients with diabetes mellitus, two patients with coronary artery disease, two with chronic renal insufficiency [defined as creatinine >130 µmol/l], four with treated OSAS). The mean BMI of the patients was 33.3±7.2. Baseline parameters of the patients are shown in Table 1.
RDN PROCEDURE
We performed four cryo applications along the length of both renal arteries up to four minutes each with a temperature drop down to –75°C (ranging between –65°C and –78°C) in nine of our patients. In one patient the cryoablation catheter could only be introduced in the right renal artery because of anatomic problems. The mean fluoroscopy time was 7.5±4.3 minutes. Patients received intravenous narcotic and sedative drugs (0.1 mg fentanyl and 2-4 mg midazolam) against the diffuse abdominal pain, and anticoagulation consisting of 100 units of heparin per kg and 500 mg aspirin to prevent thrombus formation. Subsequently, 100 mg aspirin per day was given for at least three months.
Interestingly, the pain during ablation was limited to the initial (first seconds) temperature drop. In all patients, the pain disappeared immediately after reaching the final temperature. The final angiography at the end of the procedure showed only focal renal artery irregularities (six patients) which were never flow-limiting. No renal artery dissections occurred. One patient developed a pseudoaneurysm of the femoral artery after the procedure with the need of surgical vessel reconstruction (stitch). In all other patients we did not observe any renal vascular complications during the 12 months of FU.
BLOOD PRESSURE CHANGES
The overall effect of RDN with cryoenergy on systolic OBP and ABP and diastolic ABP was significant, as were the subsequent Wilcoxon tests for systolic and diastolic ABP as well as systolic OBP at three-month FUs.
In the OBP measurement, there was a reduction of median BP values of –41/–18 mmHg (n=10) at three-month, –47/–14 mmHg (n=7) at six-month, and –61/–34 mmHg (n=6) at 12-month FU (Figure 2). In the ABP measurement we also observed a significant BP reduction of median BP values of –38/–20 mmHg (n=9) at three-month, –35/–13 mmHg (n=7) at six-month, and –52/–18 mmHg (n=6) at 12-month FU (Figure 3). According to the OBP, six of seven patients were BP responders at six months, and six of six patients were BP responders at 12 months (defined as a decrease in median systolic OBP ≥10 mmHg) after RDN with cryoenergy. In the ABP measurement, six of seven patients were responders at six, and four of six patients were responders at 12 months (defined as a decrease in median systolic ABP ≥10 mmHg) following RDN with cryoenergy. The absolute changes in median OBP and ABP are shown in Table 2. At six-month FU, three patients had reduced (–3; –2; –2) and one patient had increased (+2) antihypertensive medication. In all other patients the antihypertensive medication remained unchanged. In all patients the renal function remained unchanged (creatinine 102±40 µmol/l at baseline vs. 93±31 µmol/l, and proteinuria 1,585 mg/24 hrs vs. 804 mg/24 hrs at six-month FU).
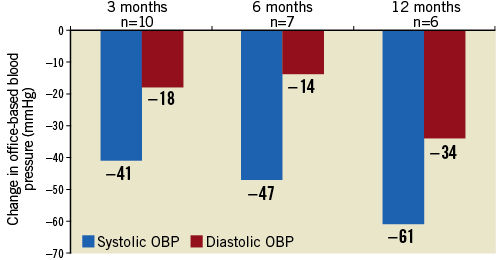
Figure 2. Median systolic and diastolic BP changes in the OBP following renal denervation at three, six, and 12-month FU. Overall, there was a statistically significant blood pressure reduction following renal denervation with cryoenergy in systolic OBP, χ2 (3)=8.100, p=0.044, but not in diastolic OBP, χ2 (3)=6.231, p=0.101. Subsequent single comparisons between baseline and three-month FU conducted by Wilcoxon signed-rank tests showed significant BP changes in systolic OBP, p=0.018. n: number of patients; OBP: office-based blood pressure
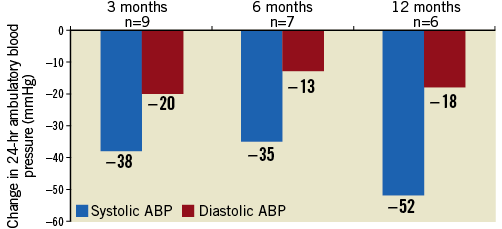
Figure 3. Median systolic and diastolic BP changes in the ABP following renal denervation at three, six, and 12-month FU. Overall, we found a statistically significant blood pressure reduction following renal denervation with cryoenergy in systolic ABP, χ2 (3)=10.837, p=0.013, and also in diastolic ABP, χ2 (3)=8.143, p=0.043. Subsequent single comparisons between baseline and three-month FU conducted by Wilcoxon signed-rank tests showed significant BP changes in systolic ABP, p=0.012 and also diastolic ABP, p=0.012. ABP: ambulatory blood pressure; n: number of patients

Discussion
In this study, we investigated the efficiency of cryoenergy for RDN as a second-line option in non-responders to RDN with RF. In all treated patients, a previous RDN procedure with RF current failed to reduce the systolic ABP by more than 10 mmHg and the median systolic ABP remained above 150 mmHg. We found that in these patients RDN with cryoenergy was effective in the reduction of OBP as well as ABP.
RF current and cryoenergy are competing methods in the treatment of cardiac arrhythmias. Recently, it was shown that the use of cryoenergy in comparison to RF current resulted in a significant reduction of pain and discomfort during ablation of supraventricular arrhythmias without reduction of the treatment efficacy26,27. On the other hand, phrenic nerve palsy is a complication that is not uncommon during cryoballoon ablation of patients with atrial fibrillation28,29. This dreaded side effect of cryoablation, the impairment of remote nerves, is a desired treatment goal during RDN. In animal experiments, we found that cryoablation was more effective in the reduction of NFL-positive nerves than RF current21,22. In fact, we found a total loss of NFL in the cryoablation lesions22. This might be one pathophysiological explanation of the observed BP reduction following RDN with cryoenergy in former BP non-responders to RDN with RF current.
A second issue that needs to be discussed in this paper is the discrepancy of BP reduction observed in clinical RDN trials depending on whether OBP or ABP measurement was used to evaluate the efficiency of RDN30. Although most RDN trials reported a striking reduction in OBP, a point of criticism is the fact that, if ABP was available (which was rarely the case), the results of both BP assessments differed31. In 2013, Mahfoud and co-workers published observational data of BP changes following RDN with the thus far largest sample of patients (n=346) with resistant HTN treated with RF for RDN. The reduction of mean systolic OBP was –23.7 mmHg at six months (n=236) and –27.3 at 12 months (n=90). In contrast, mean systolic ABP was only reduced by 8.7 mmHg at six months (n=236) and by 9.9 mmHg at 12 months (n=90). The rate of responders at six and 12 months, respectively, was 73% and 76% in the OBP (defined as a BP reduction of >10 mmHg), and 65% and 70% in the ABP measurement (defined as a BP reduction of >5 mmHg)20. As the rate of BP responders following RDN with RF in our study group (defined as a systolic BP reduction of ≥10 mmHg in the ABP measurement) was 67% at six months of FU19, the responder rates of both patient groups are not comparable. However, a higher rate of non-responders in ABP in the study of Mahfoud et al could be conceivable had the definition of responder been a BP reduction of ≥10 mmHg. Due to the well-known differences between OBP and ABP, in our present study we assessed the reduction of OBP as well as ABP. We found that the difference in the BP reduction between OBP and ABP was much smaller than in other RDN studies. Our findings are therefore in agreement with the differences between OBP and ABP observed in conventional medical treatment studies. In a recent published meta-analysis the reduction in the ABP was 78% of the reduction in the OBP32.
Limitations
Our study is obviously limited by the small number of patients. Furthermore, we cannot rule out that a second-line RDN procedure with RF instead of cryoablation, as in this study, might also have increased the number of BP responders or that the observed BP reduction might at least partially be a late responder effect to the previously performed RDN with RF.
Conclusions
In spite of these limitations, our tentative conclusion is that the reduction in systolic OBP and ABP observed qualifies RDN with cryoenergy as a second-line therapeutic option in non-responders to RDN with RF. In addition, the use of cryoenergy might reduce the pain during RDN therapy. Consequently, cryoablation for RDN could possibly also be used as a first-line approach. Future randomised studies should clarify whether cryoenergy for second-line RDN is indeed more effective than second-line RDN with RF current. Furthermore, the efficacy of RDN with RF and cryoenergy as a first-line therapy should be compared with RF current.
| Impact on daily practice Further evaluation of the clinical impact of RDN in the treatment of resistant HTN is necessary. The use of cryoablation as an alternative energy source in the treatment of resistant HTN might not only increase the effectiveness of RDN, but also reduce the pain during the procedure. Our tentative findings have to be confirmed in larger multicentre trials. Moreover, the development of a special cryoablation catheter designed for use in the renal artery is desirable. If these preconditions are fulfilled, the use of cryoenergy for RDN as a matter of routine in first-line and second-line procedures is conceivable. |
Acknowledgements
We would like to thank Prof. Dr Rainer K. Silbereisen (University of Jena) for his thorough reading of the manuscript.
Conflict of interest statement
The authors have no conflicts of interest to declare.

