More people in Europe are likely to have died from hypertension-associated cardiovascular disease during the COVID-19 pandemic than from COVID-19 itself12. As we look back at a pandemic that caused so much harm – economic, social, and health-related – readers would be forgiven for not noticing that for decades we have been living through a slow-motion global epidemic of hypertension that shows no signs of abating.
The leading cause of premature death in the world is hypertension, which begs the question “how well are we doing at treating it?” Not very well is the answer. In the United States, control rates have now fallen below 50% again3, and there are few countries doing significantly better. It, therefore, seems unquestionable that, having had more than enough antihypertensive drugs for several decades – the majority of which are inexpensive – and a good understanding of the lifestyle modifications required to mitigate hypertension, new strategies for blood pressure control are urgently required.
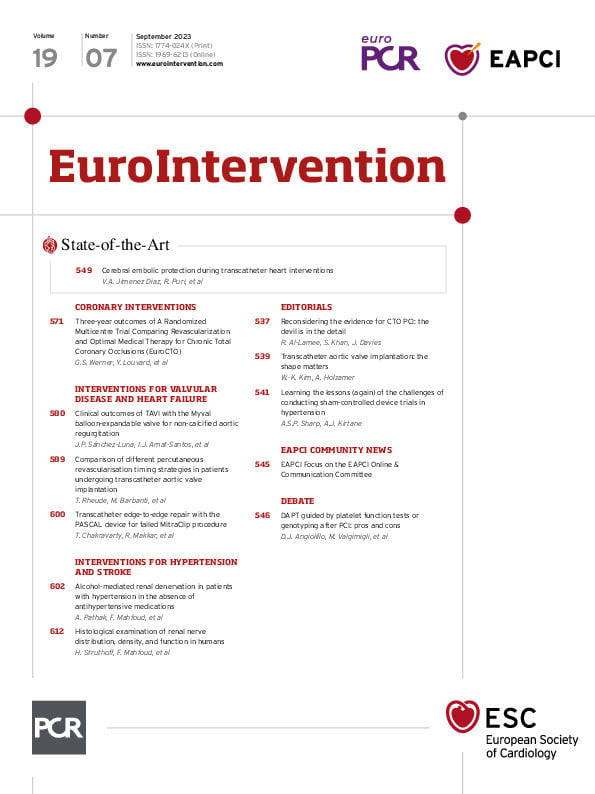
In 2023, in this journal, the European Society of Cardiology’s Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions produced a consensus statement supporting the adjunctive use of device-based therapies to treat hypertension4. This represented a radical change in the philosophy of hypertension treatment. For the first time, an international group of physicians, some of whom specialised in the pharmacological and some of whom had led the research into the interventional treatment of hypertension, came together and agreed that, within robust frameworks for delivery, renal denervation (RDN) treatment using radiofrequency (RF) and ultrasound (uRDN) technologies should now be offered to patients within Europe. This recommendation followed positive results from six, positive, sham-controlled trials using both devices567.
Conducting sham-controlled trials is not easy, and the road for RDN has been a bumpy one. Lessons were learned the hard way early on in the investigation of RDN technologies in the negative SYMPLICITY HTN-3 trial. Post hoc analysis found that (non-protocol mandated) changes in medication burden occurred in more than 1 in 3 patients between their procedure and the primary endpoint, which may have affected the blood pressure (BP) findings observed. Questions were also raised about the comprehensiveness of denervation performed in light of a better understanding of renal nerve anatomy and the need for a greater number of ablations to achieve the desired BP-lowering effect8.
A substantial redesign of the trials in this space was therefore conducted, and second-generation technologies were deployed for subsequent study. Initial trials of potential devices would now be conducted as per the standard for a new antihypertensive drug – patients would be taken off their medications, to avoid any confounding from pill adherence or prescription to prove efficacy (“OFF MED” trials). A second raft of trials would test these devices in the presence of medications – a harder task, given the dynamic drug adherence demonstrated by subjects within hypertension trials. Several trials with RF and uRDN achieved this567, and now a new method for achieving denervation – chemical denervation through the use of alcohol injected into the periadventitial space of the renal arteries – is next in line to be assessed under these conditions.
In the current issue of EuroIntervention, Pathak et al publish the results of the TARGET BP OFF-MED study9. In this trial, 106 patients had medications removed before being randomised to either alcohol-based RDN or sham control. While the trial was exploratory and not a priori powered to demonstrate the efficacy of BP lowering, the sample size compares favourably with the SPYRAL OFF-MED pilot trial, which demonstrated efficacy with a second-generation RF device6.
The first question to answer is whether this is a “positive trial”. Due to multiple measurements (and modes of measurement) of BP, hypertension trials can at times be overwhelming with the amount of data presented, some of which may appear more encouraging than others. In the current case, the trial is clearly neutral for a blood pressure-lowering effect in either ambulatory or office BP, with no difference at the primary endpoint ascertainment at 8 weeks. This timepoint is similar to the primary endpoint for the RADIANCE studies using uRDN57, so whilst a later endpoint could plausibly have shown differing results, it was assessed at a timepoint where RDN therapy has previously demonstrated efficacy.
The manuscript next moves to discuss medication burden, which can of course mask BP differences where differential treatment exists between arms. By definition, the current trial was an “OFF MED” trial, and urine testing showed that the primary endpoint was not affected by medications. However, office BP at 12 months was similar, despite evidence of a greater drug burden in the still-blinded sham group equivalent to 80% of a single defined daily dose of antihypertensive drug, a mechanism of standardising drug burden across classes and between groups. At first, this appears encouraging, until one examines the 12-month ambulatory BP data, typically providing more than 10 times the volume of blood pressure data from any given day of blood pressure assessment in trials such as this. There, we see an ambulatory systolic BP (SBP) difference of 5.3 mmHg between groups at 12 months, with lower achieved BP in the sham group. What would it typically take to narrow that gap back in favour of RDN? Approximately 80% of a defined daily dose of antihypertensive medication. It therefore seems that, whilst the office BP was similar at 12 months on fewer medications, ambulatory blood pressure was, in reality, higher in the RDN arm, perhaps because the patients were on fewer medications.
In light of these results in an “OFF MED” population, is there any hope then for this technology? The answer, in our view, is...perhaps.
An “OFF MED” trial is normally the easier of the two trial designs (OFF MED and ON MED) for demonstrating efficacy, as the influence of medication adherence issues are typically excluded. However, it is fair to ask how many patients actually received effective denervation in this trial. Fifty patients were randomised to RDN, but eight did not receive denervation of accessory arteries and two received unilateral denervation. Data from prior trials suggest reduced/non-efficacy from incomplete denervation. Additionally, we would normally expect a non-response rate to any RDN procedure of around 30%. This therefore means efficacy in this trial was driven by the response of just 28 patients. Given the greater than expected standard deviation of blood pressure measurements observed within patients enrolled during the COVID-19 pandemic, a sample size of 63 patients per arm would have been needed to show a reduction in ambulatory SBP from 147 to 142 mmHg with 80% power and a 5% alpha. Therefore, the possibility exists that the study results were achieved because of a Type II error.
Now that a new catheter for the delivery of alcohol RDN is available – allowing more patients to be fully treated – it is conceivable that an adequately powered trial could ultimately prove successful. Unfortunately, however, the most reliable way of demonstrating that is within a repeat “OFF MED” trial. The pivotal TARGET BP-1 ON MED trial has already completed enrolment, and whether that trial was able to incorporate lessons learned from the current one is unclear. Even if it could, it was conducted in an “ON MED” population, which may now be confounding the results of drug trials10, as well as device trials. Without the benefit of a positive signal in an “OFF MED” trial, this is a challenging scenario for any technology and one that we hope can be overcome for alcohol-based ablation to move forward.
Conflict of interest statement
A. Sharp is a consultant to Medtronic, Boston Scientific, Penumbra, ReCor Medical, and Philips. A. Kirtane reports institutional funding to Columbia University and/or the Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CathWorks, CSI, Philips, ReCor Medical, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, and Shockwave Medical. In addition to research grants, institutional funding includes fees paid to Columbia University and/or the Cardiovascular Research Foundation for consulting and/or speaking engagements in which Dr Kirtane controlled the content. He also receives personal travel/meal expenses from Amgen, Medtronic, Biotronik, Boston Scientific, Abbott Vascular, CathWorks, Edwards Lifesciences, CSI, Novartis, Philips, Abiomed, ReCor Medical, Chiesi, Zoll, Shockwave Medical, and Regeneron.