Hypertension is accompanied by significant adverse cardiovascular outcomes, and intensive blood pressure lowering (<120 mmHg) in patients at risk improves outcomes1. However, although numerous highly effective pharmacological therapies are available to lower blood pressure, control rates remain unacceptably low. A substantial number of patients with hypertension are reluctant or incapable of adhering to lifestyle modification and/or poly pharmacotherapy regimens, especially as the former has a time-delimited impact on blood pressure and the latter requires a lifetime of adherence, which is challenging at best. Non-pharmacological control of blood pressure is appealing, and several interventional approaches have been developed and subsequently clinically investigated2. One of these is catheter-based renal denervation. The method uses radiofrequency energy, alternatively ultrasound or chemical denervation, to disrupt renal nerves within the adventitia of the renal arteries, thereby reducing sympathetic afferent and efferent signalling to and from the kidneys3. The appeal here is that a single intervention might reduce blood pressure permanently or for a long time, removing the need for endless medication compliance.
There is widespread consensus that renal denervation can affect blood pressure in specific settings but there is similarly universal appreciation that the clinical evidence in support of renal denervation in resistant hypertension is mixed4. The interest in renal denervation has dropped significantly following the publication of the SYMPLICITY HTN-3 trial5, in which the primary efficacy endpoint was missed. The randomised, controlled, DENERHTN trial6, however, documented superiority of renal denervation: it did meet its primary efficacy endpoint and showed superiority of renal denervation in combination with optimised pharmacotherapy when compared with pharmacotherapy alone. Research activities have picked up again recently with several randomised, sham-controlled studies currently including patients in Europe, the USA, Australia and Japan to answer a number of important questions in order to establish an evidence base for renal denervation as a treatment option in patients with uncontrolled hypertension. Inadequate patient selection, alterations in compliance with antihypertensive medication, insufficient technical performance of the procedure, and several device features were acknowledged as potential confounders in previous studies7. This leaves us still to question whether renal denervation can be harnessed therapeutically. The urgency of treating hypertension and the lack of full resolution of the unanswered questions gnaw at the clinical community, and investigations and clinical trials continue.
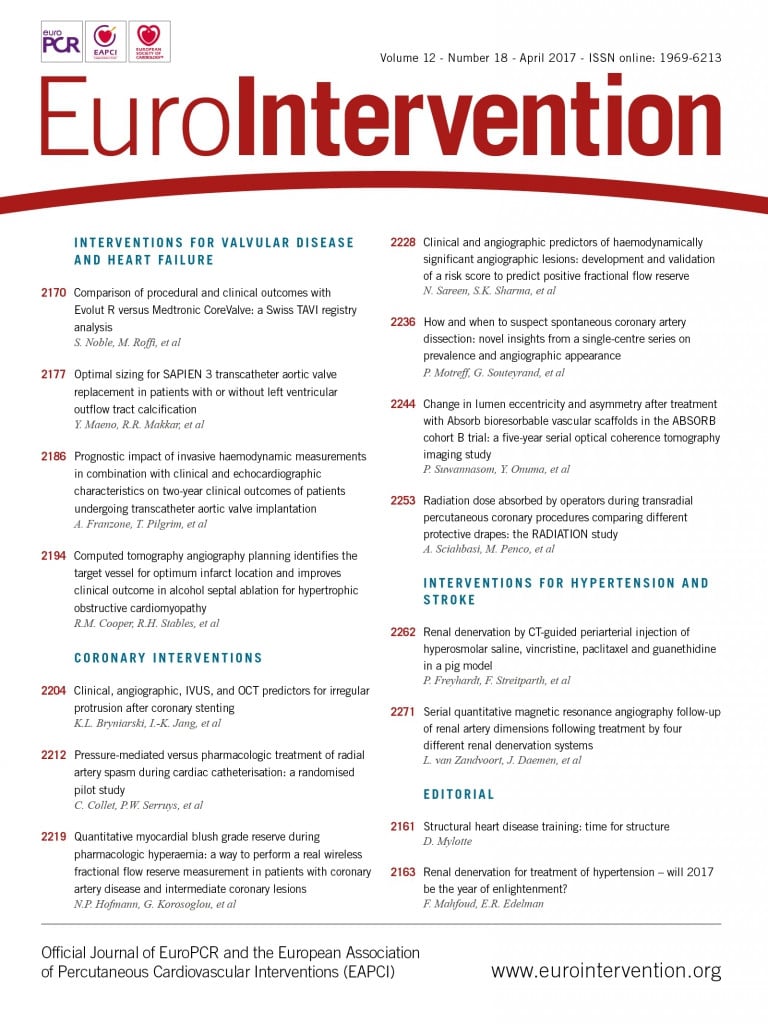
Two interesting papers on renal denervation appear in this issue of EuroIntervention which, when taken in the context of ongoing clinical trials, add to our understanding of the field. van Zandvoort et al8 examined 27 patients with uncontrolled hypertension who underwent catheter-based renal denervation using magnetic resonance angiography (MRA). In this relatively small cohort of patients, there was no decrease in renal artery luminal dimensions at six- and twelve-month follow-up, nor was there any incidence of renal artery stenosis. These data are in line with other observations derived from the ENCOReD registry9, in which MRAs from 96 patients were analysed and new stenosis (25-49% lumen reduction) was seen in only two patients and progression of pre-existing lumen reduction in a single patient after a median time of 366 days post procedure. Similarly, the Global SYMPLICITY Registry10 demonstrated a favourable safety profile in the first ~1,000 real-world patients from around the world.
Freyhardt et al11 asked if a different approach to renal denervation could heighten efficacy without jeopardising safety. They investigated CT-guided periarterial injection of drugs to affect the innervation of renal arteries in place of radiofrequency or ultrasonic energy. Injection of vincristine significantly reduced noradrenaline kidney (NEPI) tissue concentration, a surrogate of sympathetic activity, and histological signs of nerve fibre degeneration. In contrast, hyperosmolar saline, paclitaxel, and guanethidine injections did not impose any relevant alterations. Of note, the reduction in NEPI (–53%) was less marked than has been observed in preclinical studies of catheter-based renal denervation (–70 to –95%)12,13. Periarterial injection of vincristine may in principle represent an alternative, extravascular approach to achieve renal denervation but one might challenge the ease of use, the greater risk of collateral damage and potential complications associated with the CT-guided puncture, especially in obese patients, the higher radiation exposure compared with interventional approaches, and the overall complexity of the procedure. The observation that vincristine was superior to other drugs, however, is relevant and may prompt further investigations, also with the use of endovascular catheters that allow reliable peri-arterial injection of drugs14.
At the same time three major clinical trials will soon be reported.
1. The Symplicity Spyral clinical trial programme15 is studying the use of a multielectrode renal denervation system in patients with uncontrolled hypertension in the absence (SPYRAL HTN OFF-MED; n=100, NCT02439749) and presence (SPYRAL HTN ON-MED; n=100, NCT02439775) of antihypertensive drugs. These trials use the change in systolic blood pressure measured by 24-hour blood pressure from baseline to three months as an efficacy endpoint. The control groups receive sham treatment with renal angiography.
2. The RADIANCE-HTN (NCT02649426) trial compares ultrasonic renal denervation (Paradise® System; ReCor Medical, Palo Alto, CA, USA) to a sham procedure with the primary endpoint change in average daytime ambulatory systolic blood pressure from baseline to two months. Two cohorts are being investigated, namely patients without antihypertensive medication (SOLO, n=146) and patients treated with a fixed-dose triple antihypertensive drug regimen (TRIO, n=146). REQUIRE (NCT02918305, n=140) is designed to evaluate resistant hypertension patients on standard of care medication in Japan and Korea.
3. REDUCE HTN: REINFORCE (NCT02392351, n=100) studies the performance of the bipolar renal denervation system (Vessix™; Boston Scientific, Marlborough, MA, USA) over eight weeks compared to the sham effects of percutaneous renal angiography on mean reduction in daytime ambulatory systolic blood pressure in patients not treated with antihypertensive medication.
Research then continues and sometime soon the results of the ongoing studies will be available to enlighten our understanding of the role of renal denervation as an interventional treatment option for hypertensive patients. The studies will also provide relevant information for the clinical investigation of other emerging technologies such as arteriovenous anastomosis formation, carotid body ablation, carotid bulb expansion, or baroreflex stimulation. Irrespective of the outcomes, the clinical and research community will be educated about the safety and feasibility of invasive sham procedures and their potential impact on biological parameters, such as blood pressure, in hypertensive patients. In the majority of the studies, adherence to antihypertensive medication will be measured meticulously using toxicological analyses, which will provide insights into potential compliance changes while participating in a clinical study investigating a new device-based treatment. Finally, we will understand whether a class effect of different devices can be assumed or whether distinct technologies are associated with distinct outcomes.
Renal denervation is probably facing its final chance to prove its value. 2017 will certainly be an exciting year for catheter-based renal denervation – stay tuned!
Conflict of interest statement
F. Mahfoud is supported by Deutsche Gesellschaft für Kardiologie, and has received speaker honoraria and consultancy fees from Medtronic. E. Edelman has no conflicts of interest to declare.