Abstract
Despite lifestyle modification and pharmacological approaches, the rates of control of blood pressure are still not optimal. Experimental and clinical studies suggest that renal denervation therapy is an effective and safe treatment for patients with therapy-resistant hypertension leading to a reduction in blood pressure and in systemic and renal sympathetic nervous activation, which plays an important role in the development, progression and prognosis of arterial hypertension. Moreover, besides blood pressure reduction, renal denervation improves glucose metabolism, left ventricular hypertrophy and diastolic function in patients with resistant hypertension. Actually, many small clinical studies suggest that renal denervation may also be useful in diseases other than hypertension such as metabolic syndrome, sleep-related breathing disorders, chronic kidney disease and renal failure, chronic heart failure and polycystic ovary syndrome.
A rising interest
According to a PubMed search, the number of papers found by searching for “renal denervation” rose from 52 in 2010 to 192 in 2012, reflecting a growing interest in this new therapeutic strategy.
Current evidence suggests that renal denervation therapy is an effective and safe treatment for patients with therapy-resistant hypertension1. However, bearing in mind the physiopathological involvement of the sympathetic nervous system in many other disease states, novel indications for this promising technique may arise in the near future. Indeed, besides patients with arterial hypertension possible candidates for renal denervation may be patients with sleep apnoea syndrome, chronic heart failure, chronic kidney disease, metabolic syndrome, and polycystic ovary syndrome1.
Management of arterial hypertension
According to the current guidelines, renal nerve ablation is at present exclusively used in patients with treatment-resistant hypertension2. In most of these patients undergoing renal nerve ablation, a reduction or even a normalisation of blood pressure can be observed3,4, while only a few assigned to antihypertensive therapy reached normal blood pressure values3. Based on initial experience with the technique, primarily patients with normal blood pressure values in spite of three or more antihypertensive drugs are considered for renal nerve ablation.
However, the indication for renal nerve ablation in hypertensives may change with the growing use of the technique. Of note, renal sympathetic nerve activity is particularly elevated in younger hypertensives with a more recent onset of high blood pressure5 (Figure 1) and hyperactivity of the sympathetic nervous system seems to precede the development of hypertension in the offspring of hypertensive parents6 (Figure 2). Therefore, from a physiopathological point of view, renal nerve ablation could be particularly effective in this patient population, or even in patients with borderline hypertension.
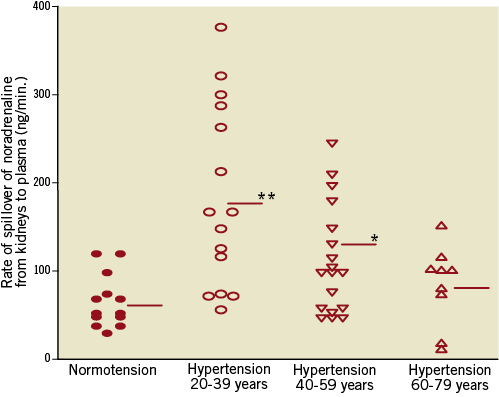
Figure 1. Rate of spillover of noradrenaline in normotensive subjects and patients with hypertension according to age. Reproduced with permission from Esler M.5
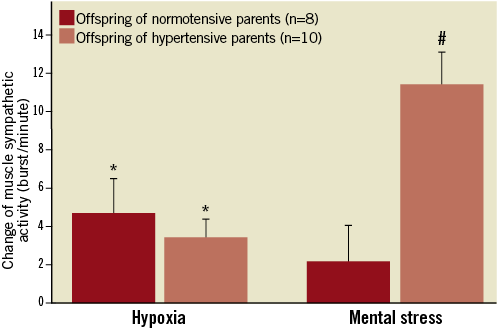
Figure 2. Change in muscle sympathetic activity in the peroneal nerve before and after hypoxia during mental stress in offspring of normotensive and hypertensive parents. Modified from Noll et al6
Recently7 it was shown that, besides its blood pressure lowering effect, renal denervation is associated with a significant reduction of left ventricular hypertrophy and improvement in diastolic function which might have important prognostic implications in patients with resistant hypertension. Unfortunately, although the effects on target organ damage are very promising, one limitation of the currently available evidence is the lack of data about the long-term effect of blood pressure reduction obtained by renal nerve ablation on major cardiovascular events (MACE). Several large randomised trials comparing renal denervation with conventional antihypertensive therapy are therefore in the planning phase (EnligHTN II [NCT 01705080], ReSET2 [NCT 01762488], SYMPLICITY HTN-3 [NCT 01418261], ACHIEVE [NCT 01789918] among others).
Patients with sleep apnoea syndrome
Sleep apnoea syndrome is characterised by abnormal breathing patterns at night and severe intermittent hypoxia. Sleep-related breathing disorders occur in 5-10% of the general population and between 47% and 83% of patients with cardiovascular diseases8. Sleep apnoea increases the risk of cardiovascular events and impairs the control of blood pressure in hypertensives8. Importantly, sleep-disordered breathing is associated with an increased incidence of stroke9,10 and silent cerebral infarction11.
From a pathophysiological point of view this could be related to the activation of the sympathetic nervous system associated to hypoxia6 which causes severe increases in blood pressure. Indeed, nitrogen breathing which induces transient hypoxia leads to marked increases in muscle sympathetic nerve traffic. Patients suffering from sleep-disordered breathing would thus be ideal candidates for renal nerve ablation, which might prevent nocturnal hypertension, might possibly correct the abnormal breathing pattern in sleep and in turn might reduce cerebrovascular events associated with this disorder.
In fact, a preliminary report in 12 patients showed a significant reduction in blood pressure six months after the procedure and, besides that, the polysomnographic studies revealed a clear trend towards reduction of the apnoea/hypopnoea index (Figure 3) and a reduction of the Epworth Sleepiness Scale score in patients treated with renal denervation12. A larger trial is at present ongoing in Poland (NCT 01366625).
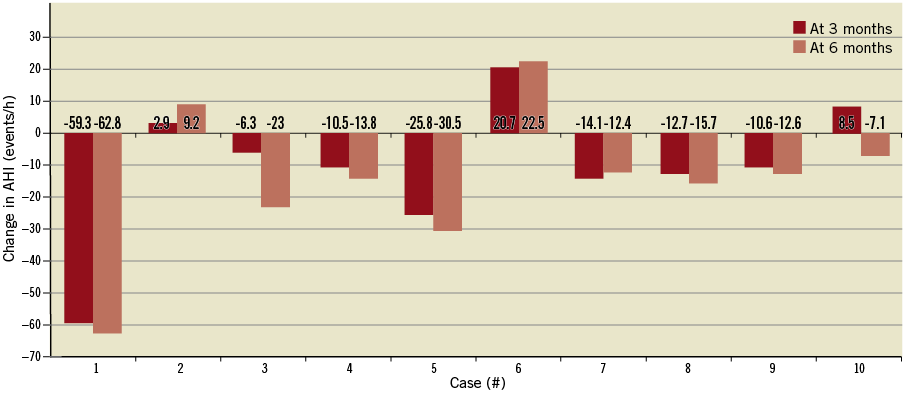
Figure 3. Changes of apnoea/hypopnoea index (AHI) at three and six months after denervation. Data of individual cases12.
Future controlled and randomised studies are required to confirm these preliminary findings and to explore whether renal denervation may also have a beneficial effect on central sleep apnoea.
Patients with chronic heart failure
Another condition where activation of the sympathetic nervous system plays a pivotal role is chronic heart failure. Indeed, activation of the sympathetic nervous system initially aims to compensate for depressed myocardial function in order to preserve cardiovascular homeostasis13. However, prolonged and marked activation has deleterious effects on cardiac structure and performance leading, in a vicious cycle, to progressive worsening of left ventricular function and to the symptoms of heart failure13.
Of note, the degree of activation of the sympathetic nervous system closely correlates with functional class and it is of great prognostic importance14,15. Moreover, drugs able to reduce this activation such as β-blockers improve outcomes in patients with chronic heart failure16. The kidneys and renal sympathetic nervous system are significantly involved in the pathophysiology of chronic heart failure. For example, activation of the renal sympathetic nerves innervating the renal tubules induces excessive retention of sodium17,18, leading to worsening of heart failure. Furthermore, renal sympathetic nerves via activation of β-receptors in juxtaglomerular cells stimulate the release of renin and in turn the formation of angiotensin. Finally, angiotensin II, either directly or via the release of aldosterone from adrenal glands, contributes to water and sodium retention.
Thus, chronic heart failure might represent a suitable condition for the use of renal nerve ablation, although studies are just in the planning phase at this point in time. Before such an indication can be considered, safety concerns need to be addressed, for instance the danger of inducing persistent hypotension1. Interestingly, a preliminary study in a very small group of patients19 showed that renal denervation was safe in this patient population and at six months led to improvements in both symptoms and exercise capacity (Figure 4). Further randomised clinical trials are required to confirm these findings and later to determine the impact of renal denervation on morbidity and mortality in chronic heart failure.
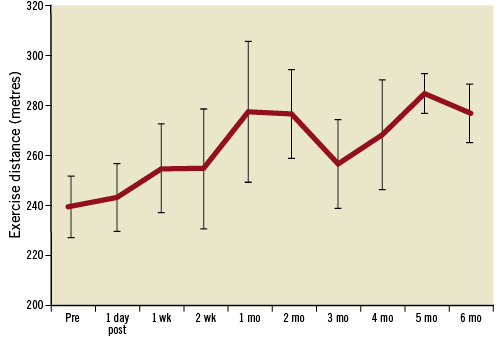
Figure 4. Increase in 6-minute walk test over six months following renal denervation. The 6-minute walk test was performed before denervation, and then at each follow-up visit. Each patient individually had a numerical increase19.
Hypertension associated with obesity and the metabolic syndrome
Impaired glucose tolerance or diabetes mellitus are often associated with arterial hypertension, obesity and dyslipidaemia (the so-called “metabolic syndrome”). Blood pressure control is usually difficult in these patients. Furthermore, in order to reduce cardiovascular risk, antihypertensive therapy should be accompanied by weight reduction, statins and drugs that improve glucose metabolism.
It is of note that obesity, hypertension and insulin resistance appear to have a common pathophysiology. Indeed, hyperinsulinaemia and increased sympathetic tone can lead to sodium retention and hyperaldosteronism20. As such, activation of the sympathetic nervous system appears to contribute to insulin resistance21.
In this context it is of interest that patients with resistant hypertension treated with renal denervation, besides a significant reduction in blood pressure, exhibit an improvement in glucose metabolism (reduction in fasting glucose and C-peptide plasma levels) and insulin resistance (lower insulin plasma levels, improved HOMA index) three months after the procedure. In line with this interpretation, during an oral glucose tolerance test two-hour plasma glucose levels were reduced12,22,23.
Many mechanisms may explain the beneficial effects of renal nerve ablation on glucose metabolism such as: 1) inhibition of central sympathetic tone; 2) better perfusion of skeletal muscle leading to increased glucose uptake; as well as 3) inhibition of the renin-angiotensin system with reduced gluconeogenesis and attenuation of glucagon secretion22. The effects of renal denervation on insulin resistance in patients with metabolic syndrome and elevated fasting glucose are currently being evaluated in the DREAMS (Denervation of the REnal Artery in Metabolic Syndrome; NCT 01465724) study.
Patients with chronic kidney disease
According to current guidelines, patients with GFR less than 45 are not candidates for renal denervation2, despite good reasons suggesting that renal denervation might be useful in patients with chronic kidney disease. Indeed, increased renal sympathetic efferent activity results in a number of intrarenal effects, including activation of the renin-angiotensin-aldosterone system (see above), renal vasoconstriction, sodium retention and inflammation. Moreover, in injured kidneys afferent renal sympathetic activity turns from inhibitory to excitatory24. Sympathetic nervous system hyperactivity is also observed in patients with renal injury, renovascular hypertension, chronic kidney disease and end-stage renal disease1.
Hering and colleagues recently showed that catheter-based renal nerve ablation resulted in a significant reduction in office blood pressure (Figure 5), namely an improvement of 24-hour blood pressure profile without any change in renal function at 12-month follow-up in patients with stage III-IV chronic kidney disease and resistant hypertension25. Moreover, a case report suggests that renal denervation might even be effective and safe in patients on chronic haemodialysis26.
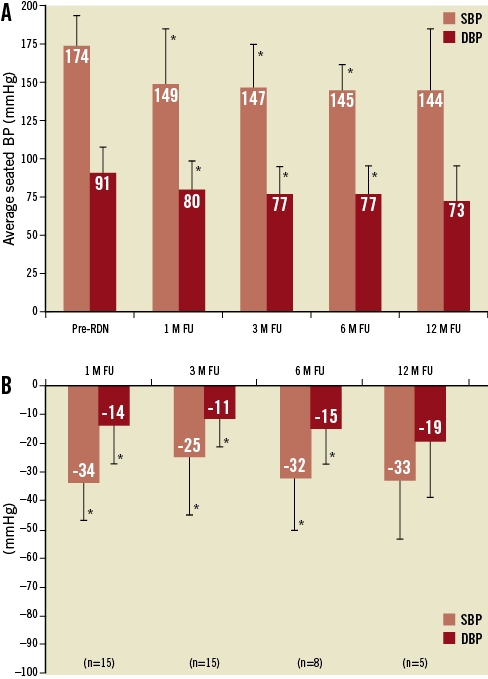
Figure 5. Office BP values at follow-up25. Changes in average office blood pressure (A) and mean decrease in office blood pressure (B) at follow-up. Error bars represent SDs. *p=0.001 versus baseline (before the procedure). FU: follow-up; M: month; pre-RDN: pre-renal denervation
A recently published study in 12 patients with end-stage renal disease and uncontrolled blood pressure showed that renal denervation was feasible in those patients and associated with a sustained reduction in systolic office blood pressure at three, six, and 12 months. In two patients the author showed a reduction of sympathetic nerve activity after renal denervation27.
Moreover, it is of note that renal denervation was found to be able to reduce renal resistive index and incidence of albuminuria without changes in glomerular filtration rate or renal artery structure within six months in patients with resistant hypertension28.
Patients with polycystic ovary syndrome
Polycystic ovary syndrome is a common endocrine disorder characterised by oligo/anovulation, hyperandrogenism and altered ovarian morphology. In women, polycystic ovary syndrome represents an unrecognised cardiovascular risk factor affecting 6-10% of all females of reproductive age1. The syndrome is associated with obesity, ovarian dysfunction and hypothalamic pituitary abnormalities. These abnormalities lead to typical clinical features including obesity, hirsutism, infertility, insulin resistance, hypertension and increased sympathetic nervous activity29,30.
In a preliminary study two obese patients with hypertension and polycystic ovary syndrome were treated by renal nerve ablation31. Three months after renal denervation a mild-to-moderate reduction in blood pressure was observed in both patients. This reduction in blood pressure was paralleled by a reduction in sympathetic nervous activity as measured by microneurography in the peroneal nerve and whole body norepinephrine spillover. Moreover, fasting plasma glucose levels were reduced and insulin sensitivity increased31. Obviously, these promising but preliminary results need to be confirmed in the longer term by randomised controlled studies.
Conclusions
Resistant hypertension is still an unresolved issue. Therefore, the development of new technologies and drugs able to optimise blood pressure control in such patients is highly welcome. The role of sympathetic nervous system activity in the pathophysiology of arterial hypertension is crucial and therefore reduction of sympathetic nerve activity is one of the main targets while searching for new therapeutic options for resistant hypertension.
Clinical trials have confirmed that catheter-based percutaneous renal nerve ablation is safe and effective in reducing blood pressure, improving glucose metabolism, left ventricular hypertrophy and diastolic function in resistant hypertension. Whether these results can be expanded to mild-to-moderate hypertension or may even allow us to prevent essential hypertension from occurring is a vision, which has come closer to reality but needs confirmation in well controlled trials.
Beyond hypertension, renal nerve ablation might have a role in other conditions associated with increased sympathetic nerve activity. Indeed, small trials suggest that the role of this new technique may not be limited to hypertension, but might also be useful in chronic heart failure, chronic kidney disease and renal failure, polycystic ovary syndrome, sleep-related breathing disorders, obesity and metabolic syndrome. Future studies will have to explore these exciting possibilities and confirm the usefulness of renal nerve ablation beyond hypertension in vigorous controlled trials.
Funding
This research was supported by grants from Medtronic and St. Jude Medical Europe.
Conflict of interest statement
T. F. Luscher received honoraria for advisory boards and lectures from St. Jude Medical and Medtronic. The other authors have no conflicts of interest to declare.