Abstract
Catheter-based renal denervation (RDN) leads to a considerable decrease of blood pressure in the vast majority of patients with resistant hypertension. However, only minor or no blood pressure change is achieved in some patients. This non-reponse is defined as a reduction of office systolic blood pressure of less than 10 mmHg following RDN. The rates of non-response vary between 8-37%. Here several causes are discussed such as inappropriate patient selection, an ineffective procedure, the subordinate contribution of sympathetic activation for the maintenance of hypertension, and patient conditions such as non-adherence to drug therapy. Based on current evidence, an ideal candidate for RDN has high baseline blood pressure, which is known to be the best predictor for blood pressure reduction after RDN. In order to ensure treatment success further criteria have to be fulfilled, such as exclusion of secondary hypertension and optimised medical therapy.
Introduction
Catheter-based renal denervation (RDN) has been shown to reduce sympathetic nerve activity and blood pressure in patients with resistant hypertension1-3. The published trials have reported a considerable decrease of blood pressure after RDN in patients with a mean baseline blood pressure of 180/110 mmHg despite an average intake of more than four antihypertensive drugs. However, blood pressure response after RDN varies and in 8-37% only minor or no blood pressure changes are achieved (non-response). In daily clinical practice, it is challenging for physicians to select appropriate patients for RDN in order to minimise treatment failure. This review highlights the prevalence and possible causes of non-response to RDN and current knowledge on the ideal candidate for RDN.
Non-responders
In immunology and oncology non-response is defined as the failure of a specific treatment. In cardiology, it is used for patients who fail to show clinical or echocardiographic improvement after receiving a cardiac resynchronisation device4. In hypertension, the definition of non-response was introduced for the first time in the Symplicity HTN-1 trial5. Arbitrarily, it has been defined as a reduction of office systolic blood pressure (SBP) of less than 10 mmHg after six months following RDN. In previously published studies, the rates of non-response after RDN ranged between 8-17%1,2,6. However, the rate of non-responders in the crossover group of Symplicity HTN-2 was 37.1%7. The causes of non-response are not completely understood but here we will discuss several hypotheses (Figure 1).
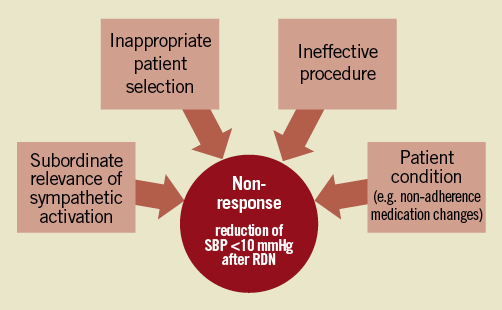
Figure 1. Possible causes of non-response to renal denervation. RDN: renal denervation; SBP: systolic blood pressure
INAPPROPRIATE PATIENT SELECTION
The selection of appropriate patients is key to ensuring successful treatment. At the present time, only patients with resistant hypertension after exclusion of pseudo-resistance and reversible or secondary cause are considered for RDN9,10. The presence of secondary hypertension may be a cause for non-response. For instance, patients with primary aldosteronism, a common finding in patients with uncontrolled hypertension, will probably not perceive a significant change of blood pressure after RDN, but it is more likely to respond to an aldosterone antagonist9. Additionally it has become clear, that the degree of blood pressure reduction depends on the baseline blood pressure. Recent data has suggested that the higher the blood pressure is at baseline, the greater the reduction of blood pressure after RDN will be (Figure 2)10. Consequently, baseline blood pressure was identified in several populations as a predictor of a greater blood pressure reduction after RDN1,2. However, these observations may partly be explained by the statistical phenomenon of “regression to the mean”11. A small study reported that in patients with a milder form of resistant hypertension (SBP 140-160 mmHg), the blood pressure lowering effect of RDN was less pronounced compared to the Symplicity trials12. Advancing the indications for RDN to milder forms of hypertension, a smaller magnitude of blood pressure reduction will be associated with the procedure. The current definition of non-response may then not be appropriate and additional surrogate parameters, such as heart rate, might be needed. Indeed it is well documented, that even modest blood pressure reductions are accompanied by significant improvements of cardiovascular morbidity and mortality13.
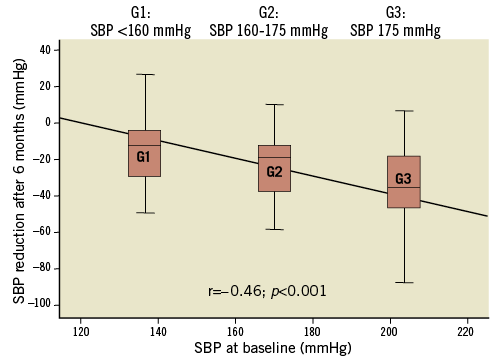
Figure 2. Systolic blood pressure (SBP) at baseline correlates with reduction of blood pressure after renal denervation. Patients with resistant hypertension (n=88) were grouped according to the tertiles of SBP at baseline (Group 1: SBP<160; Group 2: 160-175; Group 3 >175 mmHg) showing this association. SBP: systolic blood pressure
INEFFECTIVE RENAL DENERVATION PROCEDURE
Different renal denervation systems are already available or will soon be released14. These devices differ amongst others concerning the delivered energy, the number of electrodes, and the duration of ablation. However, a major unresolved issue is how to monitor treatment success intraprocedurally and this issue has not been answered by any currently available device. Blood pressure changes rarely occur directly after the procedure but rather take weeks to months. The captured procedural parameters, such as numbers of ablations, temperature, power, and impedances, vary depending on the device used. Data showing an association between procedural parameters and later response are lacking. For the time being, treating physicians have to accept a black box during the procedure, as no procedural parameters of treatment success are available. This fact underlines the importance of a close cooperation between the interventionalist and the referring hypertension expert in order to get feedback on the success of RDN during follow-up.
SUBORDINATE RELEVANCE OF SYMPATHETIC ACTIVATION
The exact mechanism of blood pressure reduction by RDN is not yet fully understood. A reduction of local and central sympathetic activity may exhibit beneficial effects as a reduction in total peripheral resistance, reduced renin release, and changes in water and sodium handling15,16. Although sympathetic activation plays a pivotal role, the pathophysiology of hypertension is multifactorial18. Therefore, it may be speculated that some cases of non-response are related to a non-significant contribution of the sympathetic nervous system to the expression of hypertension. In favour of this hypothesis, a substantial number of non-responding patients have a reduction of heart rate, another effect of RDN, which has recently been described6,18. Based on these findings, it may be speculated that in some non-responding patients sympathetic activity is reduced by RDN, observed for instance by a reduction of heart rate indicating a sufficient procedure. Other pleiotropic effects of RDN, such as changes in glucose metabolism19, reduction in the severity of obstructive sleep apnoea20, and improvement of ventricular mass and diastolic function21, need further investigation concerning their association with RDN-dependent blood pressure changes.
PATIENT CONDITION
Due to the high blood pressure values and the burden of antihypertensive medication, quality of life in patients with resistant hypertension is often impaired22. Additionally, the media, such as newspapers and television, create expectations in patients referred for RDN treatment. Serious misinformation among patients and referring doctors exists and there is a belief that the procedure is a cure for hypertension. As mentioned above, successful treatment can only be estimated after RDN with surrogates such as blood pressure. Therefore, it is mandatory that patients stay on the same drug regime for a certain period of time after the procedure, e.g., three to six months. Nevertheless, changes of medications or non-adherence can often be found in daily clinical practice. This may lead to the misconception of an unsuccessful treatment. Dealing with patient’s and physician’s expectations, explaining the course of blood pressure changes, and underlining the importance of medical adherence are key steps for a successful treatment and a satisfied patient and physician.
Characteristics of the ideal candidate for renal denervation
The ideal candidate for RDN may be summarised as a patient having severely elevated blood pressure in office and home measurement despite optimised medical therapy, with optimal renal anatomy, in whom RDN can be performed safely, and finally who shows a large drop in blood pressure and displays other pleiotropic effects.
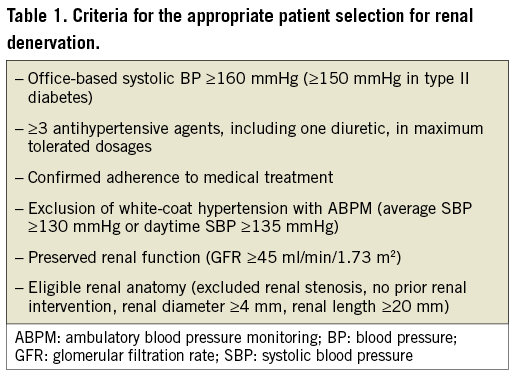
In daily clinical practice, patient selection is based on the available evidence, summarised in Table 18,9. Eligible patients fulfil the criteria of treatment resistant hypertension, defined as office systolic blood pressure ≥160 mmHg (≥150 mmHg in type II diabetics) despite treatment with at least three antihypertensive agents including one diuretic, all taken in maximum or maximum tolerated dosages. Elevated office blood pressure should be confirmed by ambulatory blood pressure measurement to exclude pseudo-resistance. A key step in the evaluation process should be exclusion of secondary causes of hypertension, in particular primary hyperaldosteronism, renal artery stenosis, OSA, pheochromocytoma, and hyperthyroidism. Although evidence on the safety and efficacy of RDN in a small number of patients with mild to moderate chronic kidney disease exists, kidney function should be preserved, defined as a glomerular filtration rate ≥45 ml/min/1.73 m2.23 Finally, the renal anatomy should meet the eligibility criteria to allow a safe and effective procedure: ≥4 mm in diameter and ≥20 mm in length with absence of significant renal artery stenosis (>50%) or prior intervention (balloon angioplasty or stenting).
Conclusion and perspective
The current knowledge indicates that RDN is an effective and safe treatment option if used in well-selected patients. Patients with a high treatment success are those with true resistant hypertension and a markedly elevated blood pressure. Treating physicians also have to face the problem of non-response. Several hypotheses on the causes of non-response exist and the truth is probably a composite of all of these. Substantial research is needed to enhance the understanding of non-response and to identify potential predictors of response.
Funding
C. Ukena, F. Mahfoud and M. Böhm are supported by the Ministry of Science and Economy of the Saarland. M. Böhm is supported by the Deutsche Forschungsgemeinschaft (KFO 196). F. Mahfoud is supported by Deutsche Hochdruckliga und Deutsche Gesellschaft für Kardiologie.
Conflict of interest statement
C. Ukena, B. Cremers, M. Böhm and F. Mahfoud received speakers’ honoraria from Medtronic Ardian. S. Ewen has no conflicts of interest to declare.

