Abstract
Aims: Recent studies have reported a considerable number of non-responders after renal sympathetic denervation (RSD) with radiofrequency technology. Here we report our results of repeat RSD using ultrasound in these patients.
Methods and results: A cohort study was performed in patients who underwent ultrasound RSD after non-response to RSD with radiofrequency. Non-response was defined as mean daytime systolic blood pressure ≥140 mmHg and/or a reduction of ≤10 mmHg in ambulatory blood pressure measurement (ABPM) ≥6 months after radiofrequency denervation. ABPM was recorded at baseline, post radiofrequency RSD as well as at three and six months post ultrasound RSD. A total of 24 non-responders underwent retreatment with the ultrasound device at a mean 15.3±8.2 months after radiofrequency RSD. Ultrasound RSD was performed successfully in all patients without severe adverse events. Mean daytime systolic blood pressure changed from 161.7±14.6 mmHg at baseline to 158.5±9.5 mmHg post radiofrequency RSD and to 150.5±10.4 mmHg and 151.6±11.0 mmHg at three and six months, respectively, post ultrasound RSD (p<0.01 with repeated measures analysis of variance). The main results of post hoc testing were as follows: baseline versus post radiofrequency RSD, p=0.83; baseline versus three months post ultrasound RSD, p=0.01; and baseline versus six months post ultrasound RSD, p=0.04.
Conclusions: Ultrasound RSD appears to be safe and an effective therapeutic approach in patients not responding to previous RSD with radiofrequency technology.
Abbreviations
ABPM: ambulatory blood pressure measurement
ANOVA: analysis of variance
BP: blood pressure
RSD: renal sympathetic denervation
Introduction
Therapy-resistant arterial hypertension affects a considerable number of hypertensive patients and represents a major risk factor for future cardiovascular events1,2. Renal sympathetic denervation (RSD) has been introduced as a promising therapeutic approach in these patients3,4. However, recent studies have reported inconsistent results regarding effectiveness, with a significant number of non-responding patients across several trials5-8. Even overall positive trials exhibited non-response in up to 30% of patients4,7. Insufficient operator experience, patient characteristics and selection as well as changing antihypertensive drug treatment have been discussed as potential explanations for the disappointing results of the largest, randomised trial to date (SYMPLICITY HTN-3), which failed to show a significant reduction in systolic blood pressure (BP) after RSD compared to a sham procedure5,9. Furthermore, technical limitations of the first-generation radiofrequency ablation catheter, which has been used in most large clinical trials, could have contributed to a lower success rate. Circumferential denervation, which should be aimed for, requires continuous repositioning of the device and is therefore difficult to assure and is highly dependent on operator experience. These issues have been addressed by developing second-generation radiofrequency devices10-14. Moreover, alternative approaches to catheter-based energy delivery (ultrasound, cryoenergy) might enhance success rates and represent a therapeutic option for patients not responding to radiofrequency RSD with first-generation catheters15-18. Currently, data regarding the optimal management of patients with an inadequate drop in BP after RSD are sparse and general treatment recommendations are missing. Successful repeat denervation with a second-generation radiofrequency device has been described in a single case report19. Moreover, a small study demonstrated the effectiveness of RSD with cryoenergy as a second-line approach in ten non-responders to radiofrequency RSD18. Utilising endovascular ultrasound might provide a substantial benefit in these patients since it enables circumferential energy delivery in a more reliable fashion with adequate tissue penetration16,17. However, redo with ultrasound has not been investigated. Hence, the aim of the present study was to evaluate retrospectively the efficacy and safety of RSD with ultrasound as a second-line treatment strategy in patients who previously underwent radiofrequency RSD with an inadequate drop in BP.
Methods
STUDY DESIGN AND PATIENT POPULATION
This retrospective study was conducted at the University of Leipzig–Heart Center and included 24 patients with resistant hypertension who underwent RSD using ultrasound between October 2013 and April 2015 after non-response to previous radiofrequency RSD. Resistant hypertension was defined as mean daytime systolic BP ≥140 mmHg in 24-hour ambulatory BP measurement (ABPM) despite the intake of ≥3 antihypertensive agents of different classes, including a diuretic. Secondary causes of hypertension were excluded and all patients had a suitable anatomy for RSD and an estimated glomerular filtration rate >45 ml/min/1.73 m2 (Modification of Diet in Renal Disease formula). Non-response to radiofrequency RSD was diagnosed in patients who fulfilled at least one of the following criteria in 24-hour ABPM ≥6 months after the procedure: 1) the reduction in mean daytime systolic BP was ≤10 mmHg; and/or 2) the definition of resistant hypertension as stated above was still applicable.
Patients were recruited from the computerised medical records including all renal denervation procedures performed at the institution. The study protocol complied with the Declaration of Helsinki and was approved by the local ethics committee.
CLINICAL EVALUATION AND INTERVENTIONS
Baseline evaluation of patients included medical history, review of medication, clinical examination, laboratory testing and 24-hour ABPM with a validated oscillometric device (Spacelabs model 90207; Spacelabs Healthcare GmbH, Feucht, Germany). BP was measured at 30-minute intervals and patients were encouraged to keep to their normal daily activity. Separate analyses were performed for the daytime (between 7:00 am and 10:00 pm) and for the night-time period (between 10:00 pm and 7:00 am) with a dedicated software (CardioNavigator Version 2.4.13; Del Mar Reynolds Medical, Hertford, United Kingdom).
After obtaining written informed consent, radiofrequency RSD was performed as described previously3,6. The Symplicity Flex™ renal denervation catheter (Medtronic, Minneapolis, MN, USA) was used to deliver four to six ablation runs of two minutes circumferentially to each renal artery wall according to the standardised protocol with controlled temperature, impedance and power output. Procedural success was evaluated via ABPM regularly during follow-up and demonstrated non-response ≥6 months after the first intervention. All patients agreed to a second RSD procedure with an ultrasound-based system (PARADISE® percutaneous renal denervation system; ReCor Medical Inc., Palo Alto, CA, USA). Interventions were performed under fluoroscopic guidance at one to three locations within each renal artery starting from distal as reported previously15. Ultrasound energy was delivered for 10 seconds after positioning the transducer in the centre of the renal artery by inflating the surrounding balloon. Energy delivery was accompanied with cooling via the inflation balloon. Remifentanyl was administered intravenously to control visceral pain during both interventions. All procedures were performed by two operators with vast experience in the field of RSD. The maximum diameter of both renal arteries in the area of RSD was systematically assessed in all patients.
FOLLOW-UP AND ENDPOINTS
Patients underwent outpatient follow-up including ABPM at regular intervals after the first intervention as well as immediately before, and at three and six months after RSD with ultrasound. The primary efficacy analysis assessed the change in 24-hour daytime systolic BP after RSD with the ultrasound system. Secondary analysis included other BP parameters as well as procedural characteristics and safety.
Statistical analysis
Categorical variables are expressed as number and percentage of patients and compared with the Fisher’s exact test. Continuous data are presented as mean±standard deviation as well as 95% confidence intervals when appropriate and compared with the independent samples t-test. ABPM values were compared between baseline, post radiofrequency RSD (corresponding to the final measurement before retreatment), as well as at three and six months after RSD with ultrasound using repeated measures analysis of variance (ANOVA). Post hoc comparisons of significant values were performed with the Scheffé correction algorithm.
A two-tailed p-value <0.05 was considered statistically significant. All statistical analyses were performed with SPSS, Version 17.0 (SPSS Inc., Chicago, IL, USA).
Results
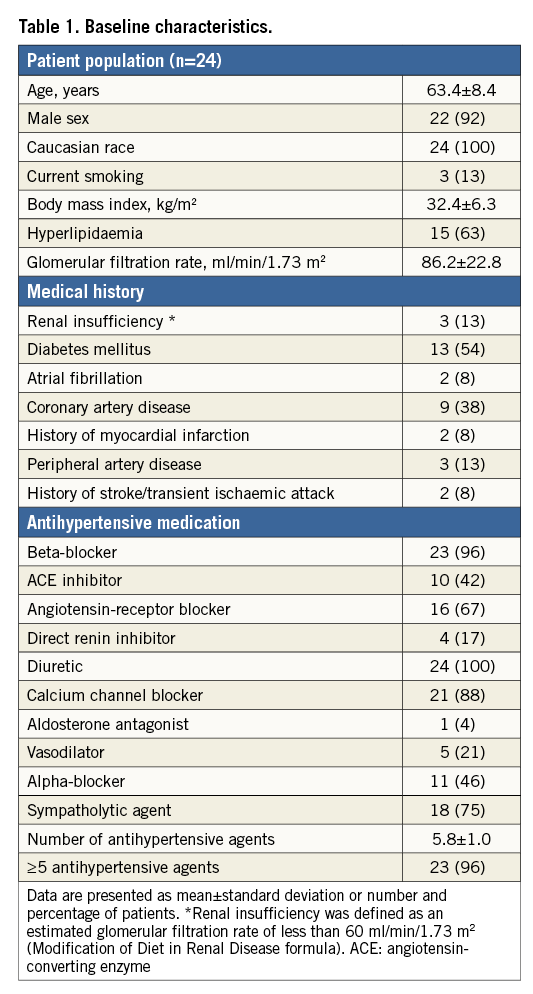
The baseline characteristics of the 24 patients with resistant hypertension included in this study are illustrated in Table 1. The patient population consisted of predominantly male patients with a mean age of 63 years and moderate cardiovascular risk profile. Patients were receiving an average of nearly six antihypertensive medications, and about three of these medications were at the maximally tolerated dose. Radiofrequency RSD did not result in a significant BP drop (Table 2), and all patients fulfilled the predefined criteria for non-response (mean daytime systolic BP ≥140 mmHg in all patients, drop ≤10 mmHg in 17 patients). Retreatment with ultrasound RSD was performed at a mean 15.3±8.2 months after the first intervention. The types and dosages of antihypertensive medications remained unchanged in 16 patients (67%) after radiofrequency RSD. Three and six months after ultrasound denervation, adherence to the medical treatment before the redo procedure was observed in 19 patients (79%) and 17 patients (71%), respectively.
PROCEDURAL CHARACTERISTICS AND SAFETY
Administration of contrast agent (94.8±49.8 ml versus 67.1±35.0 ml; p=0.04) as well as the duration of the procedure (85.3±35.2 minutes versus 59.3±21.1 minutes, p<0.01) were significantly increased during radiofrequency ablation as compared to ultrasound denervations, whereas the fluoroscopy times were similar (Table 3). The mean maximum vessel diameter in the area of RSD was 6.8±1.3 mm for the left renal artery and 6.5±1.0 mm for the right renal artery. Overall, 44 of the 48 renal arteries (91.7%) measured ≥5.5 mm and all patients exhibited at least one renal artery ≥5.5 mm.
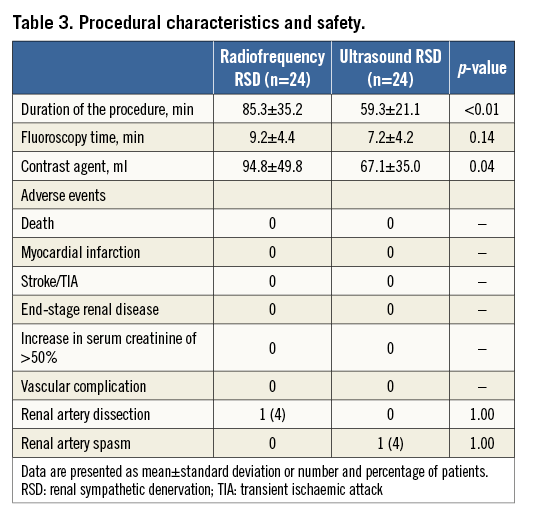
Adverse events during and after the RSD procedures are illustrated in Table 3. There were no deaths, neurological complications, alterations in kidney function or other severe events. Renal artery stenting had to be performed in one patient due to a small dissection caused by the guiding catheter during the initial procedure using radiofrequency. During redo procedures, one patient experienced severe renal artery spasm following denervation using ultrasound, which had resolved completely on follow-up renal angiography three days later (Figure 1).
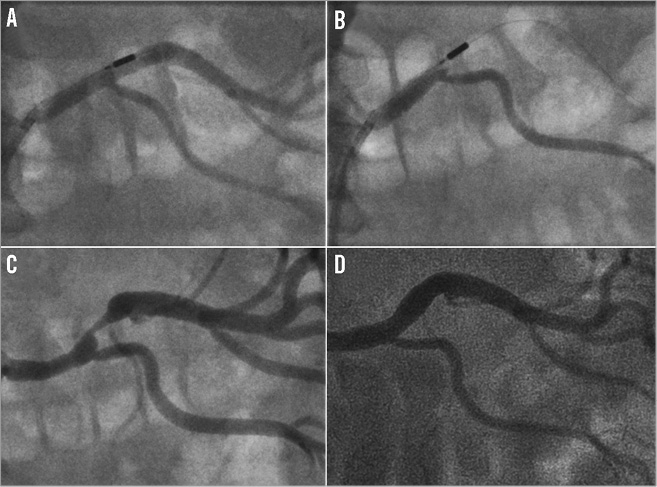
Figure 1. Spasm of the left renal artery after renal sympathetic denervation with ultrasound. A) Ultrasound-based PARADISE RSD catheter within the left renal artery of a male patient with resistant hypertension. B) Balloon inflation and verification of stopped blood flow by contrast injection. C) Acute severe spasm of the superior branch of the left renal artery. D) Complete reversibility of renal artery spasm three days after RSD therapy.
RESULTS OF AMBULATORY BLOOD PRESSURE MEASUREMENT
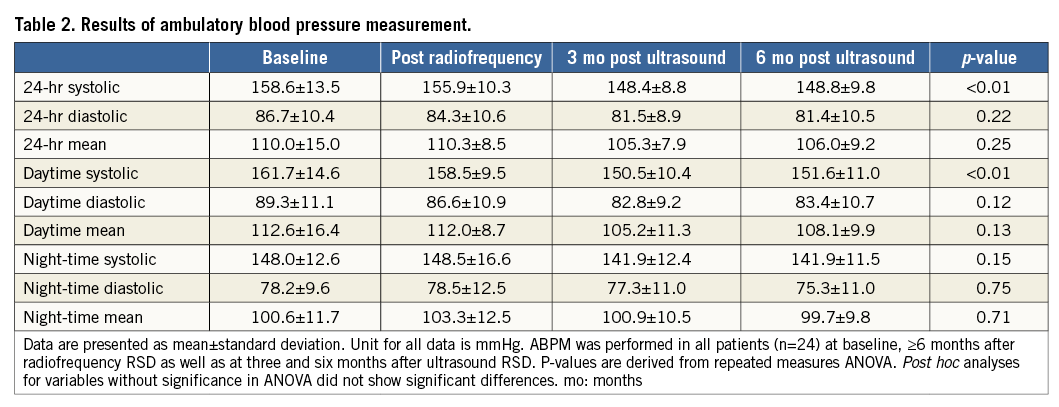
The results of ABPM at baseline, after RSD with radiofrequency as well as at three and six months after RSD with ultrasound are shown in Table 2. Mean daytime systolic BP changed from 161.7±14.6 mmHg at baseline to 158.5±9.5 mmHg post radiofrequency RSD and to 150.5±10.4 mmHg and 151.6±11.0 mmHg post ultrasound RSD (p<0.01 with repeated measures ANOVA). Post hoc analyses demonstrated a significant change from baseline to three months (p=0.01) and six months (p=0.04) post ultrasound RSD (Figure 2A). Changes from baseline to post radiofrequency RSD (p=0.83), post radiofrequency to three months (p=0.13) and six months (p=0.18) post ultrasound RSD as well as between three and six months post ultrasound RSD (p=0.99) were not significantly different. Mean 24-hour systolic BP was 158.6±13.5 mmHg at baseline and changed to 155.9±10.3 mmHg, 148.4±8.8 mmHg and 148±9.8 mmHg, respectively (p<0.01 with repeated measures ANOVA). The results of post hoc testing were as follows: baseline versus post radiofrequency RSD, p=0.87; baseline versus three months post ultrasound RSD (p=0.02); baseline versus six months post ultrasound RSD (p=0.03); post radiofrequency RSD versus three months post ultrasound RSD, p=0.13; post radiofrequency versus six months post ultrasound RSD (p=0.18); and three months versus six months post ultrasound RSD (p=1.00) (Figure 2B). Diastolic and mean BP as well as night-time values did not change significantly (Table 2).
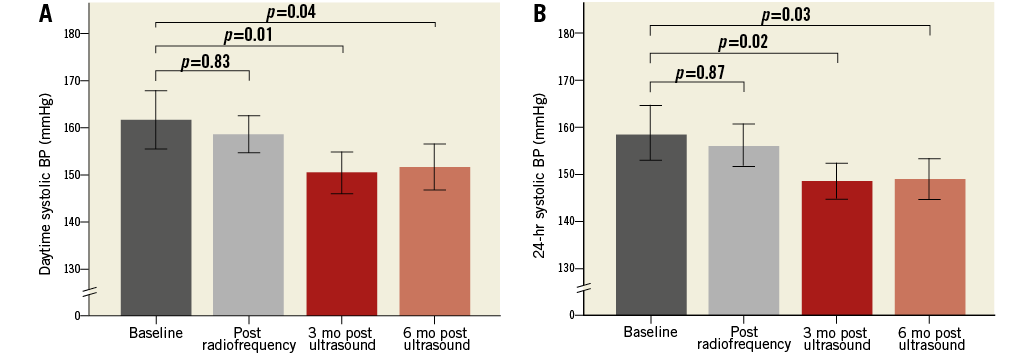
Figure 2. Mean daytime and 24-hour systolic blood pressure. The mean values for daytime systolic (A) and 24-hour systolic (B) BP in ABPM at baseline, post radiofrequency RSD as well as at three and six months post ultrasound RSD. Error bars display 95% confidence intervals. P-values are derived from post hoc comparison. BP: blood pressure; mo: months
Discussion
This study represents the first report of the ultrasound-based PARADISE RSD system in patients not responding to RSD with radiofrequency. Furthermore, to the best of our knowledge, it is the largest cohort of patients with resistant hypertension undergoing RSD with ultrasound in the current literature. The main findings are: 1) RSD with an ultrasound-based system leads to a significant reduction of BP values in non-responders to radiofrequency RSD and may represent a therapeutic approach in these patients; and 2) ultrasound RSD seems to be a safe procedure.
Irrespective of the results from the SYMPLICITY HTN-3 trial which have offset the initial enthusiasm about RSD as a therapeutic option for patients with resistant hypertension, an inadequate drop in BP has been reported in a substantial number of patients across several clinical trials4,5,7,8. Therefore, the debate about the merits of RSD for resistant hypertension should go beyond the potential limitations in this one particular trial and generate concepts to improve procedural success rates. Technical advances in RSD systems might provide a promising approach. A single-tip radiofrequency catheter (Symplicity Flex) has been used in most clinical trials that have been published to date3-8. Although RSD is a rather simple procedure, radiofrequency ablation especially with this first-generation device has some technical issues which have to be considered. Recent investigations have demonstrated a circumferential distribution of sympathetic nerves in the arterial wall and therefore suggest that effective RSD would need to be circumferential20,21. With the first-generation radiofrequency catheter, this can only be achieved by continuous repositioning of the device and delivering several ablation points one after another. This leads to a considerable duration of the procedure which can be prolonged by catheter instability and patient discomfort due to visceral pain. Furthermore, the radiofrequency technology requires adequate electrode tissue contact to produce sufficient lesions. Maintaining contact between the catheter and the arterial wall can be difficult, and high variations in electrical impedance are the only indirect sign for correct catheter positioning during the intervention. Hence, second-generation radiofrequency devices with multiple electrodes have been developed to address these aspects. The Symplicity Spyral™ catheter (Medtronic), the basket-based EnligHTN™ system (St. Jude Medical, St. Paul, MN, USA) and the balloon-based bipolar Vessix™ system (Boston Scientific, Marlborough, MA, USA) have all demonstrated safety and efficacy in first non-randomised studies10-14. They deliver multiple lesions in a predetermined fashion, thus facilitating circumferential ablation and reducing the duration of the procedure. Furthermore, the basket- or balloon-based systems are thought to ensure stable wall contact.
However, apart from these considerations, concerns have been raised regarding adequate penetration depth with radiofrequency ablation catheters. In a phantom model, the mean lesion depth after RSD with first- and second-generation radiofrequency devices was found to be <4 mm22. In contrast, several studies suggest that a substantial number of renal nerves are located beyond 4 mm of the luminal surface, which might provide an explanation for insufficient response to radiofrequency RSD in some patients16,20. The ultrasound-based PARADISE RSD system might overcome this and other drawbacks of the radiofrequency technique. Since ultrasound does not require direct tissue contact, the transducer can be stabilised in the centre of the renal artery by inflating a surrounding balloon with cooled fluid. This enables controlled, circumferential energy delivery to the sympathetic nerves in the adventitia while minimising arterial wall damage by cooling the surface16,17. Reduction of procedure duration and complete denervation in a more reliable fashion are hypothesised. Moreover, greater ablation distances from the arterial lumen compared to radiofrequency catheters have been reported16,17. At the same time, penetration depth remains highly controllable by varying the power and duration of ultrasound energy delivery to avoid damage to retroperitoneal organs16,17. First clinical experience with the PARADISE technology in 11 patients with resistant hypertension suggests that the procedure is safe and effective regarding BP reduction15. Our analysis in more than twice as many patients not responding to radiofrequency RSD could confirm these preliminary data.
Furthermore, the duration of the procedure and exposure to contrast agent were indeed significantly reduced. However, BP reduction was statistically significant between baseline and post ultrasound RSD but not between post radiofrequency RSD and post ultrasound RSD in post hoc analyses. Moreover, a considerable number of patients still fulfilled the criteria for non-response after retreatment. Therefore, a clinical benefit with the new devices remains to be proven in randomised trials before a routine use can be recommended. These studies should include patients with resistant hypertension who did not respond to RSD with the first-generation radiofrequency device. Treatment recommendations for this not negligible number of patients are missing in view of the lack of research data. Overall, interventional therapeutic options are sparse and basically limited to repeat RSD. However, the timing of assessing the procedural success is important since there are no convenient methods to determine the effectiveness of the denervation immediately. It is well known that RSD does not lead to an instant BP reduction after the intervention and delayed response has been reported23. Therefore, final evaluation (preferably with ABPM) should be performed several months after the procedure under stable drug therapy. In our analysis, retreatment was not performed until six months after the first RSD (mean time between the procedures: 15.3 months). Furthermore, we should keep in mind that the aetiology of resistant hypertension is multifactorial even though the role of sympathetic overdrive seems to be crucial24. Hence, RSD might not be effective in every patient, and recent research efforts have been directed towards identifying patients who are likely to respond. Several biomarkers, impaired baroreflex sensitivity and a lower degree of arterial stiffness have been determined as predictive factors for procedural success but need further validation25-27. If repeat RSD is finally considered as the appropriate approach, the question of the ideal device arises. Current literature provides evidence from only small, non-randomised studies. The EnligHTN system has been used successfully in a single reported case19. Besides, cryoablation, which is established for the treatment of cardiac arrhythmias, has proven to be safe and effective in a series of patients not responding to radiofrequency RSD18. In addition, our study suggests that retreatment with the ultrasound-based PARADISE system represents an effective second-line approach. Of note, the population of non-responders to radiofrequency RSD in our analysis exhibited comparatively large renal arteries with a mean diameter ≥6 mm. A recent post mortem study reported that sympathetic nerves are found further from the lumen and increase in thickness in renal arteries with larger diameters20. The authors conclude that effective RSD in these patients would need to be deeper and circumferential rather than interrupted. Hence, the aforementioned advantages of ultrasound RSD regarding circumferential denervation and penetration depth might provide particular benefits in patients with large renal arteries. Nevertheless, the need for randomised trials as a basis for general recommendations has to be emphasised again.
Limitations
Our study is obviously limited by the retrospective nature and the small patient population. Moreover, all patients received retreatment with the PARADISE system. Therefore, the superiority of this device cannot be derived from our data. Additional ablation points with other RSD devices could have resulted in similar treatment effects. Furthermore, we cannot completely exclude that the observed drop in BP might be due to late response to the first RSD with radiofrequency. However, all RSD procedures with the radiofrequency device were performed by experienced operators, the number of complete ablation runs was comparatively high, repeat ABPM demonstrated inadequate response and the time between the interventions was rather long. Hence, we are confident that the patient population consists of true non-responders to radiofrequency RSD.
Conclusions
RSD with the ultrasound-based PARADISE system seems to be safe and an effective therapeutic approach in patients not responding to radiofrequency RSD. However, final recommendations regarding first-line and second-line treatment strategies in patients with resistant hypertension cannot be given until the recent technical advances in denervation systems prove their efficacy in randomised trials.
| Impact on daily practice Primary non-response or delayed relapse after RSD for resistant hypertension is a challenging problem in daily clinical practice, since the interventional therapeutic options for these patients are sparse and consist mainly of repeat RSD or more invasive procedures (e.g., implantable devices to modulate carotid baroreflex sensitivity). Careful evaluation of the patient is imperative before considering a repeat intervention. Technological advances in RSD systems including energy delivery via ultrasound might overcome some drawbacks of the first-generation devices. This could improve procedural success and represent a therapeutic approach for patients not responding to a first intervention. However, the efficacy and safety of new devices need to be confirmed in randomised trials. |
Acknowledgements
The authors would like to thank Martin Petzold for his support in conducting this study.
Conflict of interest statement
P. Lurz has received speaker’s fees from Medtronic and is a consultant to ReCor Medical Inc. The other authors have no conflicts of interest to declare.