Abstract
Aims: The endovascular application of low-dose radiofrequency (RF) energy to the renal arteries results in effective ablation of sympathetic nerve fibres leading to a significant lowering of blood pressure (BP). This study aims to examine the feasibility and safety of renal denervation by the use of a standard electrophysiology (EP) catheter.
Methods and results: Twelve patients (mean age 62±14 years, nine male) with drug resistant hypertension despite medical treatment with at least four antihypertensive drugs underwent renal denervation by using astandard steerable RF ablation catheter with a 7 Fr diameter (Marinr®; Medtronic Inc., Minneapolis, MN, USA). Low-power RF applications have been applied along the length of both renal arteries, consecutively. Assessment of 24 hour ambulatory BP was done at baseline, at one, and at three months following RF ablation. The mean reduction of 24 hour ambulatory BP was –11/–7 mmHg at one month and –24/–14 mmHg at three months (p<0.01 for systolic and p<0.03 for diastolic blood pressure) with unchanged medication. No vascular complications have been observed in the short-term follow-up. The renal function as assessed by serum creatinine and proteinuria remained unchanged from baseline.
Conclusions: Our preliminary results indicate that the use of a standard RF ablation catheter is feasible and safe for sympathetic renal denervation as shown by a significant lowering of mean 24 hour ambulatory BP in comparison to baseline during short-term follow-up. Whether the use of a standard EP catheter for sympathetic renal denervation indeed improves the long-term outcome in resistant hypertension, however, remains to be investigated.
Introduction
Systemic arterial hypertension is one of the leading causes of disability or death due to stroke, heart attack, and kidney failure. Despite advances in the diagnosis and treatment of hypertension, its impact on cardiovascular health is continuing.1 Large clinical trials found an increasing prevalence of resistant and difficult-to-treat hypertension, defined as a blood pressure (BP) above target, despite medical treatment with three different antihypertensive drugs including a diuretic. It has been estimated that in about fifty percent of patients suffering from hypertension the BP remained uncontrolled in spite of adequate therapy.2 The failure to reach the target BP level is associated with an increased risk for cardiovascular complications.3 Therefore, research is focusing on the development of new effective therapeutic strategies to improve the management and control of these conditions. The over activity of the sympathetic nervous system especially of the kidneys plays an important role in essential hypertension. Thus, the renal efferent sympathetic activity and renal sensory afferent nerve activity might be a target to achieve an adequate BP control.4,5 Two recent published trials have demonstrated that the application of low-dose radiofrequency (RF) energy results in effective ablation of sympathetic nerve fibres which was accompanied by a significant lowering of BP.6,7 In these studies a special treatment catheter (Simplicity®; Ardian Inc., Palo Alto, CA, USA) introduced via a guiding catheter was used. Our study was conducted to prove the feasibility of using a standard steerable RF ablation catheter (Marinr®; Medtronic Inc., Minneapolis, MN, USA) to simplify this new intriguing method in treatment of resistant hypertension.
Methods
Patients
We included 12 patients with drug resistant hypertension. Patients were eligible if they had a mean 24 hour ambulatory systolic BP of 150mmHg or more, despite being treated with at least four antihypertensive drugs (mean 5.5). Written informed consent was obtained from all patients. Patients with renovascular abnormalities (including severe renal artery stenosis, previous renal angioplasty, or dual renal arteries) or known secondary causes of hypertension were excluded from intervention.
Study procedure
Prior to the ablation procedure, patients underwent baseline evaluations that included physical examination, review of medications, basic blood chemistries (including serum creatinine and proteinuria), and 24 hour ambulatory BP.
We performed bilateral common femoral artery punctures. Renal artery stenosis was excluded by renal angiogram via left femoral access (Judkins Right [JR 4] catheter; Cordis Corporation, Miami, FL, USA). After a second puncture of the right femoral artery astandard steerable RF ablation catheter with a7Fr diameter (Marinr®; Medtronic Inc., Minneapolis, MN, USA) was introduced into the renal artery. Using this bilateral approach we were able to inject contrast dye into the renal artery during ablation. RF ablation was performed in both renal arteries, consecutively. We applied low-power RF applications along the length of both renal arteries, consecutively (separated both longitudinally and rotationally to achieve a circumferential lesion). Impedance and temperature were continuously monitored during RF ablation. A continuous infusion of unfractionated heparin with an activated clotting time target range between 250 and 300 seconds was administered after an initial bolus injection (100units/kg). Subsequently, all patients received aspirin 100 mg per day for three months. Follow-up assessments at one and at three months consisted of office BP measurement, 24 hour ambulatory BP, physical examination, blood chemistries (including serum creatinine and proteinuria) and adverse events.
Statistical analysis
Continuous variables are expressed as mean±standard deviation (SD). Categorical data are summarised as frequencies and percentages. Differences in blood pressure between baseline and follow-up were analysed using the paired Student’s t-test for continuous variables. Apvalue <0.05 was considered statistically significant. The statistical analyses were computed with SPSS© (SPSS Inc., Chicago, IL, USA) statistical software.
Results
Twelve patients with drug resistant hypertension underwent renal denervation (mean age 62±14 years, nine male). Some of the patients had severe comorbidity (six patients with diabetes mellitus, two patients with coronary artery disease, and four patients with chronic renal insufficiency defined as serum creatinine levels >130µmol/l). Baseline parameters of patients are shown in Table1. Six ablations were performed within each renal artery with a maximum duration up to 1 min. each. Energy delivery was titrated to a maximum of 8-13 watts. Electrode temperature (mean 47±6°C) and impedance (mean 225±24ohms) were monitored continuously during each energy application. The mean fluoroscopy time was 8.6±3.5min. Intravenous narcotic and sedative drugs (fentanyl titrated up to 0.15mg and midazolam 4mg) were administered for the diffuse visceral abdominal pain occurring during RF ablation. The pain was limited to the duration of RF energy delivery. After the procedure a final renal angiogram was performed showing focal renal artery irregularities immediately after RF energy delivery in three patients. However, none of these irregularities were flow limiting at procedure termination. A typical example of renal angiography before, during and immediately following RF ablation is shown in Figure1 A-C. We did not observe vascular complications during follow-up. No patient was lost to follow-up. The mean reduction of 24 hour ambulatory BP was –11/–7mmHg at one month and –24/–14mmHg at three months with unchanged medication (Figure2A). Three months after the procedure, both systolic and diastolic BP were significantly lower than baseline BP (p<0.01 for systolic and p< 0.03 for diastolic BP). The absolute changes in systolic and diastolic BP of individual patients are shown in Figure2B. In three patients (25%) the BP did not change significantly. The renal function assessed by serum creatinine and proteinuria remained unchanged from baseline. Renal duplex sonography during follow-up found no evidence of renal artery stenosis or other abnormalities in all patients.
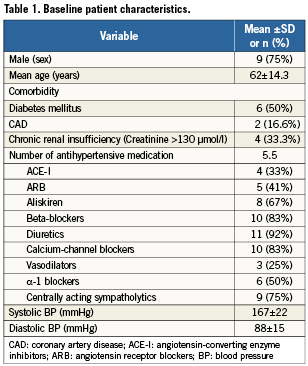
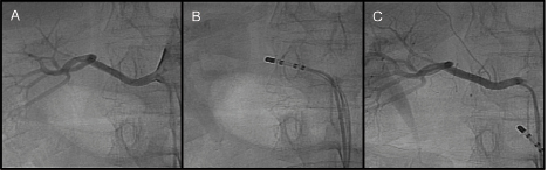
Figure 1. Angiography of the right renal artery at baseline (A), during RF ablation (B), and immediately following the procedure (C). Nosignificant stenosis of the renal artery was observed. Focal renal artery irregularities occurred immediately following the RF ablation, which were not flow limiting at procedure termination.
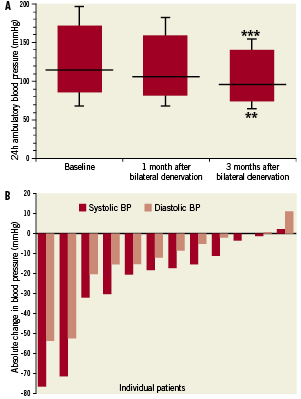
Figure 2. A) Mean changes in blood pressure at different time points following renal sympathetic denervation. The boxes show mean systolic and diastolic BP (with standard deviation) and the pulse pressure at baseline, at one month and at three months after intervention. Black line: mean arterial pressure. ** p<0.03, ***p<0.01, compared to baseline. B) Individual changes in mean blood pressure. The absolute change in mean systolic and diastolic BP three months following renal sympathetic denervation in patients with drug-resistant hypertension is shown. In three patients (25%) the blood pressure remained unchanged.
Discussion
In our study, we found that low-dose RF energy ablation of the renal artery in order to perform sympathetic renal denervation by using a standard steerable RF ablation catheter (Marinr®; Medtronic Inc., Minneapolis, MN, USA) is feasible and safe during short-term follow-up. The mean reduction in 24 hour ambulatory BP was –24/–14mmHg at three months after sympathetic renal denervation which is compatible with the results of the trial by Krum and co-workers that found a mean reduction of office BP of –21/–10mmHg6 and also with the results of the Symplicity HTN-2 trial that showed a mean reduction of office BP of –24/–8mmHg7. In our study, nine of twelve treated patients (75%) could be classified as responder to sympathetic renal denervation defined by a reduction in systolic BP of 10mmHg or more at three months after RF ablation. The Symplicity HTN-2 Trial found 84% of the treated patients to be responder to the renal denervation therapy at six-month follow-up. The time points of data assessment (three versus six months) might be one reason for the different responder rates in the studies. In fact, during the follow-up period of the Symplicity HTN-2 trial, the blood pressure reduction improved six months following renal denervation in comparison to the three-month follow-up visit.7 Furthermore, the differences in the results of the studies despite the use of the same energy source (RF) might be due to technical aspects. In contrast to the recently published trials6,7 we describe for the first time the use of a standard steerable RF ablation catheter for sympathetic renal denervation.
Differences in the performance of the catheters used in the studies (e.g., shaft torsion and stiffness characteristics as well as tip buckling and bond strengths) might be accompanied by differences in contact pressure and catheter tip temperatures that are important determinants for radiofrequency current-induced lesion size.8 However, neither in the study of Krum and co-workers6 nor in the Symplicity HTN-2 Trial7 temperatures and impedances achieved during ablation have been described. Furthermore, the RF application time in our study was shorter (up to 0.5 to 1 min each of 8-13 watts) compared with that described by Krum and co-workers (up to 2min).6 No serious complications related to the device or procedure have been observed. Serum creatinine and proteinuria as markers of renal function remained unchanged from baseline. Renal duplex sonography during follow-up found no evidence of renal artery stenosis or other abnormalities in all patients. These findings are also in agreement with recent published trials.6,7 One advantage of our approach is the broad availability of the standard steerable RF ablation catheter. With our technique it is possible to use the standard equipment of the electrophysiology laboratory (e.g., standard RF generator). The handling of the EP catheter is easy if the examiner is familiar with this technique and the performance of the catheter is non-traumatic as shown during RF ablation of the coronary venous system and the aortic sinus for ablation of ventricular arrhythmias.9 However, our preliminary study has some limitations. Since it was not a randomised placebo controlled clinical trial we cannot exclude that placebo effect might contribute to the BP lowering observed in our study. On the other hand, the recently published randomised Symplicity HTN- 2 trial has confirmed the benefit of the catheter-based renal sympathetic denervation procedure.7 Furthermore, the number of treated patients is small and the follow-up time is short. However, current available data show that already three months after renal denervation a significant reduction in BP is detectable.6,7 Even in our small group of treated patients we found a significant lowering of mean 24hour ambulatory BP in comparison to baseline expressing the efficiency of the new treatment.
In conclusion, our preliminary data indicate that the use of astandard RF ablation catheter is feasible and safe for sympathetic renal denervation in patients with drug-resistant hypertension as shown by a significant lowering of mean 24hour ambulatory BP in comparison to baseline during short-term follow-up. Whether the use of a standard EP catheter for sympathetic renal denervation indeed improves the long-term outcome in resistant hypertension, however, remains to be investigated.
Conflict of interest statement
The authors have no conflict of interest to declare.

