Abstract
Aims: To prove the efficacy and safety of renal sympathetic denervation as a new treatment option for patients suffering from resistant hypertension in a real-world setting.
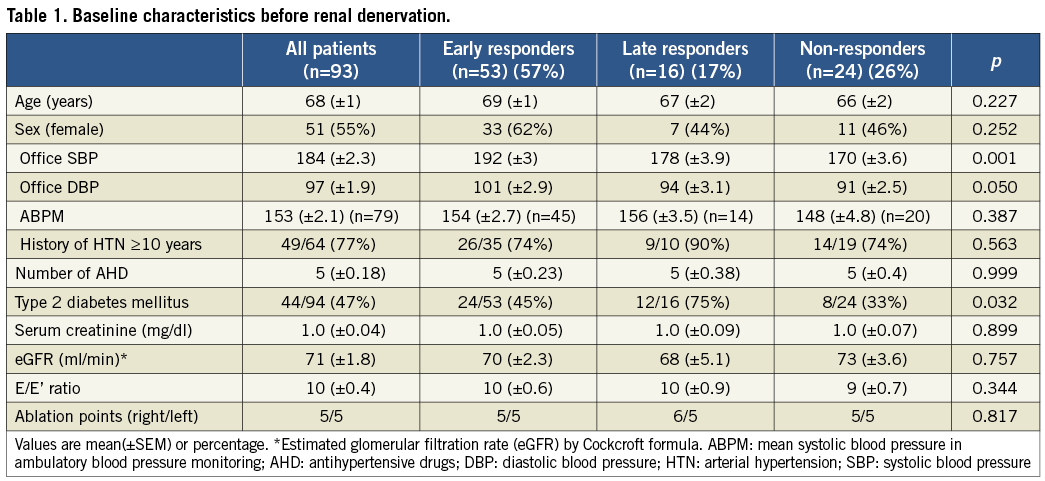
Methods and results: This single-centre real-world registry included 93 patients who underwent renal denervation employing the Symplicity system. Patients were followed for six months. The patient cohort was divided into early responders with a reduction of office systolic blood pressure >10 mmHg three months after the procedure (n=53, 57%), late responders (six months after the procedure, n=16, 17%) and non-responders (n=24, 26%). After six months, systolic blood pressure was lowered by 46±2.9 mmHg (mean±SEM, p<0.001), 31±3.4 mmHg (p<0.001) and 7.1±3.3 mmHg (p=0.79, ns), respectively. Ambulatory blood pressure monitoring also showed a significant reduction in the early responder group (20±5.7 mmHg, p=0.002). We subjected eight patients to a re-do procedure which led to a significant reduction of blood pressure in another five patients after six months (63%). One patient in this cohort developed a one-sided renal artery stenosis associated with an increase in blood pressure.
Conclusions: This real-world analysis of renal sympathetic denervation confirms the procedure to be safe and efficient in the majority of patients. Non-responders may profit from a second ablation, arguing in favour of the hypothesis that the procedure did not destroy sufficient amounts of sympathetic innervation in these patients. However, repeated denervations may also increase side effects.
Introduction
Arterial hypertension is the main risk factor for diastolic and systolic heart failure, atrial fibrillation, stroke, renal failure and arteriosclerosis1-3. Many patients do not reach the recommended blood pressure guideline values of <140/90 mmHg while on drug therapy4. The Symplicity™ renal denervation system (Medtronic, Minneapolis, MN, USA) targets the afferent and efferent sympathetic nerves of the kidney to reduce blood pressure. This system was investigated by the Symplicity HTN-1 safety and feasibility study and the Symplicity HTN-2 randomised trial which were positive regarding their primary endpoint5,6. These studies included patients with office-based systolic blood pressure values ≥160 mmHg (≥150 mmHg for patients suffering from diabetes) while on drug therapy. Recently, the one-year results of the Symplicity HTN-2 trial, including a crossover group after six months, confirmed the initial findings7. Since these studies were published, renal denervation has rapidly been adopted in routine care within the European community8.
The available studies have found a significant blood pressure reduction (defined as a reduction of office-based measurement of systolic blood pressure of ≥10 mmHg) at six months following the procedure in around 80% of patients, which was maintained at 12 months. Reliable data of 24 hr ambulatory blood pressure were missing in the first Symplicity trials but are now available, and underline the efficacy of renal denervation9. Smaller substudies and non-randomised trials additionally found a positive effect on diabetes control and cardiac hypertrophy10,11.
Here we describe the first results of a single-centre, real-world registry including 93 patients. We collected all available routine data before, as well as three and six months after, renal denervation on blood pressure, drug therapy and end-organ damage including echocardiographic parameters of diastolic heart failure. In addition, we investigated a small cohort of eight patients who were subjected to a second denervation procedure (“re-do”) because of no or insufficient reduction of the systolic blood pressure after the first renal denervation procedure. These patients were followed up for another six months after the second procedure.
Methods
The Asklepios Klinik St. Georg blood pressure (ALSTER BP) registry is a single-centre, real-world, all-comers registry performed at the Department of Cardiology at the St. Georg hospital in Hamburg between July 2010 and July 2012. The primary objective was to collect all available clinical follow-up data of patients treated with renal sympathetic denervation employing the Symplicity™ renal denervation catheter system (Medtronic). Patient selection criteria mostly matched the published criteria of the randomised Symplicity HTN-2 trial6. Moreover, we also included four patients with reduced kidney function with eGFR <45 ml/min. Briefly, adult patients aged 40-85 years with essential hypertension and treated with three or more antihypertensive drugs were routinely checked for blood pressure control. Patients were eligible for renal denervation if they presented with systolic blood pressure >160 mmHg either measured invasively during a routine coronary angiogram or using outpatient documentation while on three or more antihypertensive drugs. We checked drug compliance by taking a detailed history.
On the day of admission, patients received a routine screening including measurement of blood and urine electrolytes as well as blood pressure on both upper extremities. These excluded the most frequent reasons for secondary hypertension such as hyperaldosteronism, Cushing’s syndrome and phaeochromocytoma or anatomically related blood pressure elevation at the measurement point. Twenty-four hour ambulatory blood pressure measurements as well as an echo regarding diastolic dysfunction were performed if not already available from outpatient screening analysis. Renal denervation was performed according to locally developed standards: following angiographic visualisation of the renal arteries, including accessory pole arteries, all renal arteries with a diameter larger than 3 mm were selectively intubated. In order to minimise patient discomfort and dislocation of the ablation catheter due to patient movement, patients received sedation and analgesia. A bolus of fentanyl (0.05 mg), midazolam (2 mg) and propofol (5 ml 10% solution) was administered at the start of the procedure followed by a continuous infusion of propofol at a rate of 15-30 ml/hr depending on patient weight. A Guedel tube was placed: generally, tolerance of the Guedel predicted that the patient had no discomfort during ablation. The bolus of fentanyl was repeated every 15-30 minutes. In order to limit the use of contrast medium we performed hand injection of a 50:50 mix Imeron 350/0.9% sodium chloride solution to visualise the artery.
Starting from the most distal point of the renal artery prior to the intra-renal branches that had a diameter of >3 mm, ablation points were selected with a spiral-like pattern approximately every 5 mm. If anatomically feasible, between four and eight complete two-minute ablations were performed per artery. Accessory arteries >3 mm diameter received one superior, proximal treatment. The access site was closed using standard vascular closure devices - Angio-Seal™ 6 Fr (St. Jude Medical GmbH-Germany, Eschborn, Germany), EXOSEAL® 6 Fr (Cordis, Johnson & Johnson, Warren, NJ, USA). Patients received dual platelet inhibition for one month following the procedure. In cases of oral anticoagulation, patients only received additional clopidogrel and no ASA. Patients were discharged the day after the procedure after routine measurement of creatinine values as well as inspection of the access site regarding secondary haematoma. Routine clinical data were collected from various sources: patients were followed by telephone interview and offered an outpatient visit to the department three and six months after the procedure. Additionally, the referral doctors were asked to provide examination results. All available data from routinely performed examinations regarding symptomatic self-assessment, blood pressure measurements, 24 hr ambulatory blood pressure as well as lab values regarding renal function and other parameters such as echo parameters of diastolic dysfunction were collected. Patients were advised to continue the drug regimen they had received prior to renal sympathetic denervation.
Statistical analysis
Descriptive statistics were used to present results for the baseline parameters and treatment effects. Intra-individual comparisons of baseline values vs. follow-up measurements were performed using a paired Student’s t-test. Comparisons of quantitative baseline characteristics between the defined groups were performed using a one-way ANOVA analysis and post hoc t-tests with p-values adjusted by the false discovery rate method. Categorical data were compared by chi-square analysis. A difference was considered significant if the one-sided α-level was ≤0.05. All analysis was performed employing GraphPad Prism, version 5 (GraphPad Software Inc., La Jolla, CA, USA).
Results
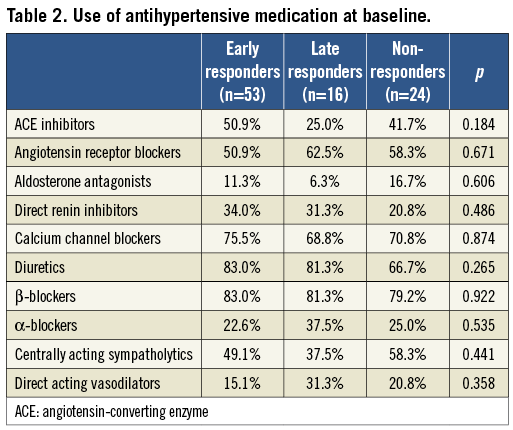
Patient baseline characteristics are summarised in Table 1 and Table 2. In comparison to patients in the pivotal Symplicity HTN-2 trial, patients in the ALSTER BP registry were older (59±15.5 vs. 68±9.3 years, respectively)7. More female patients were treated in the ALSTER BP registry (55% vs. 33% in Symplicity HTN-2), while the total number of included patients was similar (n=93 in ALSTER BP vs. n=92 in one-year results of Symplicity HTN-2). Baseline systolic blood pressure, number of antihypertensive drugs, eGFR and rate of diabetes (47%) were similar (Table 1, Table 2). Ablation was completed in all patients, defined as delivery of 8 watts for a full 120 seconds at ≥4 ablation sites. We found sufficient analgesia to be important also for technical ablation success, as patient discomfort often led to displacement of the ablation catheter during ablation due to heavy breathing and/or movement of the patient. Difficult anatomy of the renal artery was in part negotiated with a 5-in-6 GuideLiner™ catheter (Vascular Solutions Inc., Minneapolis, MN, USA) directed to the renal artery over a standard coronary guidewire. In cases of local “spasms”, ablation was still finished with additional points set more proximally and at a 10 mm distance. It appeared to us that “spasms” were more likely to occur if the vessel diameter was smaller than 4 mm. Treatment of “spasms” by locally administered nitroglycerine or other drugs was found not to be effective. If severe spasms >90% persisted, a control angiography after >7 days was scheduled. This showed complete resolution without further treatment in all cases (n=3), supporting the recent hypothesis that “ablation notches” are in fact tissue oedema rather than true spasms. There was one acute renal artery dissection treated successfully with a stent: this occurred prior to insertion of the ablation catheter following positioning of the guiding catheter. At that time this was an 8 Fr guiding catheter, necessary when working with the first-generation Symplicity catheters. There was no documented renal artery stenosis following a single renal denervation procedure. However, there was neither routine invasive follow-up nor a scheduled ultrasound assessment.
Safety
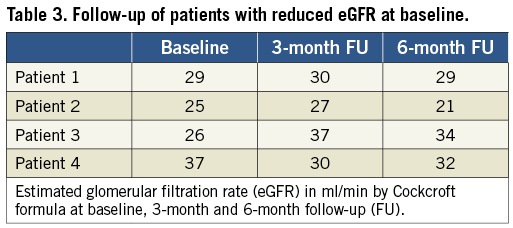
Safety of the procedure regarding eGFR was remarkable. In patients with reduced eGFR a standard regimen of sodium bicarbonate and ACC was administered prior to the procedure and contrast was limited to a maximum of 60 ml as established also for PCI in our department.
No safety issue was observed regarding renal function during the follow-up period even in patients with a basal eGFR <45 ml/min (n=4) (Table 3). This observation is similar to larger data sets from coronary angiography, where limitation of contrast medium use to below 80 ml total, adequate hydration and urine alkalisation with sodium bicarbonate prior to contrast medium exposure have resulted in a significant reduction of contrast-induced nephropathy12. Despite ongoing dual antiplatelet therapy, one case of a small kidney infarct, which was associated with sudden pain in the lower back 10 days after the renal denervation and documented by MRI, was reported to the centre by an external nephrologist. An association with a possible small thrombus at one of the ablation sites appears likely; however, the case did not have especially prominent ablation notches or other angiographic abnormalities. In this series of patients subjected to one complete renal denervation procedure, we subjected eight patients to a repeat angiography due to persistent hypertension despite ablation, recurrent hypertensive crisis or a possible rebound phenomenon. None of these patients had developed a renal artery stenosis confirming prior data that this is a rare event. The visual experience in the 93 patients reported here was, however, that ablation in close proximity to angiographic visible plaques results in increased incidence of reversible spasms/oedema and should be avoided.
Blood pressure reduction
At three months after the procedure, 57% (n=53) of our patients could be classified as responders, defined by a decrease of systolic office-based blood pressure of more than 10 mmHg (Figure 1). In fact, these early responders demonstrated a highly significant reduction of 38±2.6 mmHg after three months and 46±2.9 mmHg after six months compared to their baseline levels (mean±SEM, p<0.001). In parallel, mean 24 hr systolic ambulatory blood pressure also decreased by 8±2.3 mmHg (p<0.01) after three months and 20±5.7 mmHg after six months in this group (p<0.01) (Figure 2). Table 4 summarises the number of patients with reductions by 11-20, 21-30 and >30 mmHg regarding their office-based blood pressure values - the distribution of patients is even among these groups. Patients did not change medication significantly during this time (mean number of drugs: 5±0.2 [mean±SEM], both at baseline and first follow-up). Obviously, it was not possible to control for compliance of the patients within this registry; however, patients were interviewed regarding this aspect during baseline and follow-up examinations.
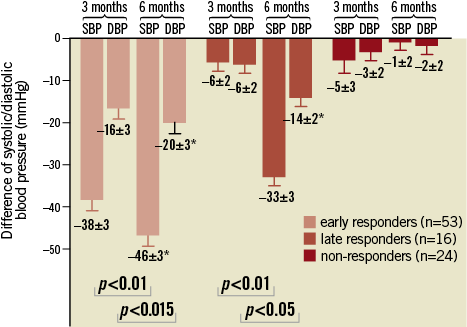
Figure 1. Change of mean systolic (SBP) and diastolic blood pressure (DBP) by office-based measurement in mmHg (±SEM) three and six months after renal denervation in patients classified as early, late or non-responders. The early and late responders showed a significant reduction of the SBP and DBP at six months after renal denervation compared to baseline (*p<0.01).
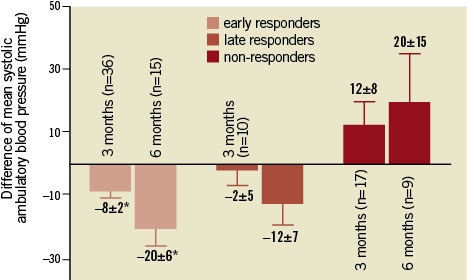
Figure 2. Change of mean systolic blood pressure by ambulatory blood pressure measurement in mmHg (±SEM) three and six months after renal denervation. The early responders showed a significant reduction compared to the baseline value (*p<0.01). The differences in the late and non-responder groups are not statistically significant.
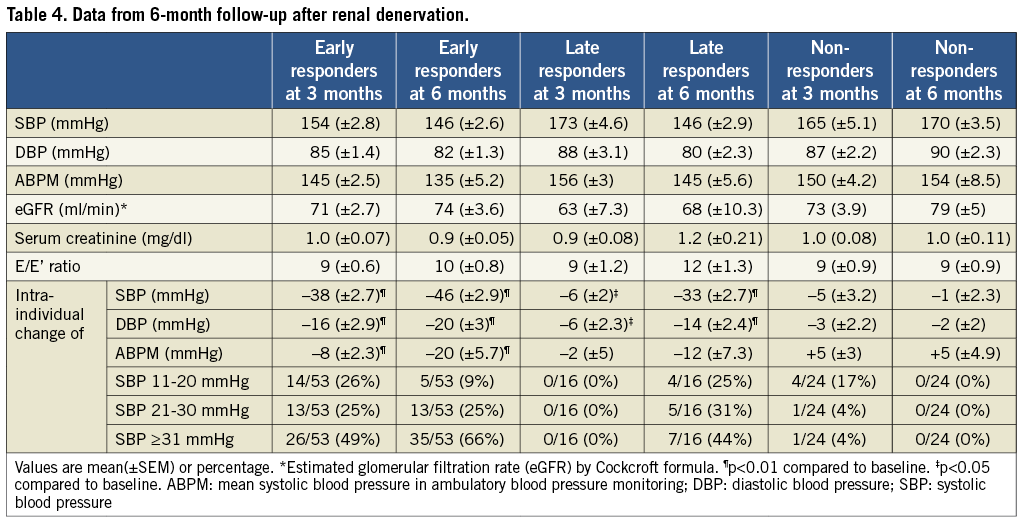
We identified a second group of patients consisting of another 17% (n=16) of our cohort, which we termed late responders because a blood pressure reduction >10 mmHg could not be determined after three but only after six months. This group demonstrated no significant reduction of systolic blood pressure after three months (-6±2.3 mmHg); however, after six months blood pressure had dropped by 33±2.7 mmHg (p<0.001) (Figure 1). Interestingly, this patient cohort was likely to have type 2 diabetes (75% in the late responder cohort, p<0.05). In addition, 90% of the late responders were on antihypertensive drugs for more than 10 years (early responders: 74%, p=0.563). Neither number of ablation points nor number of antihypertensive drugs, eGFR or age was different between early and late responders.
We collected data on several parameters of end-organ damage including echocardiographic measurement of E/E’ as a measure of diastolic dysfunction, HbA1c as a measure of diabetes control, serial creatinine measurements to follow eGFR and symptoms of dyspnoea. We found no effect of renal denervation in our cohort by six months on HbA1c similar to the published data. We did not perform fasting glucose tests11.
We identified a third cohort consisting of 26% of our patients here called “non-responders”, which did not show a significant blood pressure reduction after six months. In comparison to the early and late responders the non-responders had the lowest systolic (p<0.01) and diastolic (p<0.05) blood pressure at baseline (Table 1). We were not able to identify any other parameters predicting non-responders. Neither age nor diabetes, sex, duration of antihypertensive drug treatment, number of ablation points or eGFR was significantly different to the overall population. Larger cohorts may be required to perform multivariate analysis.
The Symplicity HTN-2 investigators recently published the one-year data of the study including crossover patients after the initial study phase of six months7. In that study, no additional effect on blood pressure reduction was found after the first six months. We had previously decided to offer a second procedure outside the current guidelines to patients if they did not show a sufficient reduction of their systolic blood pressure after six months. Further criteria included insufficient symptom control as well as progressive end-organ damage such as heart failure. We have completed the six-month follow-up of all patients treated within this re-do group. The cohort consisted of eight patients. The re-do ablation procedure was performed in a similar manner to the initial ablation with four to six ablation points in a spiral pattern from distal to proximal. We observed blood pressure reduction in five out of eight (63%) re-do patients (Figure 3). These data support the hypothesis that two ablation procedures were necessary to destroy a sufficient percentage of sympathetic nerve fibres to optimise blood pressure control.
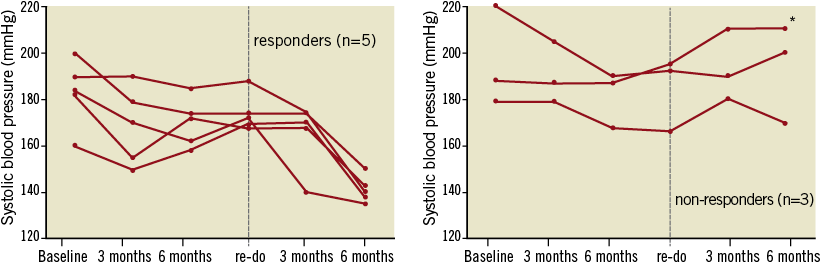
Figure 3. Individual follow-up after re-do procedures: systolic blood pressure (office-based measurement) before (baseline), three and six months after the first renal denervation procedure, at the time point of the re-do procedure and again three and six months after the re-do procedure. Eight patients were followed up. Five patients (63%) showed a reduction of their systolic blood pressure >10 mmHg six months after the re-do (responders), three patients showed no reduction >10 mmHg (non-responders). One patient showed a significant renal artery stenosis five months after the re-do procedure (*).
The re-do procedure at >6 months after the initial treatment (9±0.8 months) did not result in impairment of renal function or acute damage to the vessel. However, one patient (13% of the total cohort) demonstrated a rebound phenomenon regarding her blood pressure leading to a hypertensive crisis five months after the re-do procedure. The workup included a CT angiogram of the abdominal aorta that showed a new renal artery stenosis on the right side. This was confirmed by angiography and the stenosis was treated with a renal artery stent (Figure 4). The lesion was present at one of the ablation points from the first and second procedure. The timing strongly suggests that the ablation procedure was causal for the new stenosis. Apart from this one case, no other side effects were observed.
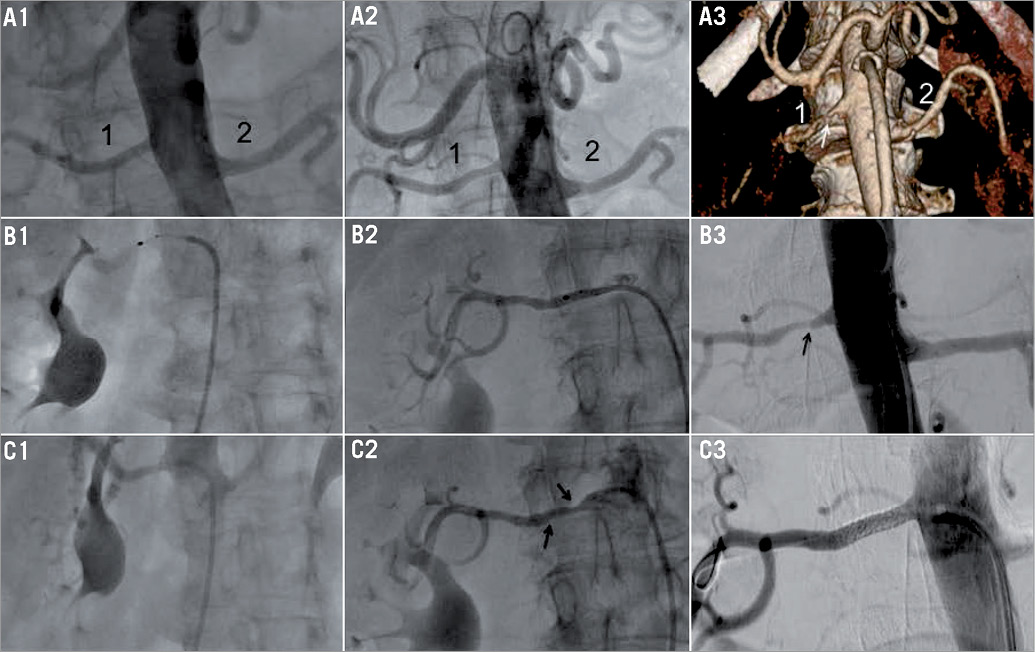
Figure 4. Stenosis of the right renal artery following repeated renal denervation procedures. The number 1 indicates the right and the number 2 the left renal artery. (A1-C1) Baseline. (A1) Angiography before first renal denervation procedure with completely intact renal arteries, (B1) radiofrequency application in the right renal artery, (C1) angiography after first renal denervation procedure with minimal spasm at the ostium. (A2-C2) Re-do procedure 7 months after the initial procedure. (A2) Angiography before second renal denervation procedure: a minimal plaque is now visible in the proximal part of the right renal artery. (B2) Radiofrequency application in the right renal artery during second procedure, and (C2) angiography after second renal denervation procedure showing 2 ablation notches. (A3-C3) Analysis of the renal arteries 5 months after the re-do procedure. (A3) 3D reconstruction of computed tomography with contrast showing a high grade stenosis of the right renal artery 5 months after the second procedure: patient had been re-admitted due to a hypertensive crisis. (B3) Angiography showing a 75% stenosis of the right renal artery located in the proximal but not ostial part of the artery. (C3) Angiography after stent implantation (Herculink 4.5/15 mm; Abbott Vascular, Santa Clara, CA, USA) into the right renal artery.
Discussion
Safe and effective control of essential hypertension by ablation of sympathetic nerves along the renal arteries does provide a new therapeutic approach for many currently undertreated patients. Randomised trials need to be confirmed in real-world settings. The ALSTER BP all-comers registry allows the assessment of the effect and time line of introducing this therapy into routine treatment. The patients in our cohort were significantly older and we included more female patients compared to the Symplicity HTN-2 trial. This represents the real-world patient cohort in Germany that will not achieve blood pressure control on three or more drugs13. Very similar to the Symplicity HTN-2 trial, almost 50% of our patients were also diagnosed with diabetes. According to the pivotal UKPDS study, long-lasting blood pressure control is even more important to prevent end-organ damage in these patients14. The majority of patients in this registry had E/E’ values ≥8 (72%) suggestive of heart failure with preserved ejection fraction (HFPEF). This is a typical finding in this patient cohort with long-standing hypertension. As HFPEF is related to increased morbidity and mortality, it is mandatory to offer additional therapy such as renal denervation to these patients15,16.
This real-world registry found roughly 70% of patients with significantly reduced systolic blood pressure (“responders”) six months after renal denervation employing the Symplicity renal denervation system. The responder group can be further divided into early responders (blood pressure reduction after three months) and late responders (response observed between three and six months following renal denervation). Type 2 diabetes mellitus was a significant predictor of a late response. This is a new and interesting observation raising some questions about the underlying mechanisms, for example, of vessel remodelling and innervation following renal denervation, as diabetes typically afflicts these processes. It remains unclear whether further blood pressure reduction and/or an increase in the numbers of responders occurs after six months. The best available data were recently published describing the one-year data from the Symplicity HTN-2 trial including a crossover group. No further blood pressure reduction was found in that trial beyond six months (six months: –31.7±23.1 [mean±SD], 12 months: –28.1±24.9 mmHg)7. We conclude that it is unlikely that patients not showing any response after six months will demonstrate a later response.
We also found a significant reduction in mean 24 hr ambulatory systolic blood pressure values in the early responder group. The late responders showed a trend towards reduction that was statistically not significant, most likely due to the small number of patients in that group. According to the latest investigations of a multicentre analysis with ABPM data of 346 patients, office blood pressure reduction was more pronounced than the reduction in ABPM we observed here9. Data from large prospectively collected cohorts have set an even tighter threshold to mean ambulatory blood pressure than the statistically derived measurements: optimal 24 hr ABP is 125/75 mmHg to yield a normal cardiovascular risk profile17. If these values are regarded as the aim of hypertension treatment, renal denervation, in addition to the well-established combination drug treatment, is a valuable addition to the treatment armamentarium for many hypertensive patients.
The side effects of renal denervation in our cohort were limited to access-site complications such as haematoma. Renal function remained stable following denervation even in those patients with an eGFR <45 ml/min, comparable to other described patients with chronic kidney disease in a small pilot study18. It is mandatory in these patients to take the usual precautions also established for coronary angiography, namely limiting the use of contrast medium and hydration12.
Twenty-six percent of the patients included in this real-world registry had to be classified as “non-responders”. The change in systolic blood pressure of this group at six months was negligible (–7±3.4 mmHg). So far, the only reliable predictor for the effectiveness of renal denervation procedures seems to be the office blood pressure at baseline, as described in other studies19. In our registry also, higher blood pressure values at baseline correlated to higher blood pressure reduction at three and six-month follow-up. A predictor for non-response could not be identified; until now it is unknown whether renal sympathetic innervation is involved in blood pressure control of these patients or whether the ablation procedure might not be effective in such patients. However, animal studies have previously confirmed the central role of renal sympathetic innervation in almost all models of essential hypertension20. The limitation may rather be found in the “blinded” ablation currently performed: there is no routine method to confirm reduced sympathetic activity following renal denervation.
To our knowledge, this is the first report on results of re-ablation for non-responders as classified six months after the procedure. The re-do procedure, clearly outside current recommendations, was performed in patients with persistent symptomatic hypertension and progressive end-organ damage, such as HFPEF, or renal failure21. Sixty-three percent of patients in the re-do group showed a significant blood pressure reduction six months after the re-do procedure (approximately 15 months after the initial procedure); however, one renal artery stenosis (13% of patients) probably related to the repeated denervation procedure was observed in this group. The patient presented with rather small renal arteries (3.8 mm mean diameter), which we find to be prone to spasms and possibly also to endothelial damage following radiofrequency ablation. However, there are reported cases in which renal denervations in small arteries were performed without short-term complications22. Still the question arises as to how to limit such damage, as re-ablation may put the patient at an especially high risk of repeated endothelial damage and renal artery stenosis. Irrigated catheters may possibly decrease the risk of endothelial damage. Such catheter types for renal denervation have recently become available in Europe: initial results are promising but must be confirmed in larger trials23. Optical coherence tomography (OCT) may be a useful tool to analyse endothelial damage after radiofrequency ablation – initial results have been presented24.
Limitations
The limitations of this registry-based study can be found in the circumstances of a real-world approach. Not all patients could be followed up in-house; some data were collected from the referring practitioners. Therefore, blood pressure measurements have not been performed in a standardised manner. To minimise the impact of the assumed impreciseness we have chosen to use cut-off values that were more likely to give an accurate view of the responder rates (>10 mmHg rather than ≥10 mmHg). Clearly, these limitations could be seen as a weakness compared to randomised studies. However, we believe this approach gives additional interesting data since many practitioners will observe the exact same results. Moreover, the results are still comparable to the published data of other investigated cohorts and in our view give an even more powerful view of the impact of renal denervation in a real-world setting.
Conclusions
In summary, we find denervation of the renal sympathetic innervation employing the Symplicity system to be both effective as well as safe in a real-world setting. Based on these results, as well as the published randomised trials, we believe renal denervation should be offered to all patients who present with systolic blood pressure outside the current recommended values (>140 mmHg systolic office-based BP) despite three or more drugs. Achieving blood pressure control in these patients will most likely dramatically reduce end-organ damage including infarct, heart failure, renal failure and stroke, in terms of the detrimental effects of uncontrolled hypertension. Further studies need to evaluate these effects beyond measuring blood pressure in this patient cohort.
| Impact on daily practice The ALSTER BP real-world registry results show a positive effect on blood pressure values in 74% of the included patients without any other specific additional therapy. Many patients within the registry showed a long-term history of arterial hypertension as well as comorbidities like diabetes and have already been treated with the most established drug regimens, including ACE-inhibitors, calcium channel antagonists, diuretics and even new substances like direct renin inhibitors. The UKPDS study showed the highest risk of further end-organ damage without additional therapy for these patients, who therefore can particularly profit from the growing availability and ongoing improvement of renal denervation. |
Conflict of interest statement
Karl-Heinz Kuck receives speaker honoraria and grant support from Biosense Webster, Medtronic and St. Jude. Martin Bergmann receives speaker honoraria from Medtronic, Covidien and Biosense Webster. The other authors have no conflicts of interest to declare.

