In the initial stages of the renal denervation (RDN) “saga”, catheter-directed radiofrequency ablation was associated with a significant blood pressure (BP) reduction in hypertensive patients, generating enthusiasm and expectations. However, the subsequent sham-controlled studies produced contrasting results and RDN was substantially discouraged in consensus statements and international guidelines1.
Subsequently, several methodological issues were raised concerning the design of the sham-controlled studies, including the completeness of denervation, variable adherence to antihypertensive therapy, frequent medication changes, and the limited training and experience of the proceduralists. Second-generation trials were then encouraged and designed with the aim of overcoming all the possible drawbacks of the first-generation RDN trials1.
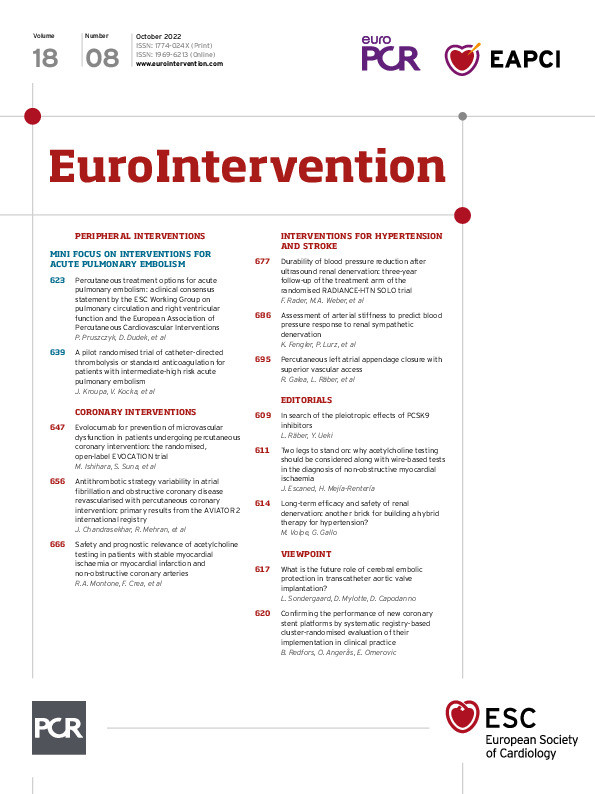
Along this conceptual line, different sham-controlled studies were initiated to test the efficacy and safety of RDN, mostly as an adjunctive treatment strategy in selected patients. Among these new-generation trials, the RADIANCE-HTN SOLO (A Study of the ReCor Medical Paradise System in Clinical Hypertension) 2, a multicentre, international, single-blind, randomised, sham-controlled trial investigating endovascular ultrasound renal denervation to treat hypertension, enrolled patients with combined systolic–diastolic hypertension, aged 18-75 years, with an ambulatory BP ≥135/85 mmHg and <170/105 mmHg after a 4-week discontinuation of up to 2 antihypertensive medications and with suitable renal artery anatomy. A targeted endovascular catheter-based denervation of the renal efferent and afferent nerves with a minimally invasive approach was performed. In the original cohort, 74 subjects were allocated to renal denervation and 72 to the sham procedure. The primary endpoint of change in daytime ambulatory systolic BP at 2 months was significantly reduced in the RDN group compared with the sham-operated group2.
In this issue of EuroIntervention, Rader and colleagues report the 3-year follow-up results of the RADIANCE-HTN SOLO trial with the important aim of assessing the long-term safety and efficacy of RDN on office BP (OBP)3. Of the 74 patients originally randomised to RDN, 51 patients completed the 36-month follow-up. For this subgroup, OBP decreased by 18/11±15/9 mmHg from baseline (p<0.001), with an improvement of BP control (<140/90 mmHg) from 29.4% at screening to 45.1% at 36 months (p=0.059). Changes in office systolic BP (SBP)/diastolic BP (DBP) from screening (before washout) to 36 months were –8/–4 ±17/11 mmHg (p<0.001 and p=0.004, respectively). For patients uncontrolled at screening (n=36), systolic OBP decreased by 10.8 mmHg (p<0.001) at 36 months while maintaining similar antihypertensive medications (p=0.158)3.
The long-term results of this trial are undoubtedly relevant. They include, in particular, a sustained antihypertensive efficacy, supported by the decreases in OBP from screening (before washout of antihypertensive therapy) and from baseline (after washout), independent of the number of prescribed medications and in the presence of a substantially good safety profile. However, a number of key questions remain unanswered.
First, at screening, patients received an average of 1.2 medications, and ~16% were not pharmacologically treated. While previous guidelines recommended starting treatment with monotherapy4, the current European5 and US6 guidelines recommend a combination therapy strategy in most patients. Indeed, more than three-quarters of hypertensive patients failed to achieve therapeutic targets with a monotherapy approach. In fact, in the RADIANCE-HTN SOLO trial, at initial screening OBP was not controlled (145/92±14/10 mmHg), and only 33% of hypertensives received 2 BP-lowering medications. After medication washout, BP further increased by 9.3±12 mmHg. Antihypertensive treatment should be started immediately and maintained in patients with Grade 2 and Grade 3 hypertension with the aim of reaching adequate BP control within 3 months578. In fact, the available evidence suggests that the prevailing benefits of BP control are associated with the early achievement of therapeutic targets, resulting in a more effective and sustained BP lowering and in a reduction of the impact of cumulative cardiovascular (CV) risk exposure9.
Second, recent international guidelines now recommend more ambitious targets compared to the former BP therapeutic goals and indicate that BP values <130/80 mmHg should be achieved in patients aged <65 years if therapy is tolerated5678. Indeed, different studies and meta-analyses conducted in the last few years strongly support the concept that “lower is better” for hypertension control, showing significant reductions in the rate of combined major CV events, myocardial infarction, stroke, heart failure, and all-cause mortality in patients treated with more intensive BP-lowering strategies10. In the present study, however, only a quarter of the study population had normalised BP levels at 2 months, and only a minority of patients (45% in the RDN group) achieved BP targets <140/90 mmHg at 3-year follow-up3. As stated by the authors, although hypertension control rates slightly increased after RDN, BP levels remained disappointingly elevated3. These results are consistent with those of the 3-year follow-up of SPYRAL HTN-ON MED (Global Clinical Study of Renal Denervation With the Symplicity Spyral™ Multi-electrode Renal Denervation System in Patients With Uncontrolled Hypertension on Standard Medical Therapy), in which, in spite of RDN, antihypertensive therapy was not sufficient to achieve guideline-recommended BP targets11.
Third, a comparison with the sham-operated group was not feasible since 46% of patients in the sham group were crossed over to the RDN group within 36 months.
Fourth, the patients had no history of CV or cerebrovascular events, the mean estimated glomerular filtration rate (eGFR) was 86 ml/min/1.73m2 (none with an eGFR <60 ml/min/1.73m2), no one was diabetic, and only a small percentage (about 8%) had sleep apnoea. According to these data, the enrolled population was largely represented by individuals with a relatively low CV risk profile. Moreover, patients aged >75 years were excluded in order to minimise the potential confounding impact of isolated systolic hypertension and increased arterial stiffness. Although this choice can be considered an added value of the study, it implies a current limitation to extending clinical indications for RDN to elderly people.
Finally, patients and clinical staff were unblinded to group assignment after 6 months from randomisation, potentially influencing the long-term results of the study.
The results of RADIANCE-HTN SOLO3 and SPYRAL HTN-ON MED11 are reassuring with regard to long-term safety and the BP-lowering efficacy of RDN. They reinforce the emerging concept that RDN should be viewed as a “companion” to pharmacological treatment, with more compelling indications for patients with resistant hypertension, those who are non-adherent or intolerant to multiple antihypertensive drugs, or who express a firm and shared preference to undergo RDN.
Since the effects of RDN on the prevention of hypertension-mediated organ damage and reduction of major CV events have not been explored, the additional potential benefits of this procedure remain unanswered at this time. Further studies are necessary.
Conflict of interest statement
M. Volpe served as an advisor and steering committee member for Kalos Medical and as a collaborator through a Medtronic contract with the Department of Clinical and Molecular Medicine, Sapienza University of Rome. G. Gallo has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.