Abstract
Aims: Interventional cardiologists are exposed to substantial occupational ionising radiation. This study sought to investigate differences in radiation exposure in biplane versus monoplane coronary angiography and percutaneous coronary interventions (PCI).
Methods and results: RAMBO (RAdiation exposure in Monoplane versus Biplane cOronary angiography and interventions) was a prospective, randomised, two-arm, single-centre, open-label trial, enrolling a total of 430 patients undergoing coronary angiography. Patients were randomly assigned to biplane or monoplane imaging. The primary efficacy measure, the operator radiation dose at the level of the left arm as measured by a wearable electronic dosimeter, was significantly higher in the biplane as compared to the monoplane group (4 [1-13] µSv vs 2 [0-6.8] µSv, p<0.001). The dose area product was 11,955 (7,095-18,246) mGy*cm2 and 8,349 (5,851-14,159) mGy*cm2 in the biplane and the monoplane groups, respectively (p<0.001). While fluoroscopy time did not differ between the groups (p=0.89), the amount of contrast medium was lower with biplane as compared with monoplane imaging (p<0.001).
Conclusions: Biplane imaging for coronary angiography and PCI is related to an increased radiation exposure for the interventional cardiologist as compared with monoplane imaging. Monoplane imaging should be considered for advanced radioprotection in cardiac catheterisation, with biplane imaging used for selected cases only.
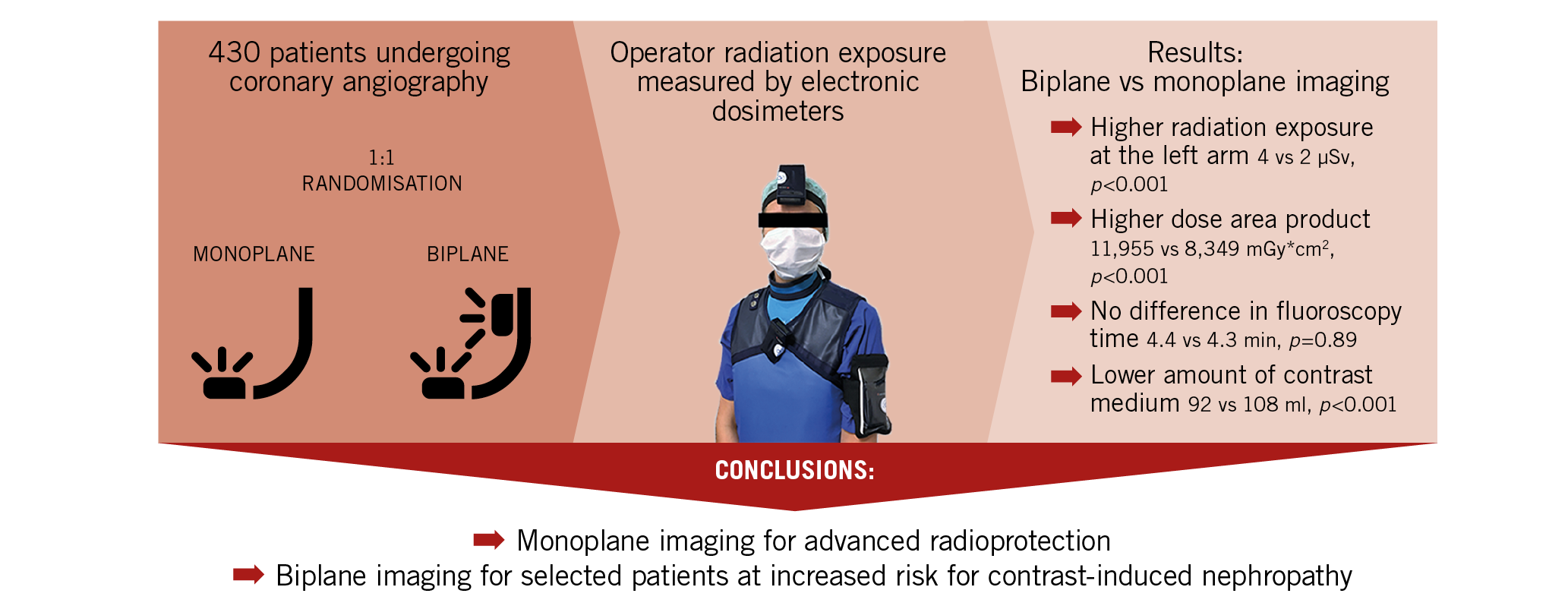
Visual summary. RAdiation exposure in Monoplane versus Biplane percutaneous cOronary angiography and interventions: the RAMBO trial.
Introduction
Interventional cardiologists are among the health professionals who are most exposed to occupational ionising radiation1,2,3. Exposure to ionising radiation is of particular concern given the related risk of cancer1,4. Recent reports on the increased risk of cataract, left-sided brain malignancies, thyroid disease, accelerated atherosclerosis, and chromosomal deoxyribonucleic acid (DNA) damage have further raised awareness of the occupational risk related to long-term low-dose ionising radiation during cardiac catheterisation5,6,7. Recognition of these occupational hazards has fuelled the search for advanced protective measures and refined radiation safety protocols to minimise radiation exposure during cardiac catheterisation. Scatter of radiation from the patient represents the main source of ionising radiation exposure to the staff performing angiography-guided cardiovascular procedures. Contemporary standards for radioprotection in cardiac catheterisation laboratories comprise upper ceiling leaded shields and table drapes among others, along with individual radioprotection measures including lead aprons, thyroid collars, and glasses. Further, procedure-related factors including image field size, beam collimation, frame rate, and tube angulation have been shown to be substantial determinants of the degree of radiation exposure to both patients and staff and are gaining more and more importance in the era of increasingly complex percutaneous coronary interventions (PCI)8,9,10.
Coronary angiography is performed by using either monoplane or biplane imaging. Monoplane imaging visualises the coronary arteries via a single X-ray source and detector. Biplane imaging uses two C-arms with a double monitoring system which allows a simultaneous visualisation of a coronary artery in two different planes. Biplane imaging is generally considered to bear the advantage of requiring a lower amount of contrast agent and of being more efficient, given the simultaneous orthogonal visualisation of the coronary arteries with a single contrast injection11,12. Whether the use of biplane in comparison to monoplane imaging for diagnostic coronary angiography and PCI affects radiation exposure remains ill-defined and randomised data are lacking.
The aim of this study was therefore to assess the radiation exposure of interventional cardiologists during coronary angiography and PCI with biplane versus monoplane imaging in a randomised design and using wearable electronic dosimeters. In addition, the impact of biplane versus monoplane imaging on procedural characteristics was investigated.
Material and methods
STUDY DESIGN
This prospective, randomised, two-arm, single-centre, open-label RAdiation exposure in Monoplane versus Biplane cOronary angiography and interventions (RAMBO) trial evaluated the individual operator and patient radiation exposure of biplane versus monoplane imaging during diagnostic coronary angiography and PCI. Patients were screened before coronary angiography and randomised in a 1:1 ratio to either biplane or monoplane coronary angiography. Randomisation was performed with the use of sealed, opaque envelopes. Prior to the procedure, personal electronic dosimeters (DMC 3000™; Mirion Technologies, Hamburg, Germany) were placed at the level of the upper left arm, the thorax (outside the lead apron), and the head (in the middle of the forehead). A fourth electronic dosimeter was placed on the angiographic table at the level of the patient’s head. The operators performed diagnostic coronary angiograms and PCI when indicated according to the assigned group.
For coronary angiography and PCI, the Philips Allura Xper FD10/10 biplane angiography system (Philips Healthcare, Amsterdam, the Netherlands) was used. All imaging parameters were kept static when switching between the monoplane and biplane set-up. All procedures were performed in line with current guidelines and using standard techniques without any study-related specifications13, besides the requirement to display the right coronary artery from at least two different projections and the left coronary artery from at least five different projections during coronary angiography. Lateral imaging with the right radial approach was performed with the right arm placed alongside the body and the left arm placed above the head. Diagnostic procedures were performed with 5 Fr diagnostic catheters, and PCI with 6 Fr guiding catheters. Contrast medium was injected using the ACIST CVi™ system (ACIST Europe B.V., Heerlen, the Netherlands). According to the standards of the centre, the field of view used was 20 cm, the image frame rate was 7.5 images/second, and maximal collimation was performed throughout the procedures. Standard radiation protection comprised a ceiling-mounted upper body leaded shield and a lower body table drape attached to the side of the operating table, and each operator wore a lead apron, a thyroid collar, and glasses with a lead equivalent of 0.75 mm Pb. The use of an additional radiation protection drape (Protection Cover MaxLite™, 120×80 cm, 0.25 mm Pb; UniRay Medical LLP, Navi Mumbai, India) was left to the discretion of the operator.
The protocol was approved by the ethics committee (EA1/109/18), and written informed consent was obtained from all operators and patients participating in the study. The study was conducted in full conformity with the principles of the Declaration of Helsinki, and in accordance with local law and regulations. This trial is registered with the German Registry of Clinical Studies (DRKS00014907).
STUDY POPULATION
A total of 430 patients who underwent coronary angiography for suspected coronary artery disease at our institution between August 2018 and April 2019 were enrolled in the study. Procedures were performed by 14 expert operators. Patients were eligible if they were between 18 and 85 years old, were scheduled for clinically indicated coronary angiography, and were able and willing to give written informed consent. Exclusion criteria comprised referral for targeted PCI, emergency coronary angiography, haemodynamic instability, prior coronary artery bypass grafting, renal failure (defined as an estimated glomerular filtration rate ≤45 ml/min), and any psychiatric disorders in need of therapy.
The intention-to-treat population comprised 430 patients who underwent coronary angiography and were randomised to either the biplane or the monoplane study arm. The per-protocol population included 388 (90.2%) patients who underwent coronary angiography and completed the procedure according to the study protocol and in the assigned study arm (Figure 1). Study protocol deviations were due to non-adherence of the operators to the required minimal number of projections due to emergency situations in daily clinical practice.
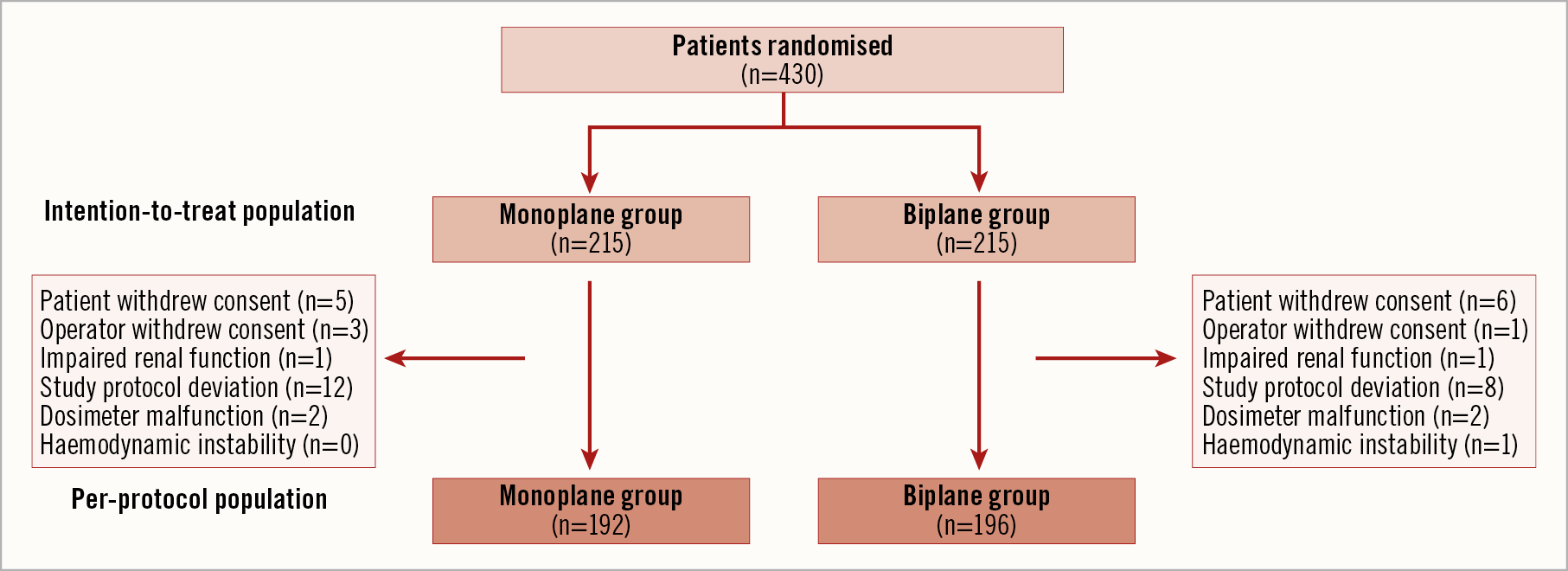
Figure 1. Study flow chart.
MEASUREMENT OF RADIATION EXPOSURE
Real-time radiation exposure was measured by wearable electronic dosimeters (DMC 3000; Mirion Technologies) calibrated in Hp(10) terms with a measurement range from 1 µSv to 10 Sv and from 0.1 µSv/h to 20 Sv/h. The radiation dose was directly recorded from the screen at the end of each procedure and was reset afterwards. Fluoroscopy time (minutes) and dose area product (mGy*cm2) were measured by the angiography system. All radiation measures were recorded after diagnostic angiography and when PCI was performed additionally at the end of the procedure.
EFFICACY MEASURES
The primary efficacy measure was the operator radiation dose at the level of the left arm. Secondary efficacy measures at the operator level included radiation doses at the level of the head and thorax, and peak radiation dose rates at the level of the left arm, the head, and the thorax. Secondary efficacy measures at the patient level included both radiation dose and peak radiation dose rate at the level of the head. Secondary efficacy measures also comprised dose area product, fluoroscopy time, and amount of contrast medium used.
STATISTICAL ANALYSIS
Continuous variables are presented as mean and standard deviation or median and interquartile range as appropriate, and categorical variables as count and frequency. The Shapiro-Wilk test was used to test whether a parameter followed a normal distribution. The Mann-Whitney U test was used for comparisons of continuous variables, and Pearson’s χ² test or Fisher’s exact test for comparisons of categorical variables. Correlations between two variables were specified by the Spearman’s rank correlation coefficient. Primary and secondary efficacy analyses were performed on the per-protocol population as pre-specified and were repeated on the intention-to-treat population. A pre-specified subgroup analysis comprised patients undergoing diagnostic coronary angiography only. Binary logistic regression models were applied to estimate unadjusted and adjusted risks of increased radiation exposure (≥median operator radiation dose at the upper left arm) in both the biplane and monoplane groups. Models were adjusted for baseline variables significantly associated with increased radiation exposure (>median operator radiation dose at the upper left arm) in univariate analysis with p-values <0.05. All testing was two-sided and conducted at the 0.05 significance level. Statistical analyses were performed using SPSS, Version 24 (IBM Corp., Armonk, NY, USA).
SAMPLE SIZE ESTIMATION
Sample size was based on the primary efficacy measure14,15,16. Radiation doses of 9 µSv in the biplane and 8 µSv in the monoplane group with a standard deviation of 3.5 µSv were assumed. Based on a two-sided alpha level of 0.05, a total of 192 patients were needed in each group for the study to have a power of at least 80%. Anticipating a 10% drop-out rate, 215 patients were randomised per group. A total of 430 patients were therefore included in the study.
Results
PATIENT AND PROCEDURAL CHARACTERISTICS
Baseline clinical characteristics are summarised in Table 1. Percutaneous coronary intervention during the index procedure was performed in 85 (21.9%) patients. The use of angiographic projections in the biplane and the monoplane groups is summarised in Supplementary Table 1. The median number of procedures performed per operator was 22 (9-47).
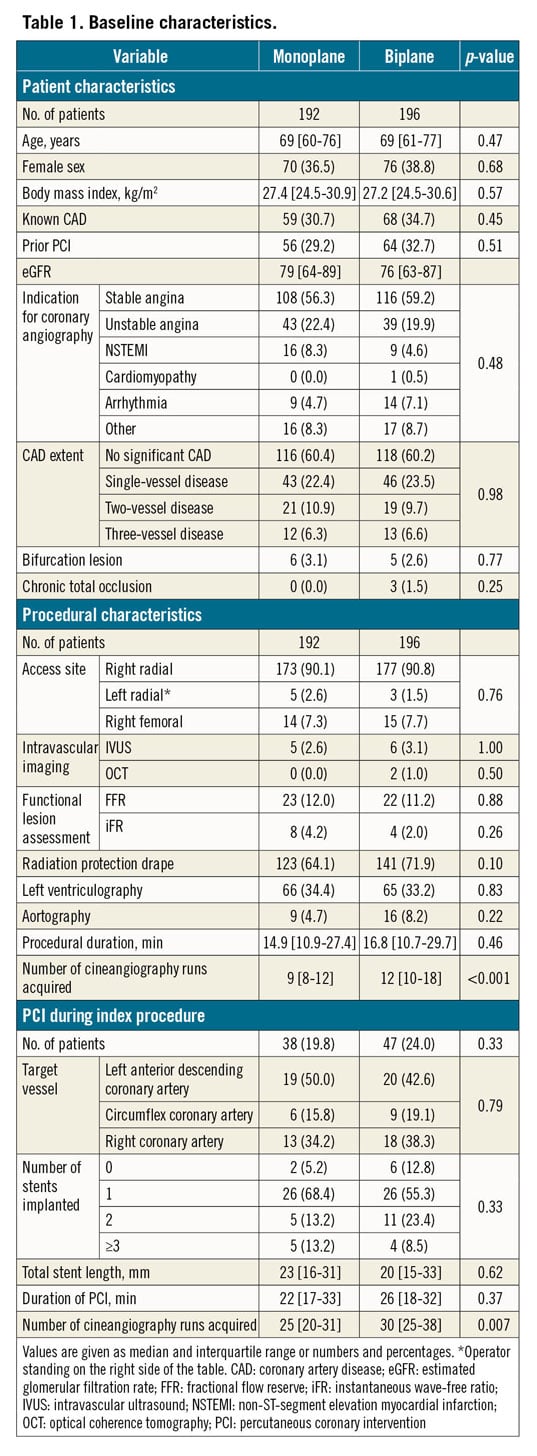
The number of cineangiography runs was numerically higher in patients with as compared to those without three-vessel disease (10 [7-19] vs 8 [6-11], p=0.09), and higher in patients with as compared to those without bifurcation lesions (25 [21-35] vs 8 [6-11], p<0.001). The number of cineangiography runs correlated significantly with the number of stents placed (r=0.70, p<0.001), and was higher in patients treated with ≥2 stents (35 [29-41]) as compared to those treated with 1 stent (25 [21-29], p<0.001).
EFFICACY RESULTS
The primary efficacy measure, the operator radiation dose at the level of the left arm, was significantly higher in the biplane as compared to the monoplane group (4 [1-13] µSv vs 2 [0-7] µSv, p<0.001) (Table 2, Figure 2). Corresponding rates in the intention-to-treat population were 4 [1-14] µSv and 2 [1-7] µSv (p<0.001).
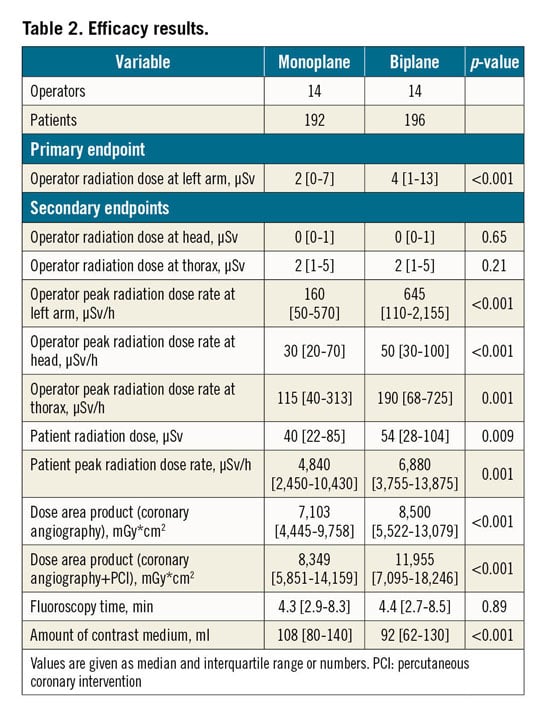
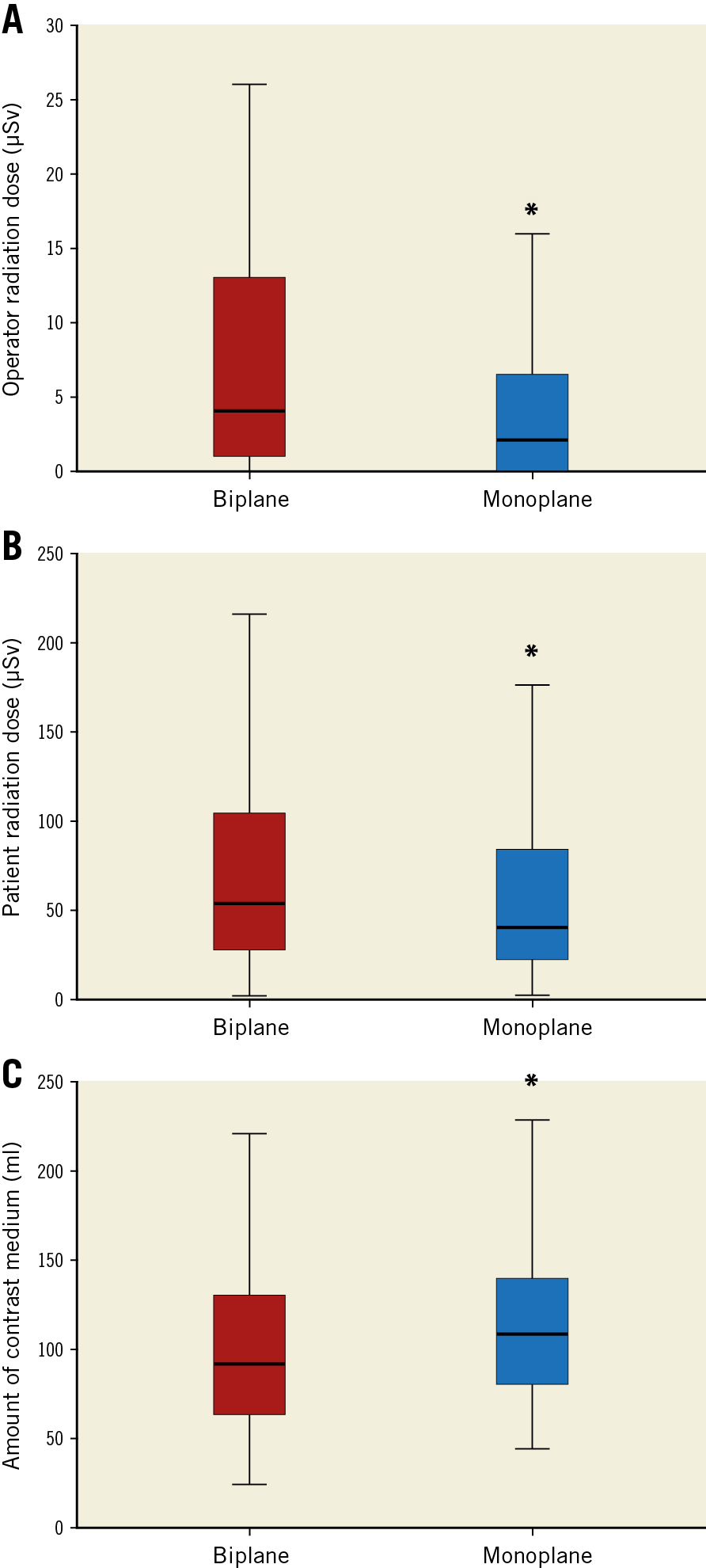
Figure 2. Radiation dose in biplane versus monoplane imaging. A) Operator radiation dose at the level of the left arm in biplane (red) and monoplane (blue) imaging. B) Patient radiation dose at the level of the head in biplane (red) and monoplane (blue) imaging. C) Amount of contrast medium in biplane (red) and monoplane (blue) imaging.
Secondary efficacy measures included measurements of radiation exposure at the operator and the patient level. At the operator level, peak radiation dose rates at the level of the left arm (p<0.001), head (p<0.001), and thorax (p=0.001) were significantly higher in the biplane as compared with the monoplane group. At the patient level, radiation dose at the level of the head (p=0.009) and peak radiation dose rate (p=0.001) were significantly higher in the biplane as compared with the monoplane group. The dose area product was higher in the biplane group (p<0.001). Patient radiation dose correlated significantly with the dose area product (r=0.84, p<0.001). The amount of contrast medium used was lower in the biplane as compared with the monoplane group (92 [62-130] ml vs 108 [80-140] ml, p<0.001). Results were confirmed in the intention-to-treat population.
In a pre-specified subgroup analysis including patients undergoing diagnostic coronary angiography only, radiation dose at the level of the left arm was significantly higher in the biplane as compared with the monoplane group (p=0.004), with similar trends observed in patients undergoing PCI (p=0.10) (Supplementary Table 2).
PREDICTORS OF INCREASED RADIATION DOSE
Independent predictors of increased operator radiation dose at the level of the left arm (≥median) in both the biplane and monoplane groups are summarised in Supplementary Table 3.
Discussion
This study demonstrated for the first time that biplane imaging for coronary angiography and PCI was related to an increased radiation exposure for the interventional cardiologist. Radiation exposure to the patient was also higher in biplane as compared with monoplane imaging, while procedural duration and fluoroscopy time did not differ between the groups. Further, biplane imaging was associated with a lower amount of contrast medium used.
PROCEDURAL CHARACTERISTICS OF BIPLANE VERSUS MONOPLANE IMAGING
While procedural duration was similar between the groups, the number of cineangiography runs was significantly higher in biplane imaging, and the selection of the angiographic projections differed between the biplane and monoplane groups. These findings demonstrate that the availability of two X-ray sources and detectors in biplane imaging substantially affects the number of acquisitions and the selection of the angiographic projections. We can only speculate about the reasons underlying this observation. Per additional projection needed, mostly two angiograms were acquired on biplane imaging while only one was acquired on monoplane imaging, which at least in part contributes to the increased number of cineangiography runs acquired with biplane imaging. Further, optimal projections may be more difficult to obtain with two C-arms in biplane imaging systems.
The use of advanced invasive diagnostic testing by fractional flow reserve and intracoronary imaging is in line with previously reported data and did not differ between the groups17,18. Left ventriculography was performed in about one third of patients, particularly when echocardiography was not available at the time of coronary angiography.
The contrast load was reduced by 15% with biplane imaging. This observation is in line with previous observational studies reporting a 5% to 40% reduction in the amount of contrast medium used with biplane imaging11,12,19,20. Therefore, biplane imaging seems to be particularly well suited for patients at increased risk of contrast-induced nephropathy21.
RADIATION EXPOSURE OF BIPLANE VERSUS MONOPLANE IMAGING
To the best of our knowledge, this is the first randomised study showing that biplane imaging for coronary angiography and PCI was related to an increased radiation exposure for the interventional cardiologist. These findings were confirmed by higher peak radiation dose rates measured at the left arm, head, and thorax with biplane imaging and in a sensitivity analysis including only patients undergoing diagnostic coronary angiography. Consistently, patient radiation exposure was increased by 35% in biplane imaging, and the dose area product by 19%. These results are in line with previous studies which suggested an increased radiation exposure with biplane imaging. Although over 10,000 patients have so far been included in studies on radiation exposure in biplane versus monoplane imaging, analyses were limited by the observational design and the measurement of the dose area product only12,19,20,22,23,24. While Smith et al observed a 23% increase of the dose area product with biplane as compared with monoplane imaging12, Grech et al reported an increase of over 70% when biplane imaging was used19. In line with previous studies8,16,23,25, the need for PCI, lateral angulation, and left ventricular angiography emerged as independent predictors of increased radiation exposure with biplane imaging, while the use of an additional radiation protection drape was protective. The use of adjunctive protective drapes emerged as an independent predictor of reduced radiation exposure in the biplane but not in the monoplane group. The more frequent use of the lateral tube angulation in the biplane group, causing an increased amount of scatter radiation8,26, may explain a more pronounced radiation protection achieved by adjunctive protective drapes in biplane imaging.
As the left upper arm of the operator is closest to the X-ray system and therefore represents the part of the body with the highest radiation exposure, lying directly within the radiation path, the operator radiation exposure at the level of the left arm was defined as the primary endpoint. The overall observed operator radiation exposure is comparable with previously reported data16; higher levels might be expected in a real-world setting.
Since substantial concern has been raised on the adverse effects of long-term low-dose radiation related to interventional cardiovascular procedures5,6,7, radiation safety in cardiac catheterisation has gained further importance, technical refinements to the X-ray systems have been implemented to reduce radiation exposure, and the efficacy of adjunctive protective drapes has been proven in different studies27,28,29. The enhanced knowledge of specific characteristics related to biplane and monoplane imaging, particularly in terms of radiation exposure and the amount of contrast agent used, helps to select optimal technical settings for each individual patient and, at the same time, helps to minimise patient and operator radiation hazards effectively in invasive cardiology. The findings of this study advance our understanding of radiation safety in cardiac catheterisation, and strongly support the use of monoplane imaging, with both lateral angulations and ventricular angiography restricted to selected cases. Given the possibility to visualise lesion segments in two different planes simultaneously and the lower amount of contrast agent used, biplane imaging systems, although they have higher installation and maintenance costs, are considered to have particular advantages over monoplane systems in selected patients such as those undergoing complex interventions for bifurcation lesions or chronic total occlusions, as well as those with pre-existing kidney disease, diabetes, congestive heart failure, or older age at increased risk for contrast-induced nephropathy11,21,30.
Limitations
A few limitations need to be considered. First, the study is limited by the single-centre design. However, the number of expert operators involved in the study is comparable to other trials in this field9. Second, as only duration of PCI, total number of stents implanted, and total stent length were recorded as surrogates for procedural complexity, differences in the extent and severity of coronary artery disease may have affected the results. Third, given the high proportion of transradial procedures in the study, comparison between different access sites was precluded. Further, the selection of the angiographic projections and angulations was left to the discretion of the operator, i.e., a design which allowed achieving optimal image quality with minimal foreshortening and overlap and at the same time the investigation of the impact of biplane versus monoplane imaging on the course of the procedure in a randomised design. We can, however, not completely exclude the possibility that differences in the individual angiographic projections selected may have introduced some bias.
Conclusions
These results demonstrate that biplane imaging results in a substantially higher radiation exposure to the interventional cardiologist as compared with monoplane imaging. The study therefore supports the use of monoplane imaging for advanced radioprotection in contemporary cardiac catheterisation, with biplane imaging used for selected patients only, particularly those at increased risk for contrast-induced nephropathy.
|
Impact on daily practice Biplane imaging for coronary angiography and percutaneous coronary intervention is related to an increased radiation exposure for the interventional cardiologist as compared with monoplane imaging. Monoplane imaging should therefore be considered for advanced radioprotection in cardiac catheterisation, with biplane imaging used for selected cases at increased risk for contrast-induced nephropathy. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.