Abstract
Background: Percutaneous coronary intervention (PCI) is indispensable in cardiology; however, exposure to potentially harmful ionising radiation remains a concern.
Aims: This study was designed to assess the PCI-related radiation dose over the last decade and to identify predictors of increased dose exposure.
Methods: The PROcedural radiaTion dose Exposure in percutaneous Coronary intervenTION (PROTECTION VIII) study included all PCIs reported to a German quality assurance programme between 2008 and 2018. Dose area product (DAP) and radiation time were analysed. Effective dose (ED) was estimated (ED=DAP*k; conversion coefficient k=0.0022 mSv/cGy*cm2). Multivariate linear regression analysis was used to identify predictors associated with a clinically relevant increase of radiation dose (ED ≥1 mSv).
Results: We enrolled 3,704,986 patients undergoing PCI (median age 70 years, 30% female). Indications were chronic coronary syndrome (37.5%), unstable angina pectoris and non-ST-segment elevation myocardial infarction (non-STEMI; 33.2%) and STEMI (18.5%). Median DAP was 4,203 (interquartile range [IQR] 2,313-7,300) cGy*cm, ED was 9.2 mSv and median radiation time was 9.2 (IQR 5.8-15.0) min. Within the 10-year period, radiation exposure was reduced by 36% (p<0.001) and resulted in a median DAP of 3,070 cGy*cm (ED 6.8 mSv) in 2018. A significant 5.3-fold variability of median DAP was observed between catheterisation laboratories (p<0.001). We identified patient-related (gender, coronary artery bypass graft surgery, heart failure) and procedure-related (coronary occlusion PCI, ostial lesion PCI, left main PCI, multivessel PCI) predictors of increased radiation dose (all p<0.001).
Conclusions: This radiation dose survey demonstrates a considerable reduction of PCI radiation exposure during the last decade. However, large variability between catheterisation laboratories underlines the need for further radiation dose reduction.
Introduction
Percutaneous coronary intervention (PCI) is the guideline-recommended first-line therapy for coronary revascularisation in patients with acute coronary syndrome and obstructive coronary artery disease (CAD)12. Furthermore, PCI is an important therapeutic strategy in patients with symptomatic chronic coronary syndrome and haemodynamically relevant obstructive CAD34. The downside of cardiac catheterisation procedures is the potentially harmful exposure to ionising radiation. Detrimental effects include the development of malignancies, skin damage, inheritable defects, cataract formation and pregnancy complications5678. The risk of radiation-induced cancer presumably increases in direct proportion to effective dose, since it is believed that the stochastic effects of ionising radiation follow a non-threshold, radiation-dependent risk model9. In the recently performed PROTECTION VII study, radiation dose exposure of diagnostic cardiac catheterisation in current clinical practice was analysed and considerable dose reduction during the last decade was reported10. Importantly, radiation exposure in PCI is higher and clinically more relevant when compared to diagnostic catheterisation only. Furthermore, the indications and complexity of PCI procedures have increased in recent years. At the same time, the awareness of radiation safety and the development of radiation dose reduction techniques have improved.
Consequently, the actual amount of radiation dose exposure in current clinical routine and the change in radiation dose during recent years are of great interest for both the interventional cardiologists and the patients undergoing PCI. However, only radiation dose data from small studies with limited patient numbers are currently available1112131415.
Therefore, the PROcedural radiaTion dose Exposure in percutaneous Coronary intervenTION (PROTECTION VIII) study was designed to (i) examine the current level of radiation dose, (ii) assess the development of radiation dose during the last decade, and (iii) identify independent predictors of a clinically relevant increase in PCI radiation dose in a large-scale patient cohort. We used data from a nationwide quality assurance programme in Germany allowing a comprehensive and representative assessment of PCI-related radiation dose.
Methods
Study protocol
In this investigator-initiated, nationwide, multicentre, retrospective study all PCI procedures after diagnostic invasive coronary angiography that were reported to the quality assurance programme for cardiac catheterisation and PCI in Germany between 2008 and 2018 were included. Data were collected, hosted and organised by the aQua institute (Institut für angewandte Qualitätsförderung und Forschung im Gesundheitswesen; 2008-2013) and the IQTiG institute (Institut für Qualitätssicherung und Transparenz im Gesundheitswesen; 2014-2018). Participation in the quality assurance programme is mandatory for all catheterisation laboratories and complete data collection for patients with public health insurance is assured, as it has been linked to PCI reimbursement. All patients undergoing diagnostic catheterisation and subsequent PCI in one setting between 2008 and 2018 were included in the PROTECTION VIII study. Data collection of the quality assurance programme was amended in 2017 and additional PCI-related parameters were collected by the IQTiG institute from that time on. Therefore, a more detailed analysis of PCI radiation dose was performed in the subgroup of patients who were treated in 2017 and 2018. Data analysis was facilitated by the quality assurance procedure of the Federal Joint Committee (Gemeinsamer Bundesausschuss [G-BA]) in accordance with Article 136 of the German Social Code Book V. The PROTECTION VIII study has been approved by and received ethical oversight from the Federal Joint Committee (G-BA), which is the highest decision-making body of the joint self-government of physicians in Germany (application number 2019-19/06).
Radiation dose measures
The primary outcome parameters for the current analysis were (i) the radiation dose area product (DAP, in cGy*cm2), and (ii) the total radiation time (min.). The DAP was available from 2008 to 2018, and the radiation time from 2008 to 2014 (radiation time was not collected by the IQTiG institute after 2014). Both variables summarise the radiation data for both fluoroscopy and digital cine angiography. The DAP measures the stochastic effects of ionising radiation and has been described as a useful variable characterising the patient radiation exposure during catheterisation procedures8. Data were analysed on a patient level and a site level. The effective dose (ED) during PCI was estimated from the product of the DAP and a conversion coefficient k for the chest. This conversion coefficient (k=0.0022 mSv/cGy*cm2, averaged between male and female models) was evaluated from organ dose conversion coefficients given for an average of typical projections in cardiac angiography16, and interpolated for radiation qualities applied in the present study. This value is in reasonable agreement with respective conversion coefficients for various chest posteroanterior (PA) projections17. The variability in median DAP between study sites and the multivariate regression analysis were performed in the detailed PCI patient cohort that was available in 2017 and 2018. In the analysis of dose variability between participating catheterisation laboratories, we included all sites that performed at least 25 PCI procedures and further excluded 2.5% of catheterisation laboratories with very low and 2.5% of catheterisation laboratories with very high median DAPs to accommodate for outliers beyond a 95% confidence interval.
Statistical analysis
Variables are expressed as counts with percentages or medians with interquartile ranges (IQRs). Comparison of groups was performed with the Wilcoxon Mann-Whitney U test or chi² test as appropriate. Comparison of multiple groups was performed using the Kruskal-Wallis test and Dunn’s (1964) Kruskal-Wallis multiple comparison test. P-values were adjusted with the Bonferroni method. Trend analysis was performed using the Bartels test for randomness. Univariate and multivariate linear regression analyses were performed to identify predictors significantly associated with radiation dose. Here, the significance level for a clinically relevant change in radiation dose was set to ED ≥1 mSv. A p-value <0.05 was considered to be statistically significant. Statistical analysis was performed using R Version 1.1.383 (R Foundation for Statistical Computing).
Results
Patient and procedural characteristics of PCI
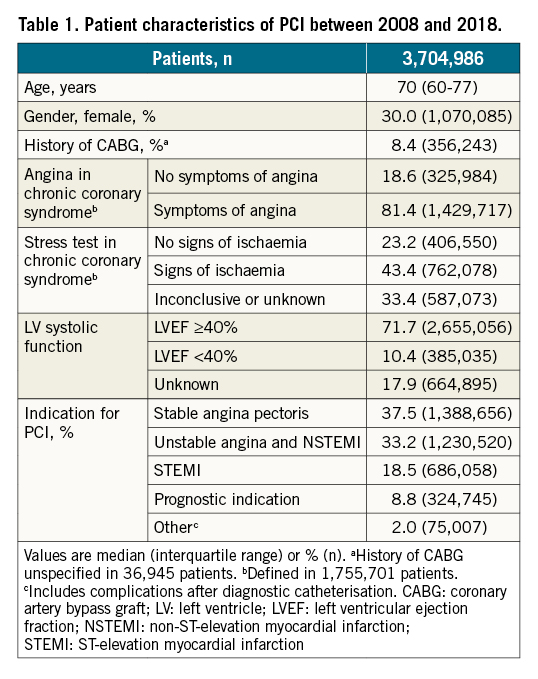
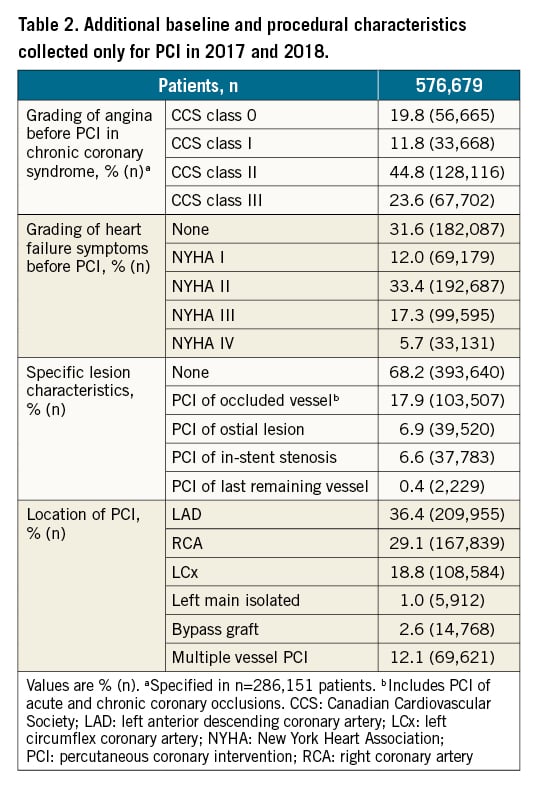
A total of 3,704,989 PCI procedures performed in Germany between 2008 and 2018 were included in the current analysis. The number of catheterisation laboratories enrolling patients into the PROTECTION VIII study increased from 611 in 2008 to 860 in 2018. All available patient characteristics for patients treated between 2008 and 2018 are summarised in Table 1. Patients were 70 (IQR 60-77) years old and 30.0% were female. A history of coronary artery bypass graft (CABG) surgery was reported for 8.4% of patients. In patients presenting with a chronic coronary syndrome, the majority (81.4%) reported angina pectoris. Signs of myocardial ischaemia were observed in 43.4% of patients with chronic coronary syndrome, as detected by non-invasive myocardial stress testing, while test results were unknown or inconclusive in 33.4% of cases. Reduced left ventricular ejection fraction (LVEF) below 40% was reported for 10.4% of patients. The most frequent indication for PCI was stable angina pectoris in 37.5%, followed by unstable angina pectoris and NSTEMI in 33.2%, and STEMI in 18.5% of patients. Additional baseline and procedural characteristics were available for a subgroup of 576,679 patients undergoing PCI in 2017 and 2018 (Table 2). The above-mentioned patient characteristics of this subgroup were comparable to the complete study cohort from 2008 to 2018 (Supplementary Table 1). For the 2017/2018 subgroup, signs of heart failure were reported in 68.4% of patients that were most frequently attributed to New York Heart Association (NYHA) Functional Class II (Table 2). PCI for coronary artery occlusion was performed in 17.9% of patients. PCI of ostial lesions and in-stent-restenosis was performed in 6.9% and 6.6%, respectively. The most frequent coronary artery targeted by PCI was the left anterior descending coronary artery (LAD) in 36.4% of patients, followed by the right coronary artery (RCA; 29.1%) and the left circumflex coronary artery (LCx; 18.8%). Isolated PCI of the left main artery (LMA) was performed in 1.0% of procedures. Isolated bypass graft PCI was performed in 2.6% and multivessel PCI was performed in 12.1% of patients.
Change of radiation dose exposure and variability between cardiac catheterisation laboratories
The median DAP of all 3,704,989 PCIs between 2008 and 2018 was 4,203 (IQR 2,313-7,300) cGy*cm2. This radiation exposure translates into a median estimated ED of 9.2 (IQR 5.1-16.1) mSv. The associated median radiation time that was reported between 2008 and 2014 and was 9.2 (IQR 5.8-15.0) min. During the ten-year observational period, the median DAP associated with PCI was significantly reduced (p<0.001 in trend analysis and multiple group testing) (Central illustration, panel A). In 2008, the median DAP of 267,451 PCIs was 4,811 (IQR 2,530-8,394) cGy*cm2. Ten years later, the median DAP had decreased by 36% to 3,070 (IQR 1,722-5,299) cGy*cm2, with an estimated ED of 6.7 (IQR 3.8-11.7) mSv as assessed in 285,066 PCIs (p<0.001). In contrast, the median radiation time increased slightly during the observational period (Central illustration, panel B). In 2008, the median radiation time was 8.8 (IQR 5.5-14.3) min and increased by 11% to 9.8 (IQR 6.1-15.7) min in 2014 (Central illustration, panel B; p<0.001). A total of 747 catheterisation laboratories that performed at least 25 PCI procedures in 2017 and 2018 were listed in ascending order according to their median DAP (Central illustration, panel C). In the subsequent variability analysis, we included all sites within a 95% confidence interval (710 catheterisation laboratories), and thus, sites with a median DAP below the 2.5 percentile and above the 97.5 percentile were excluded (37 catheterisation laboratories) (Central illustration, panel C, red area). We observed a significant 5.3-fold variability between the catheterisation laboratories with the lowest median DAP (1,137 cGy*cm2) and highest median DAP within this 95% confidence interval (5,997 cGy*cm2; p<0.001) (Central illustration, panel C). The median number of PCIs performed in catheterisation laboratories within the 95% DAP confidence interval of the 2017/2018 dataset was 641 (IQR 238 to 1,103) PCIs. We stratified institutions within the 95% DAP confidence interval of the 2017/2018 dataset into low volume (<238 PCIs in 2017 and 2018), moderate volume (238 to 1,103 PCIs in 2017 and 2018) and high volume (>1,103 PCIs in 2017 and 2018) catheterisation laboratories (Central illustration, panel D). High-volume sites were associated with higher median DAP (3,458 cGy*cm2), when compared to moderate- (2,944 cGy*cm2) or low-volume sites (2,580 cGy*cm2; p<0.001) (Central illustration, panel D). However, the intersite variability of radiation dose was similar between high-volume (significant 5.0-fold variability) and low-volume sites (significant 5.2-fold variability; both p<0.001) (Supplementary Figure 1).
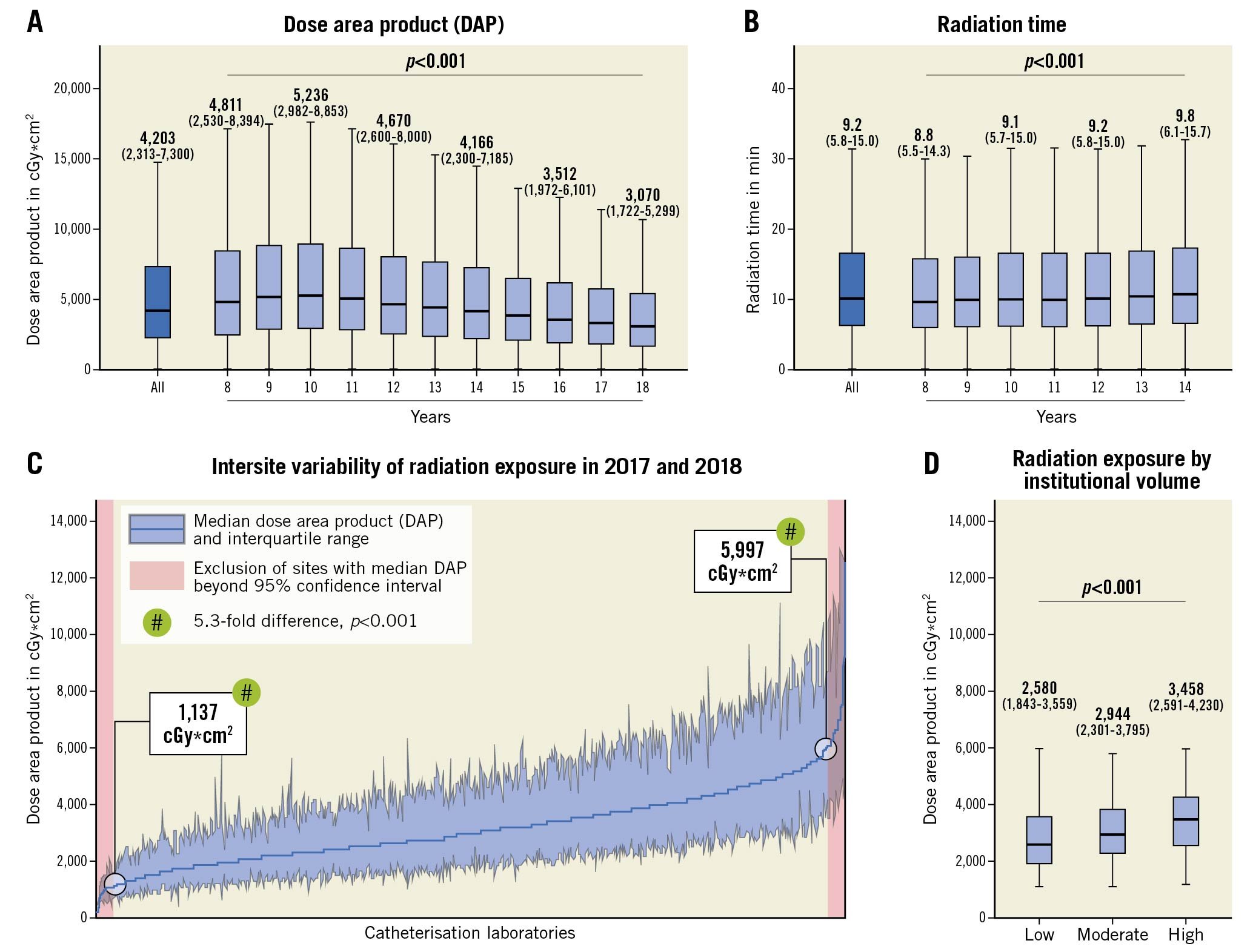
Central illustration. Trends of radiation dose exposure in PCI. A) DAP of all PCI procedures (left) and by year between 2008 and 2018 (right). B) Radiation time of all PCI procedures (left) and by year between 2008 and 2018 (right). C) Variability of DAP in the 2017/2018 PCI group between catheterisation laboratories in Germany. Lines demonstrate median, filled area represents IQR. For accommodation of outliers in the registration of DAP, only study sites with a median DAP within the 95% confidence interval were compared and outliers (red area) were excluded. D) DAP by institutional volume. All catheterisation laboratories with a median DAP within the 95% confidence interval were stratified according to the number of PCIs in 2017/2018 into low volume (institutional volume <1st quartile: 25-238 PCIs), moderate volume (IQR of institutional volume: 238-1,103 PCIs) and high volume (institutional volume >3rd quartile: >1,033 PCIs). Box plots show median (middle horizontal line), IQR (box), and the range of non-outlying data points (lower whisker: lowest data point within the 25th percentile minus 1.5 times IQR; upper whisker: highest data point within the 75th percentile plus 1.5 times IQR). DAP: dose area product; IQR: interquartile range; PCI: percutaneous coronary intervention
Radiation dose exposure in subgroups of PCI
Different indications for PCI were associated with small differences of radiation dose exposure (Supplementary Table 2). Stable angina pectoris was associated with the lowest median DAP of 3,075 cGy*cm2 and ED of 6.8 mSv. In contrast, acute coronary syndrome due to unstable angina or NSTEMI was associated with the highest median DAP of 3,309 cGy*cm2 and ED of 7.3 mSv. Several patient-related factors were associated with differences in radiation dose exposure during PCI (Figure 1A). Male gender was associated with 38% increased DAP during PCI when compared to female patients (p<0.001). PCI in patients with a history of CABG surgery was associated with a 32% increase in DAP, when compared to patients with native coronary arteries (p<0.001). PCI in patients with heart failure was associated with increased DAP. Accordingly, DAP was increased by 2% (NYHA Class I), 9% (NYHA Class II), 22% (NYHA Class III) or 34% (NYHA Class IV), when compared to patients without symptoms of heart failure (all p<0.001). Furthermore, the characteristic of the coronary artery lesion undergoing PCI was significantly associated with radiation dose (Figure 1B). PCI of an occluded coronary artery was associated with a 25% increase in DAP when compared to PCI of a non-occluded coronary artery (p<0.001). An ostial lesion led to a 27% increase of DAP when compared to PCI of a non-ostial coronary artery lesion (p<0.001). Finally, the coronary artery itself as well as multivessel PCI were associated with significant differences of radiation dose exposure during PCI (Figure 1B).
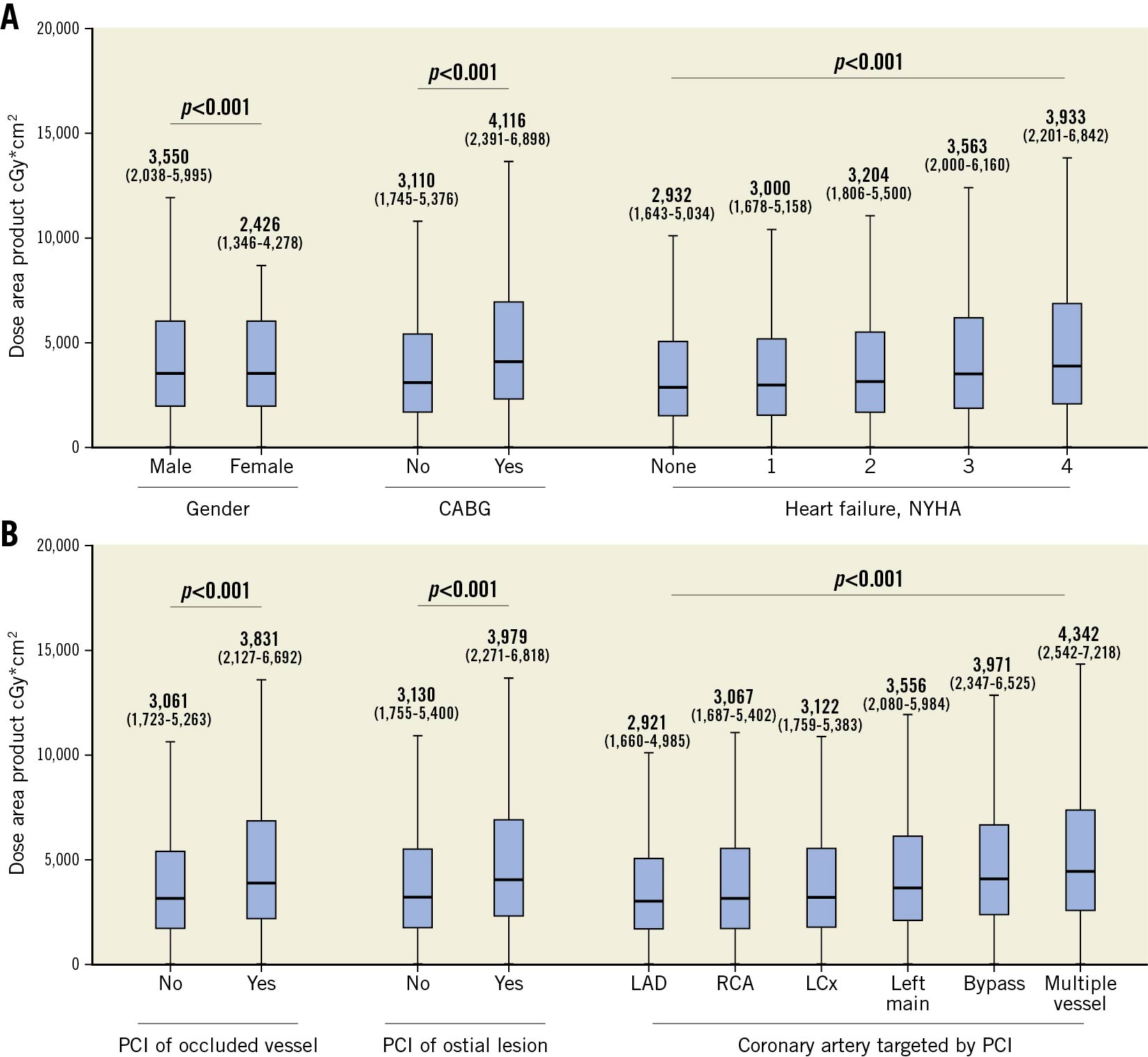
Figure 1. Radiation exposure of PCI by patient-related and procedure-related characteristics. A) Patient-related differences of DAP by gender (left), CABG history (middle), and heart failure (right). B) Differences of DAP in relation to PCI of occluded coronary artery (left), PCI of ostial lesion (middle), and the coronary artery undergoing PCI (right). Box plots show median (middle horizontal line), IQR (box), and the range of non-outlying data points (lower whisker: lowest data point within the 25th percentile minus 1.5 times IQR; upper whisker: highest data point within the 75th percentile plus 1.5 times IQR). CABG: coronary artery bypass grafting; CAD: coronary artery disease; DAP: dose area product; LAD: left anterior descending coronary artery; LCx: left circumflex coronary artery; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; RCA: right coronary artery
Independent predictors for radiation dose exposure in PCI
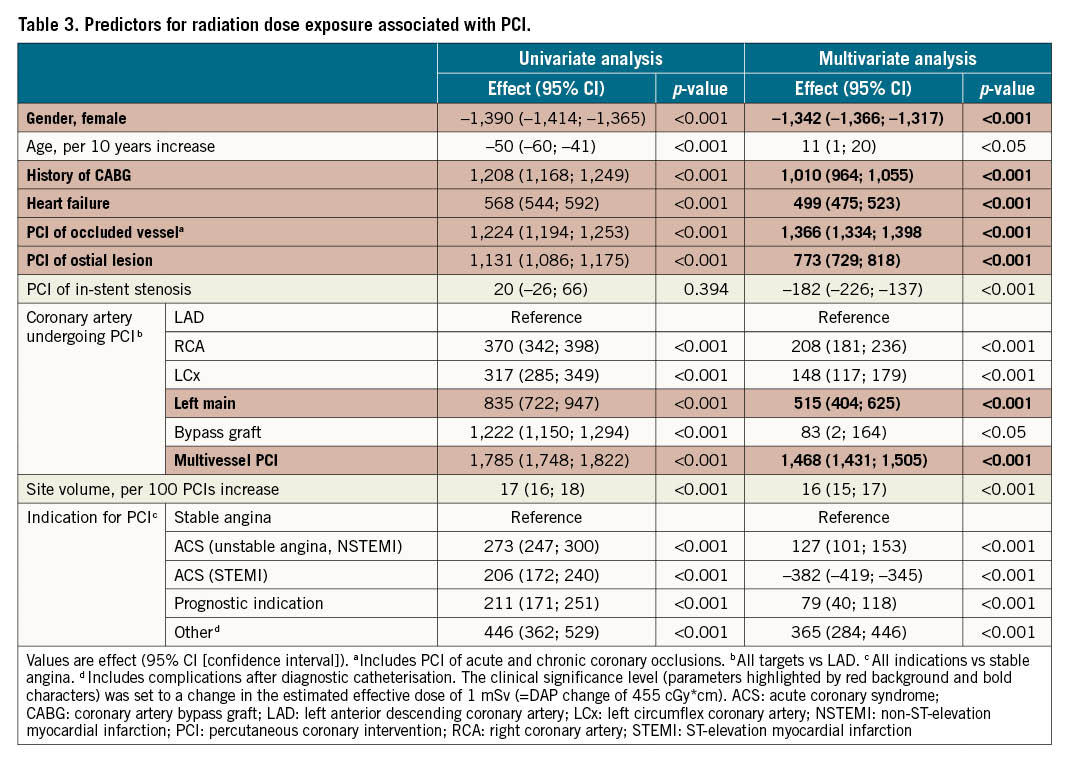
All available patient and procedural details of PCI in 2017 and 2018 were included in a multivariate regression analysis. Due to the large size of the dataset, almost all variables were identified as statistically significant predictors associated with radiation dose (Table 3). Thus, the level for clinical significance was set to an estimated effective dose of at least 1 mSv, which corresponds to an absolute DAP effect of 455 cGy*cm2. In the multivariate model, independent and clinically significant predictors for increased radiation dose exposure in PCI were male gender (+1,342 cGy*cm2), CABG (+1,010 cGy*cm2), heart failure (+499 cGy*cm2), PCI of an occluded vessel (+1,366 cGy*cm2), PCI of an ostial lesion (+773 cGy*cm2), PCI of the left main coronary artery (+515 cGy*cm2), and multivessel PCI (+1,468 cGy*cm2) (Table 3, highlighted in red, all p<0.001).
Discussion
PCI has emerged as an indispensable tool in cardiology that is frequently performed in patients with acute and chronic coronary syndromes. Exposure to potentially harmful radiation is an important safety aspect associated with PCI and is increasingly recognised by both patients and cardiologists. This results from (i) the growing evidence of radiation-related complications that increase with the level of radiation dose exposure, and (ii) the accelerating complexity of PCI procedures that are associated with increased radiation dose. However, evidence regarding the actual level of radiation dose exposure during clinical routine is scarce and results from large radiation dose surveys are lacking. Our study includes over 3.7 million patients undergoing PCI after diagnostic catheterisation and is the largest radiation dose survey of PCI practice to date. The study was designed on the basis of a nationwide quality assurance programme in Germany allowing for a complete, robust and representative assessment of radiation dose parameters in clinical routine PCI.
We demonstrated a significant reduction of PCI radiation dose exposure by 36% during the last decade (p<0.001), resulting in a median DAP of 3,070 cGy*cm2 and estimated ED of 6.7 mSv in the year 2018. This reduction of radiation dose was achieved despite the increasing complexity of PCI procedures as suggested by the increase of radiation time observed between 2008 and 2014. In the PROTECTION VIII study, a detailed procedural characterisation was available only in the last years of data acquisition and, thus, the development of the procedural complexity cannot be directly extracted from the presented results. However, procedures associated with increased radiation dose such as left main PCI and chronic total occlusion PCI were supported by recent guideline recommendations and have been facilitated by technical improvements of catheterisation devices1819. There are many potential explanations for the reduction in PCI radiation dose exposure during the last decade. First, technical improvements of catheterisation laboratories may have contributed to more efficient imaging and the reduction of radiation dose exposure20. Among the technical advantages are radiation tubes that replace conventional helical coils with flat emitters that allow shorter pulse width and better filtration resulting in a more efficient photon spectrum. Furthermore, detectors with higher dynamic range improve image detail accuracy and contrast. Furthermore, implementation of dose-saving techniques potentially contributed to the observed reduction of radiation dose exposure. The recommended strategies for dose reduction in PCI include careful preparation of the procedure and limitation of the fluoroscopy time, frame rate reduction1321, utilisation of low-dose fluoroscopy instead of high-dose cinefluorangiography, imaging in less angulated projections22, application of real-time dose monitoring14, and implementation of advanced image processing algorithms such as noise reduction technology1123.
Besides the overall reduction of radiation dose in PCI, the results of this study also demonstrate a significant 5.3-fold variability of the median DAP between catheterisation laboratories in the 2017/2018 dataset (p<0.001). A similarly high variability of the median DAP was observed in low-volume as well as in high-volume catheterisation laboratories. This illustrates the wide range of radiation dose exposures in routine clinical PCI and demonstrates the need for further dose reduction. In accordance with the findings of our study, a significant variability regarding the exposure of extremely high radiation doses during PCI procedures has been observed between catheterisation laboratories in a recent study24.The results from this study should be noted as an opportunity for implementing radiation safety quality improvement practices across institutions. Interventional cardiologists should critically review the radiation safety performance of their catheterisation laboratory radiographic systems and consider modernisations and modifications to minimise radiation dose exposure. Furthermore, interventional cardiologists should continuously monitor the radiation exposure of their own PCI procedures, and consequently implement the above-mentioned dose-saving strategies in order to improve safety during the procedure for patients and staff.
Additionally, we strongly recommend the participation of institutions in radiation dose surveys allowing benchmarking with other physicians and institutions. The participation in such programmes might improve “best practice” performance. Furthermore, the certification of catheterisation laboratories which adhere to “best practice” recommendations will help patients and doctors to select centres with low radiation exposure for cardiac catheterisation. Interestingly, the volume of PCI procedures performed by an institution was not associated with lower radiation doses in this analysis. This demonstrates that the number of PCIs performed per se does not support best practice regarding radiation safety.
Another important finding of this study is the identification of clinically relevant and independent predictors for radiation dose exposure in PCI. In our analysis, we set the level for a clinically significant change in radiation exposure to an estimated ED ≥1 mSv, because predictors with even smaller changes became statistically significant in this analysis due to the very large sample size. Using a multivariate model, we identified patient-related (male gender, history of CABG and heart failure) and procedure-related (coronary occlusion PCI, ostial lesion PCI, left main PCI and multivessel PCI) predictors that were associated with increased radiation dose exposure (all p<0.001). We recommend that, in the presence of these dose risk factors, interventional cardiologists should pay specific attention to radiation reduction and should keep the radiation dose exposure as low as reasonably achievable. In particular, the implementation of dose-saving techniques should be critically reviewed in any of the above-mentioned risk-related PCI scenarios, before starting with the procedure.
Limitations
A number of limitations have to be considered when interpreting the findings. The PROTECTION VIII study is limited by its observational retrospective design. In this study, no direct radiation dose measurements were taken. Some catheterisation laboratories might have used systems that actually measure DAP, while other systems only calculate radiation dose parameters. Additional patient characteristics (access site, body mass index), lesion characteristics (separation into acute or chronic coronary occlusion), technical parameters (specifications of the catheterisation laboratories, different manufacturers, acquisition protocols) and details of the operator (e.g., operator volumes within sites) with potential impact on radiation dose were not available in this quality assurance registry and could not be analysed; however, the approach allowed a nationwide representative analysis of radiation exposure in clinical practice. Advanced procedural details were not specified between 2008 and 2016; nevertheless, the subanalysis of PCI procedures in 2017 and 2018 was still constituted by over 0.5 million patients and reflects most recent PCI practice. Finally, the results from PROTECTION VIII were obtained in Germany only and transfer of the results to other countries might be limited.
Conclusions
In conclusion, the results from this large radiation dose survey demonstrate that radiation exposure in PCI practice has been considerably reduced over the last decade. Importantly, a large variability in median radiation dose was observed between catheterisation laboratories, which suggests the need for further site-specific training and education as well as the standardised implementation of advanced technology and low-dose procedural protocols. In particular, cardiologists should critically revise and utilise all available radiation dose reduction techniques in high radiation risk scenarios including PCI of coronary occlusion, ostial lesions, the left main artery, and multiple vessels.
Impact on daily practice
PCI is frequently performed in Western societies and has emerged as an indispensable tool in cardiology. Besides its impact on morbidity and mortality, potential deleterious effects of procedural radiation exposure are of significant healthcare concern for both the examined patient and the investigating invasive cardiologist. The PROTECTION VIII study demonstrates considerable reduction of radiation dose exposure in PCI, implicating improved procedural safety for patients and invasive cardiologists. The observed large intersite variability in PCI-associated radiation dose in current clinical practice requires particular attention. Hospitals and healthcare providers are requested to improve site-specific equipment and radiation dose education further. Clinicians should use low-dose acquisition protocols by default in order to keep radiation dose as low as reasonably achievable.
Funding
The study was supported by the German Heart Foundation/German Foundation of Heart Research (grant number F/39/20 to TJS).
Conflict of interest statement
J. Hausleiter has received speaker honoraria and research support from and serves as consultant for Abbott Vascular and Edwards Lifesciences. H. Möllmann has received speaker/proctor honoraria from Abbott Vascular, Boston Scientific, Edwards Lifesciences, Siemens Healthcare and SMT. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.