Abstract
Aims: The radiation exposure resulting from cardiovascular procedures may increase the risk of cancer, and/or cause skin injury. Whether the novel cardiovascular automated radiation reduction X-ray system (CARS) can help reduce the patient radiation dose in daily clinical practice remains unknown. The aim of this study was to evaluate the reduction in patient radiation dose with the use of CARS in the cardiac catheterisation laboratory (CCL).
Methods and results: This study retrospectively analysed 1,403 consecutives patients who underwent a cardiac catheterisation with coronary angiography (CA) and/or a percutaneous coronary intervention (PCI) in the Brest University Hospital over the course of one year. Patient radiation doses (dose area product and air kerma) were collected and compared between the CCL with (new CCL) and without (control CCL) CARS. Additionally, the patient radiation doses according to femoral versus radial access, procedural complexity and body mass index were compared. The radiation lesion position on the skin was assessed by automatically optimising the X-ray source to image distance (SID) and subsequently generating a radiation Dose-Map for those procedures exceeding 3 Gray of exposure. Overall, 447 patients underwent procedures in the control CCL and 956 in the new CCL. Baseline patient and procedural characteristics were similar between the two groups, with the exception of male gender and primary PCI, which were more prevalent in the new CCL group. Compared to the control CCL, the utilisation of the CARS in the new CCL resulted in a reduction of dose area product by 46% for CA, 56% for PCI alone and 54% for CA and PCI during the same procedure. Of note, radial access generated a higher radiation dose than femoral access (p<0.001). In this study, seven patients had an air kerma exceeding 3 Gray; however, only one patient had a skin dose greater than 3 Gray.
Conclusions: The utilisation of the CARS resulted in a significant reduction in patient radiation doses compared to the control equipment. A real-time Dose-Map may help the operator change the projection during complex procedures to reduce the patient skin dose.
Abbreviations
CARS: cardiovascular automated radiation reduction X-ray system
CCL: cardiac catheterisation laboratory
DAP: dose area product
Gy: Gray
SID: source-to-image distance
Introduction
The radiation received from medical radiographic imaging procedures and diagnostic tests has become the greatest source of exposure to ionising radiation in the general population1. Coronary angiography (CA) and percutaneous coronary intervention (PCI) are among the most common cardiovascular procedures and provide the largest contribution to the annual cumulative patient radiation doses2. This exposure is known to have deleterious health effects, both stochastic and deterministic, such as increasing the risk of long-term malignancy3-5, and increasing the risk of acute skin injury, particularly in procedures of a relatively long duration6. It is therefore essential to keep the radiation dose “as low as reasonably achievable” (ALARA) and to consider the appropriateness of each procedure. According to the European Commission Council Directive3, the International Commission on Radiological Protection4,7 and additional international guidelines8,9, both the evaluation of the exposure of patients undergoing medical procedures involving ionising radiation and the comparison to reference values are highly recommended. Since the introduction of the first flat panel X-ray system, numerous technological improvements in medical radiographic equipment have been made in order to aid reducing the radiation exposure both for patients and for operating staff10. The first of these involved improvements in the efficiency of the image chain (X-ray tube, flat panel detector and image processing) so that more clinical information could be captured while decreasing the amount of radiation used in any given procedure. The second improvement was the development of several dose reduction features, such as the automatic optimisation of distance between the flat panel and the patient to reduce the amount of radiation absorbed by the patient. Finally, the third improvement was the development of new dose awareness tools, such as the Dose-Map™ (Ashland Inc., Ashland, KY, USA), which displays in real time the estimated skin dose during treatment and also enables monitoring and minimising of peak skin radiation during PCI procedures. These three technological advances will be referred to as the cardiovascular automated radiation reduction X-ray system (CARS) in this manuscript. The CARS portends an automated radiation dose reduction for the patient, without any manual intervention by the physician or staff.
The hypothesis for this study was that the use of the CARS technology installed in the new CCL will significantly reduce patient radiation exposure during CA and/or PCI procedures, compared to the previous-generation laboratories. Additional objectives included the identification of the main factors which contribute to patient radiation and whether the new features, such as the awareness tools, may possibly enable operators to adapt their clinical practice to reduce patient radiation exposure further.
Methods
STUDY DESIGN
This is a retrospective observational, single-centre comparison on the radiation doses between patients undergoing CA and PCI either in the new CCL (with CARS) or in the control CCL (with standard X-ray equipment), from January 2013 to December 2013, at the Brest University Hospital Centre, Brest, France. Of note, the radiation dose parameters were predefined before the study; however, the patient and procedural characteristics were collected retrospectively. Patients who received transcatheter aortic valve implantation (TAVI), right heart catheterisation, or cine angiography of aortic or mitral mechanical valves were excluded. The Centre’s cardiac catheterisation volume includes around 1,300 CA and 800 PCI procedures per year. Four experienced operators carry out diagnostic and therapeutic cardiac catheterisations in new and control CCL. Of note, all of these operators switched from a primary femoral to radial routine approach in 2011.
X-RAY EQUIPMENT
The novel radiolographic equipment (X-ray imaging system) used in this CCL was the Innova IGS 520 (GE Healthcare, Little Chalfont, United Kingdom) with the CARS technology, installed in December 2012. The equipment was initially set at a speed of 7.5 frames per second for fluoroscopy (with the ability to modify to 15 frames per second) and 15 frames per second for cine angiography. On the other hand, the control equipment was the Innova 2000 (GE Healthcare) installed in 2004. The frame speed was defined at 15 frames per second for both fluoroscopy and cine angiography. The main difference in radiation reduction strategies between the two groups of CCL was the CARS, which included the efficiency of the image chain (X-ray tube, flat panel detector and image processing), dose reduction features (automatic optimisation of distance between the flat panel and the patient) and the new dose awareness tools (Dose-Map).
PROCEDURE DETAILS
To characterise the population, the following data were collected: clinical and demographic parameters including sex, age and body mass index (BMI), procedural details including access site, indication for the procedure, and the type of procedure, i.e., CA alone, PCI alone or CA and PCI during the same procedure (CA+PCI). Two parameters were used to define the complexity of PCI. The first was procedure duration from arterial puncture to arterial closure. The second parameter was the number of devices used, which included intracoronary wires, balloons, stents, rotational atherectomy devices, intravascular ultrasound (IVUS), optical coherence tomography (OCT), or fractional flow reserve (FFR), but excluding guiding catheters. Thus, a complex procedure was defined as having a duration ≥54 min (corresponding to the 4th quartile) and the use of more than five devices (4th quartile). Simple procedures were characterised by a procedure duration ≤27 min (1st quartile) and fewer than two devices used (1st quartile).
PATIENT RADIATION DOSE ASSESSMENT
The patient radiation dose measured with the use of various radiation parameters was automatically captured by both systems. The air kerma (Ka,r), dose area product (DAP), dose rate, fluoroscopy and cine angiography (time and DAP for each) were collected. Ka,r corresponds to the cumulative dose at the patient entrance reference point located 15 cm back from the isocentre towards the focal spot; it has been used as a predictor of the risk of tissue effects5,8,9. The DAP, also called kerma area product, is the integral of air kerma and reflects the total energy delivered to the patient; it is thus a reasonable indicator of the risk of stochastic effects. The dose rate is the dose delivered per minute by the system.
Additional information was collected from the new CCL: source to image distance (SID), and the main camera projection angles during the PCI procedures that contribute to the overall patient dose. After the conclusion of each procedure, for each patient who received a dose exceeding 3 Gray in air kerma, the estimated peak skin dose relative to the estimated true absorbed dose that the skin received during the procedure was calculated, and a map of the estimated skin dose distribution (Dose-Map) was generated.
STUDY ENDPOINTS
The primary endpoint was patient radiation dose measured by the DAP and the total air kerma during each procedure for the new CCL vs. the control CCL study groups. The secondary endpoints included a detailed analysis of the impact of vascular access, BMI, procedure type, and lesion location on the patient radiation dose. An additional evaluation included creating a Dose-Map for each patient who achieved the cumulative threshold of 3 Gray patient radiation doses during the same procedure.
STATISTICAL ANALYSIS
All statistical analyses were performed with the SPSS, Version 20.0 (IBM Corp., Armonk, NY, USA). Continuous variables were summarised by mean±standard deviation or by median and the 25th to 75th interquartile range. Categorical variables were presented as percentages. Differences in categorical variables were tested by either the chi-square or the Fisher’s exact test. Continuous data were tested by parametric or non-parametric tests (Mann-Whitney U or Student’s t-test), as deemed appropriate. In addition, a multivariable linear regression model adjusted for significant differences between the new CCL group and the control CCL group including age, gender, primary PCI, lesion location and contrast average was performed to assess the DAP and total air kerma reduction with CARS. A p-value <0.05 was considered an indicator of statistical significance.
Results
During 2013, a total of 1,403 procedures were carried out in both types of CCL. Of these, 956 were procedures performed in the new CCL incorporating the novel CARS, which included 598 CA studies and 358 PCI procedures. In the control CCL group without the CARS, 447 procedures were performed, which included 290 CA and 157 PCI procedures.
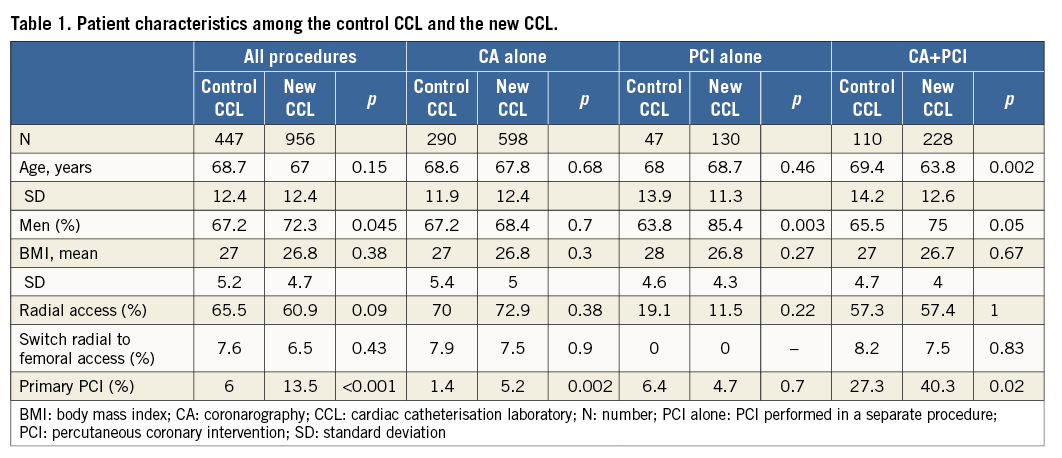
PATIENT AND PROCEDURAL CHARACTERISTICS
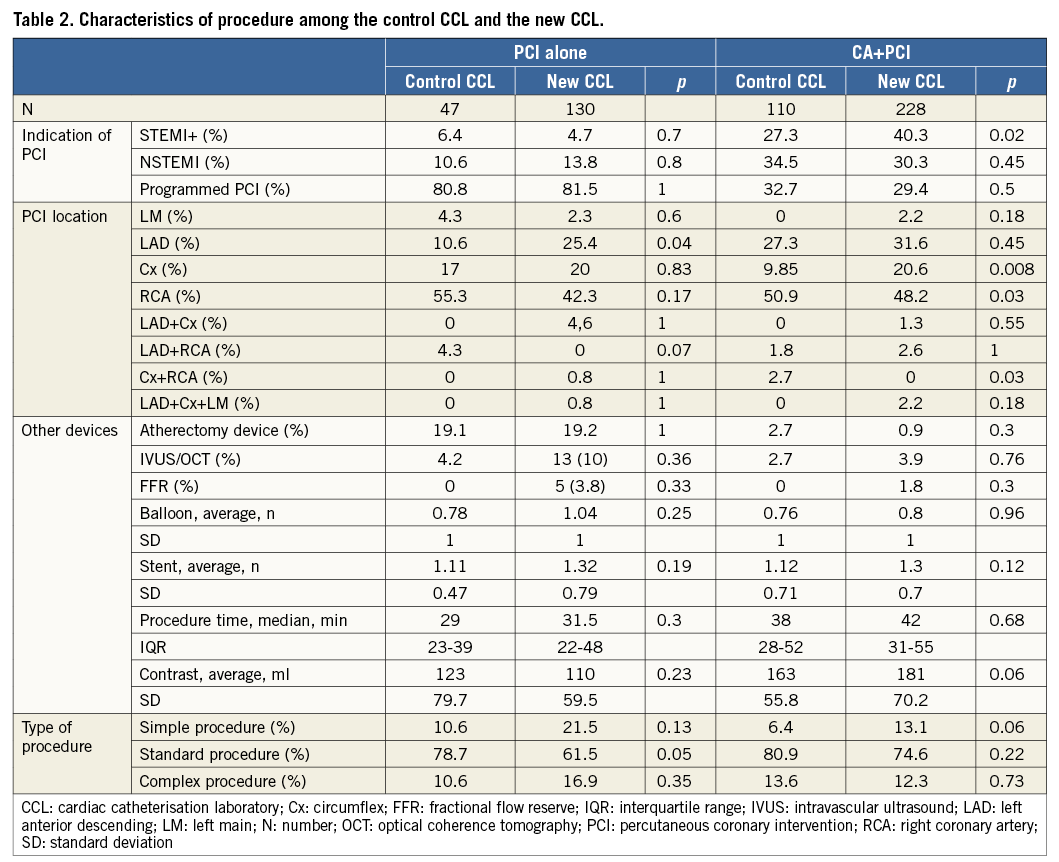
Baseline characteristics according to the type of procedure completed and further subcategorised according to the use of the new CCL vs. the control CCL are presented in Table 1. The baseline characteristics demonstrate similar age and BMI for the overall population, while the prevalence of male gender and primary PCI was higher in the new CCL group. The default access approach was the radial artery for CA and for CA+PCI. Of note, left radial access was most frequently used (84.4%) compared to the right radial access. As illustrated in Table 2, the distribution of procedural complexity was equal between the new and control CCL groups. However, regarding the index PCI artery, the incidence of left anterior descending coronary artery PCIs was more common in the new CCL vs. the control CCL for PCI alone, while in the CA+PCI procedure the incidence of circumflex coronary artery PCIs was significantly higher in the new CCL.
PATIENT RADIATION DOSE PARAMETERS
As depicted in Table 3 and Figure 1A, total patient radiation doses assessed either by the DAP or by total air kerma were significantly lower in the new-generation CCL compared with the control CCL. Overall, the magnitude of the respective patient radiation reduction in the new CCL compared to the control CCL, as assessed by DAP, included: 46% (5,505 vs. 2,708 cGy.cm²; p<0.001) for CA alone, 56% (6,056 vs. 2,656 cGy.cm²; p<0.001) for PCI alone, and 54% (9,721 vs. 4,497 cGy.cm²; p<0.001) for CA+PCI. Similarly, the total air kerma was also significantly reduced, favouring the new CCL compared to the control CCL for CA (336 vs. 713 mGy; p<0.001), for PCI alone (400 vs. 913 mGy; p<0.001) and for CA+PCI (672 vs. 1,510 mGy; p<0.001). After adjustment for significant differences in patient characteristics between the new and control CCL including age, gender, primary PCI, lesion location and contrast average, the radiation reduction remained significant for each class of procedure, with a 39% reduction in DAP for CA, 43.5% for PCI and 24% for CA+PCI (p<0.001 for all comparisons) (Figure 1A).
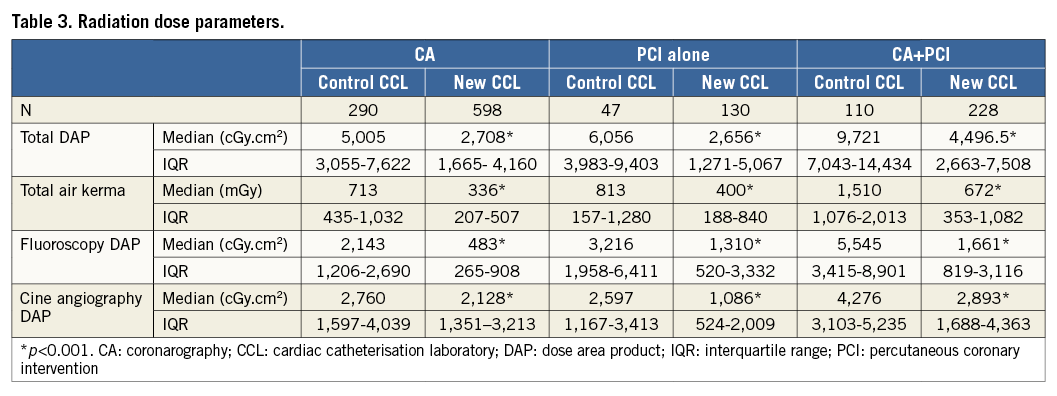
Although the fluoroscopy time was longer than the cine time for all types of procedure, cine time conferred a higher contribution to DAP in the new CCL group (Figure 1A, Figure 1B).
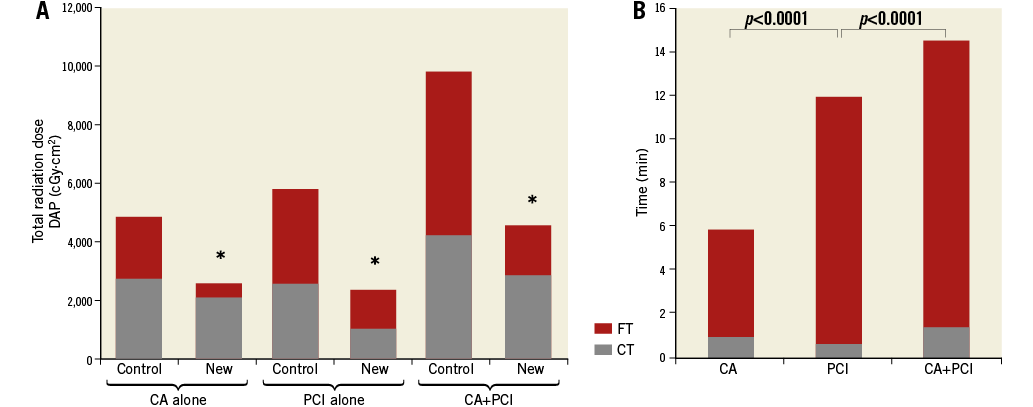
Figure 1. Radiation dose parameters. A) Comparison of total radiation dose in DAP between new CCL and control CCL according to fluoroscopy and cine angiography for each type of procedure. After adjustment: β for CA=0.390, p<0.001; β for PCI=0.435, p<0.001; β for CA+PCI=0.242, p<0.001. * p<0.001. B) X-ray time with the new CCL. CA: coronarography; CCL: cardiac catheterisation laboratory; CT: cine angiography time; DAP: dose area product; FT: fluoroscopy time; PCI: percutaneous coronary intervention.
IMPACT OF BMI AND VASCULAR ACCESS ON PATIENT RADIATION DOSE
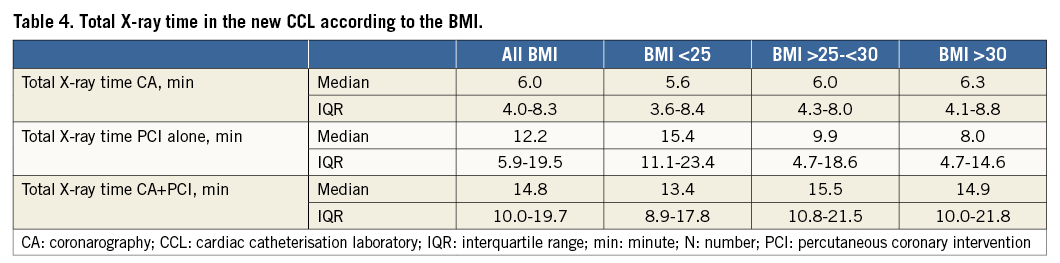
Among patients who underwent procedures in the new CCL, patient radiation dose was significantly influenced by BMI and vascular access route. Notably, even with modern X-ray equipment BMI had a strong influence on DAP rates for both fluoroscopy and cine times (Figure 2). However, the SID automatic optimisation feature in the new CCL allowed the SID to be maintained at around 1.05 m for each tertile of BMI, resulting in an insignificant augmentation of SID for patients with BMI >30 kg/m2 (Figure 3). This feature, in turn, enabled the operator to limit the radiation dose for patients. Of note, X-ray time was not higher among patients with BMI >30 kg/m2 (Table 4).
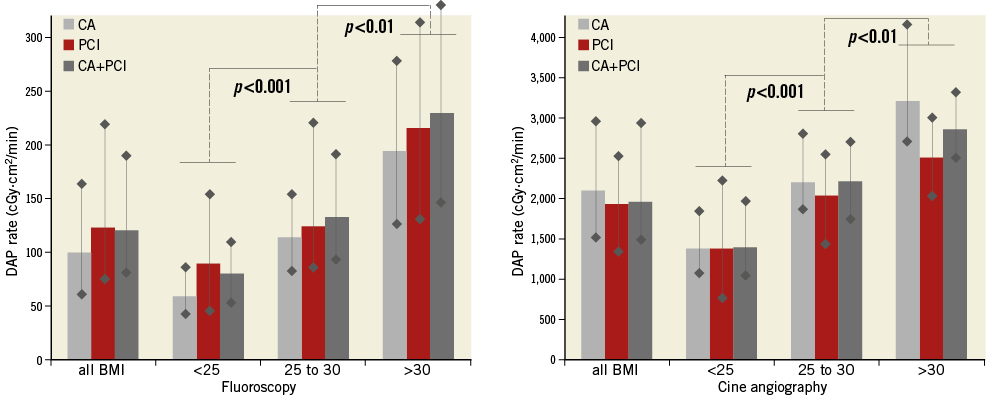
Figure 2. Median and interquartile range of DAP rate in fluoroscopy and in cine angiography according to the BMI in the new CCL group. BMI: body mass index; CA: coronarography; CCL: cardiac catheterisation laboratory; DAP: dose area product; PCI: percutaneous coronary intervention
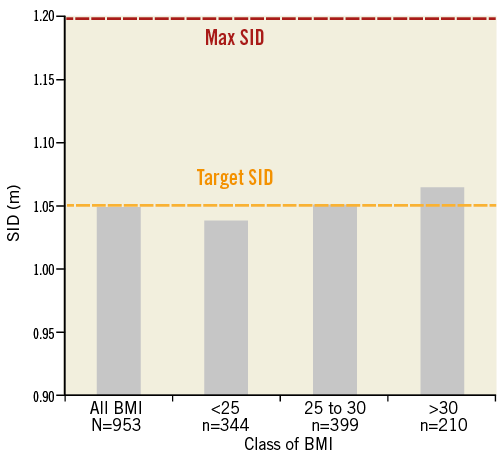
Figure 3. Automatic optimisation of SID: variation of the SID in all procedures of the new CCL group (N=953) according to the different classes of BMI. BMI: body mass index; CCL: cardiac catheterisation laboratory; N: number of procedures; SID: source to image distance
Overall, the radial approach was associated with higher radiation exposure assessed by DAP than the femoral access for both CA (28.2 vs. 23.3 Gy.cm²; p<0.0001) and CA+PCI (61.8 vs. 36.2 Gy.cm2; p<0.0002), as demonstrated in Figure 4. Potential contributors to the higher radiation doses among patients undergoing radial access were longer average total X-ray time (+1.7 min, p<0.0001) and fluoroscopic time (+2.9 min, p=0.0003) when compared to the femoral access.
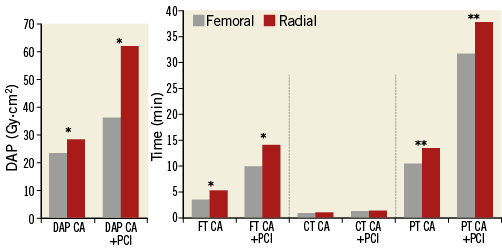
Figure 4. Comparison between femoral and radial access for CA, and CA+PCI in terms of dose area product, fluoroscopy time, cine angiography time and procedure time in the new CCL group. *p<0.0002. **p<0.02. BMI: body mass index; CA: coronarography; CCL: cardiac catheterisation laboratory; CT: cine angiography time; DAP: dose area product; FT: fluoroscopy time; PCI: percutaneous coronary intervention; PT: procedure time
IMPACT OF LESION POSITION AND PRIMARY PCI PROCEDURES ON PATIENT RADIATION DOSE
The details of lesion locations in patients treated in the new CCL are shown in Table 2. For each of the 358 PCIs in this group, the first projection that contributed to the exam-cumulative dose (i.e., projection producing the majority of the dose received by the patient) is shown in Figure 5. The estimated patient thickness as seen by the X-ray system in this first projection, which was independent of the BMI, was 2 centimetres greater for circumflex artery lesions than for the right coronary or left anterior descending lesions. This additional thickness for circumflex lesion location led to a significant augmentation of the dose rate compared to right coronary or left anterior descending artery lesions under fluoroscopy (39 vs. 21 and 27 mGy/min; p<0.0001, for the circumflex vs. right coronary and left anterior descending, respectively) and under cine angiography (442 vs. 278 and 337 mGy/min; p<0.0001, for the circumflex vs. right coronary and left anterior descending, respectively). In addition, albeit to a lesser extent, the dose rate for the left coronary system lesions was greater than that for the right coronary system lesions (p=0.04). Furthermore, the median patient radiation dose among patients who underwent primary PCI was higher compared to the other procedures (4,878 vs. 3,890 cGy.cm2; p=0.005, respectively).
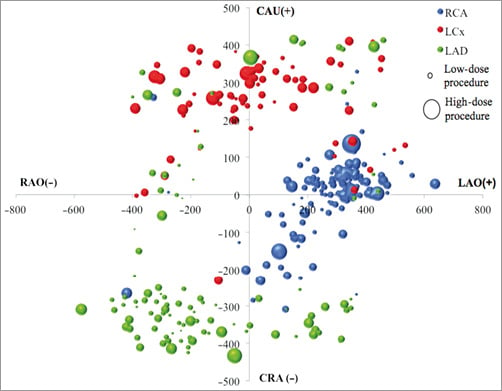
Figure 5. Spatial repartition and dose for each PCI (N=358) for the first angulation contributing to cumulated dose in the new CCL group. CAU: caudal; CCL: cardiac catheterisation laboratory; CRA: cranial; LAO: left anterior oblique; RAO: right anterior oblique
PATIENT RADIATION DOSE-MAP
Only seven patients (0.7%) had a cumulative dose higher than the threshold of 3 Gy in the new CCL, as opposed to 14 patients (3.9%) in the control group (p=0.001). The latter included three patients with a cumulative dose >5 Gy. No significant skin lesions were found at one-year follow-up evaluation in these 21 patients. The estimated peak skin radiation dose and the Dose-Map were retrospectively generated for the seven high-dose patients who underwent procedures in the new CCL. According to this map, only one patient received a skin radiation dose that exceeded 3 Gy (Figure 6), with all procedures in this group of patients being categorised as complex, as per the study protocol definition.
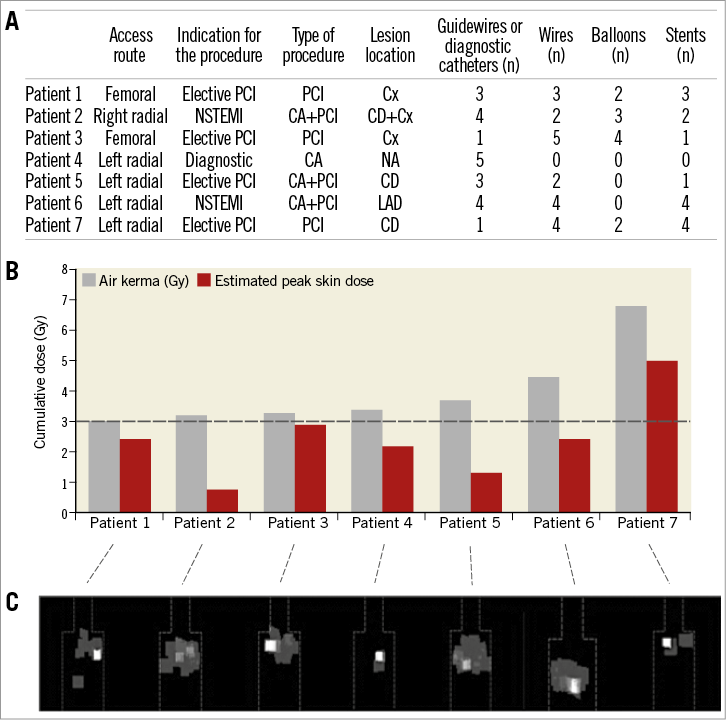
Figure 6. High-dose patients from the new CCL: procedure characteristics, cumulative doses, and Dose-Maps. A) Procedure characteristics. B) Air kerma and estimated peak skin dose. C) Dose-Map. ---- Limit of 3 Gy. CA: coronarography; CCL: cardiac catheterisation laboratory; Cx: circumflex coronary artery; LAD: left anterior descending coronary artery; n: number; NSTEMI: non-ST-segment elevation myocardial infarction; PCI: percutaneous coronary intervention; RCA: right coronary artery
Discussion
This study demonstrates the significant beneficial impact of CARS (including the improvement of the X-ray tube, the flat panel, the addition of dose reduction features and additional tools that are able to tailor the patient dose) on patient radiation dose reduction. There were several notable findings including the following. 1) There was a significant reduction in the DAP and total air kerma for both CA and PCI procedures with the new X-ray equipment using CARS. 2) Although there was a steady increase in patient radiation dose directly related to an increasing BMI, new features such as the automated optimisation SID were able to maintain the target SID (≈1.05 m) and potentially contribute to automatic reduction of the patient dose. 3) Radial access, circumflex lesion location and emergency procedure were significantly associated with higher patient radiation. 4) A patient radiation Dose-Map may be useful to monitor patients for the assessment of potential skin complications after long procedures.
Currently, medical radiographic diagnostic and interventional examination and procedures are considered to be the major source of radiation exposure for the general population. This radiation exposure represents a significant risk for both staff and the patient2,3. Ionising radiation has been associated with several types of cancer3-5 and acute skin injuries6 due to either deterministic or stochastic effects. The deterministic effects are directly related to the absorbed radiation dose, and the severity of the effect increases as the dose increases. Thus, our findings of patient radiation dose reduction by about 50% after the re-engineering of our CCL compared to our control CCL of the previous generation may potentially reduce the risk of both types of injury. Moreover, the radiation dose from our new CCL was consistently lower than that of the average overall historical control from the French11 and United States12 registry data for patients undergoing PCI alone (2,656 vs. 4,780 vs. 11,700 cGy.cm2, respectively) or CA+PCI (4,496 vs. 5,800 vs. 11,900 cGy.cm2, respectively).
In recent years, there has been an increase in the awareness of radiation risks among the cardiac and vascular societies, which have therefore recommended routine adoption of control measures, such as applying collimation, fluoroscopy at 7.5 frames/sec, and reduced time of cine, to reduce radiation doses further. Although efficient in reducing the radiation exposure, these measures may have been offset by the increase in cardiovascular procedural complexity in both coronary (e.g., chronic total occlusions) and extra-coronary (e.g., transcatheter heart valves) domains where, at times, the radiation time is the only limitation for procedural completion. Therefore, novel ways to prevent and monitor excessive patient radiation doses represent an unmet clinical need in the further reduction of the radiation risk for our patients.
The gradual improvements in radiographic systems technology along with the implementation of new-generation X-ray systems, such as the automatic optimisation of the SID, can add supplementary tools that decrease patient radiation exposure. In our study, although the total patient radiation directly correlated with BMI as has been described in other studies13, the new optimisation could potentially reduce the total radiation absorbed by the patient across all BMI groups (including BMI >30 kg/m2) while maintaining the image quality during the procedure and without the need for physician adjustment or increasing the total X-ray time (Table 4). This study suggests that this dose reduction feature should be widely activated for all CCL which have this function pre-installed or, if this automated system is not available, the physician should diligently monitor and verify the SID manually after each projection.
In our cohort, radial access resulted in a higher radiation dose than femoral access in both CA and PCI procedures. Our data are in line with previously published studies14, which demonstrated that radial access results in additional radiation exposure compared to femoral access. The increased dose associated with radial access was possibly mainly due to the additional fluoroscopy required to control and image the advancement of the guidewire and catheter from radial puncture to the aorta. Furthermore, this could also be attributed, at least in part, to the use of the left radial in our cohort, which might require the alignment of the radiation source with the left arm for the advancement of the guidewire, and thus may increase the radiation level due to the superposition of the abdomen and the radius and ulnar bones. However, from our study it is reasonable to speculate that, by switching to a low radiation dose setting (3.75 frames per second), while following the guidewire from the radial puncture to the aorta, where the temporal resolution is not necessary, this could be one way to offset the higher radiation levels caused by the radial access.
This study confirms that PCI of lesions located in the circumflex artery involves unavoidable excess irradiation of the patient in comparison to lesions in other arteries15. The tools available in the new system provide real-time data, such as the Dose-Map, which can help the interventional cardiologist to reduce the patient skin radiation dose during the procedure. This would result not only in correcting relatively trivial problems, such as the interposition of the patient’s arm in the radiation field, but also in implementing modifications such as minor changes in the projection angle during the procedure, thereby altering the distribution of the skin radiation dose without affecting the quality of the image obtained. Furthermore, displaying the Dose-Map in real time, on the screen with a cursor between 0 Gy and 2 Gy during the procedure will help the operator to assess the ongoing radiation absorption status of the patient. This may be a simple but worthwhile tool to help the operator be mindful of and continually follow the radiation dose, and constitutes an easily implemented measure in guiding the operator to tailor his or her own procedural routine in an attempt to minimise the patient radiation. This tool could also encourage the physician to revise the projection during the procedure in order to distribute the dose to the skin and to reduce the risk of potential skin injuries. The construction of a Dose-Map after long procedures helps to identify patients who have experienced a high peak skin dose, which in turn can prompt the physician to assess the patient for potential complications involving the skin at follow-up. In addition, the general practitioner can also utilise the Dose-Map to guide their examination of the skin during a follow-up physical examination.
Limitations
Although this study was performed in a single centre with the same operators and similar procedural complexity characteristics between the new CCL and the previous-generation CCL, we cannot exclude the possibility of residual bias. In addition, the estimation of the real patient dose by the DAP and the air kerma captured by the equipment also constitutes a limitation. Moreover, the extraction of the mean SID for each procedure was only available in the new CCL, making the comparison with the control group unfeasible. The retrospective creation of the Dose-Map and the skin follow-up were only completed for the patients with a high dose of air kerma. This could also be considered a limitation.
Conclusion
The use of the CARS results in a reduction in patient radiation dose compared to the earlier systems. This reduction permits achievement of a radiation dose level substantially lower than national and international reference values. Additionally, the new tools facilitate real-time monitoring of the distribution of estimated patient skin dose (Dose-Map) during PCI and have demonstrated the benefit of changing the projection of the X-ray beam during complex and long procedures.
| Impact on daily practice The use of the cardiovascular automated radiation reduction X-ray system available in the new cardiac catheterisation laboratories allows reduction of patient radiation dose in coronary angiography and percutaneous coronary intervention without the need for manual adjustment by the operator. The new tools help to monitor and evaluate patient radiation during and after the procedure. |
Conflict of interest statement
The authors have no conflicts of interest to declare.