“Seeing is believing” is an idiom that means only physical or concrete evidence is convincing. Thomas, one of the twelve apostles, claimed this before Jesus Christ, who responded that there were those who had not seen but nevertheless believed. It leads to a sophistry that “seen evidence” can be interpreted easily and correctly, even when, in fact, interpretation may be difficult. When we work in the catheterisation laboratory our main aim is to obtain high-quality images from the patient’s heart to allow the proper treatment. This is done using ionising radiation that cannot be captured by our senses. It is not seen, smelled or heard.
Increased radiation may have long-term hazardous effects on the patient and on the operator. Although in recent years there has been an increase in the awareness of radiation risks, the focus of the operator is mainly on the treatment and less on ways to reduce radiation1-3. In general, and especially during complex and emergency cases, the typical operator does not always follow basic safety measures to avoid excess radiation, to both patient and himself/herself, does not use all shielding available, and cares less about how to prevent orthopaedic damage and injuries to himself/herself.
Novel ways to prevent and monitor excessive patient radiation dose are an unmet clinical need to reduce radiation risk to the patient and to the operator further. Most of the radiation to the operator comes from scatter radiation from the patient. Humans understand better and more easily when they see something different from the norm. One example is the expiry notification in the BVS package - which appears in a different colour. Thus, the staff understand very clearly that the device has expired, unlike other stents or medications that simply have a regular label that indicates when they reach expiry date. Most X-ray vendors simply provide a five-minute notification of fluoroscopy time, aimed at reminding the operator of the radiation, but that is all. With the new X-ray models there are many improvements, including an option for medical staff to monitor their personal X-ray dose exposure in real time. The information is presented in a clear way with the cumulative dose of the case on a screen in front of the operator. This may help reduce unnecessary radiation. All major vendors have made efforts to decrease radiation whether in hardware, image processing or software. Two papers on this important topic appear in this issue of EuroIntervention.
Wilson et al4 evaluated whether a real-time colour pictorial radiation dose-monitoring system reduces patient skin and total dose during coronary angiography and intervention. The operator can see, adjacent to the fluoroscopy image, a real-time pictorial display of the dose-tracking system. The display provides a colour-coded representation of the cumulative skin dose distribution on a patient graphic as well as real-time peak skin dose and cumulative skin dose values at the current beam projection. The colour pictorial changes to yellow when peak skin dose reaches 2,000 mGy and then red when greater than 3,000 mGy (Figure 1). The present analysis, which was not randomised but included more than 1,000 patients, showed that the use of the skin dose recording system resulted in a 22% reduction in peak skin dose. Not surprisingly, radiation dose reduction was most pronounced in those having interventions (40% reduction) but was also seen over a range of subgroups including those with prior coronary artery bypass surgery, high BMI, and with radial arterial access.
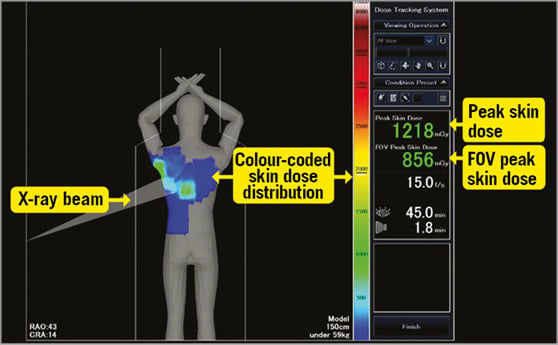
Figure 1. Operating screen of the dose tracking system. Illustration of the colour-coded skin dose distribution display area and the dose information display area which includes numerical peak skin dose and field of view peak skin dose estimates. FOV: field of view
Christopoulos et al reported a reduced radiation total dose when an audible tracking system was used5. In our catheterisation laboratory we also used similar methods to measure radiation. When the radiation meter starts to beep, for example during prolonged attempts to cannulate the RCA, the operator instinctively and immediately stops stepping on the fluoroscopy pedal. The increased frequency of beeps during periods of higher radiation dose may be distracting to the operator, worrying to the patient, and may ultimately be a limitation for wide adoption of such a technology.
Didier et al6 report in this issue a retrospective analysis of 1,403 patients undergoing angiography with a new X-ray imaging system and compare these data to their own historical radiation data collected with an older X-ray machine. The new model was equipped with the Cardiovascular Automated Radiation Reduction X-ray System (CARS). It includes an automated radiation dose reduction for the patient, without any manual intervention of the physician or staff. CARS includes a more efficient image chain (X-ray tube, flat panel detector and image processing), improved dose reduction features (automatic optimisation of distance between the flat panel and the patient) and dose map (a new dose colour awareness tool). The new functions resulted in a reduction of dose area product (DAP) of 46% for angiography and more than 50% for interventions. The authors note that radial access, circumflex lesion location and emergency procedure were significantly associated with higher patient radiation and that the real-time dose map may change their practice during complex procedures.
In both studies published in this issue, there was a significant reduction in the DAP and total air kerma for both diagnostic and interventional procedures with the new X-ray equipment. Of note, the radiation dose was evaluated by various radiation parameters captured automatically from the equipment. No actual measurements were performed and all were based on device/machine automatic reporting output. This output is based on multiple calculations and assumption and may all be a result of the vendor algorithm change. In the era of self-reporting results by well-respected companies such as Volkswagen and Mitsubishi, we should keep in the back of our minds that the values presented are the result of complex calculations and are presented by the vendor. Few studies have compared different vendors7, and it is almost impossible to learn and compare between vendors regarding these values and other radiation aspects.
However, at this time in radioprotection, the DAP is the best we have. It is available and used in all catheterisation laboratories for the control and evaluation of patient radiation. It is easy to record for each patient and should be used in order to assess the patient radiation dose. Moreover, the correlation between the DAP and the effective doses accessed by patient dosimetery on phantom studies appears good.
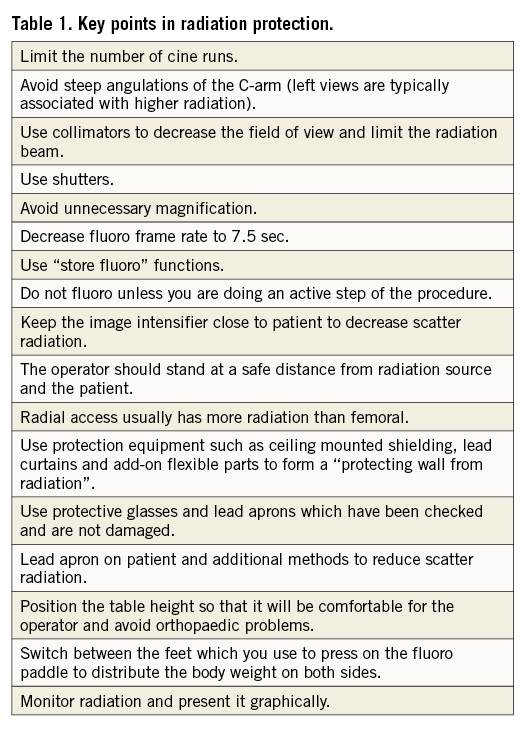
In recent years there has been an increase in the awareness of radiation risks among the cardiac and vascular societies, which have therefore recommended routine adoption of control measures (Table 1). It has previously been demonstrated that education on radiation protection techniques results in reduced radiation dosing. Yet, over time, without regular and continued feedback, the knowledge and work habits may not be maintained8. There is a continued struggle to remind the operator about radiation hazards and ways to reduce them.
During coronary angiography there is currently no audiovisual signal notifying the operator of the radiation dose. We work in a blind (and deaf) fashion. In the past, miners would bring canaries into the coal mine. As long as the canary kept singing, the air was safe. When it stopped, it served as an early warning that it was time to leave the mine. Software to reduce radiation and systems to provide real-time graphic feedback are designed to prompt alterations in operator behaviour and reduce dose. Awareness of the peak skin dose prompts operators to work in a different view and avoid an overlapping field of view. When the new position involves less detector angulation, there is likely to be less output from the tube, thus reducing DAP and air kerma. The automatic CARS package and similar improvements by all vendors allow greater attention to well recognised, but often neglected, techniques of reducing radiation.
Seeing radiation is believing, causing our work habits to change. These new solutions are our modern canaries because they provide an early warning of unnecessary radiation which cannot be detected by human senses. These newer functions may alter physician behaviour and improve patient outcome by making it possible for dose reduction changes to occur during the procedure. Consideration should be given to widespread adoption of these technologies. They do not need to be an additional, expensive and fancy function. We should demand that all vendors include all radiation safety measures as their basic standard of care. This will serve as a paradigm shift in radiation monitoring and reduction in dose and hazards.
Conflict of interest statement
The author has no conflicts of interest to declare.