Introduction
During the past 30 years, interventional cardiology has advanced dramatically resulting in outstanding increases in occupational radiation exposure of interventional cardiologists. Despite the remarkable changes in fluoroscopic procedures, radiation protection technology is not much different from how it was decades ago. Moreover, new evidence on occupational radiation suggests that low doses of ionising radiation exposure may be associated with the development of cancer in interventional cardiologists and radiologists1-6. The brain is of particular interest, because it is one of the least protected organs during interventional procedures2. The trunk and the thyroid are protected with lead aprons, and the eyes are protected by lead glasses; however the head is completely exposed. The annual head dose sustained by a cardiologist generally ranges between 20 and 30 mSv, and in some cases may reach up to 60 mSv per year7. This indicates a dose 10 times higher than whole body exposure8.
Ceiling-suspended lead shields reduce radiation doses to the brain but they are designed to protect the face and head from primary scatter radiation from the patient. Therefore, a significant amount of secondary radiation scattered from the laboratory walls may reach the operator’s head, despite the presence of a ceiling-mounted glass shield. Until now, operators have not used protective garments to protect their head from radiation.
We have investigated the efficacy of the lead cap in radiation protection of the head and have compared it with that of a ceiling-mounted lead glass screen in a real-life setting.
Description
The lead cap weighs approximately 1,140 grams and is closed under the chin, thereby also providing protection of oral mucosa and parotids. The cap provides 0.5 lead equivalent protection and can be worn with protective eyewear and a thyroid shield (Figure 1).

Figure 1. Lead cap, glasses, collar and apron. A dosimeter was attached outside the lead cap on the left side of the head, a second one was placed inside the lead cap at the level of the other dosimeter outside the lead cap, and a third was placed outside the apron at the level of the lower trunk on the left side.
Indications for use
The lead cap is used for radiation protection of the head in the catheterisation laboratory. It also provides protection for oral mucosa and parotids.
History
Lead caps have been suggested as a method for reducing occupational radiation to the brain, but these were considered to be uncomfortable and did not find common acceptance among interventionalists. The scarce amount of data regarding the effectiveness of lead caps in radiation protection of the head is based on laboratory measurements rather than real-life experiences of operators9. Although subjective, data regarding the comfort of these caps are also lacking.
Clinical experience
Occupational radiation data were obtained from three personal dosimeters attached to a single interventional cardiologist employed in a university clinic. One of the dosimeters was attached outside the apron at the level of the lower trunk on the left side, the second one was worn outside the lead cap on the left side of the head, and the third one was placed inside the lead cap at the level of the other dosimeter outside the lead cap (Figure 1). The dosimeter worn outside the lead cap gave an estimate of the dose to the unprotected head, and the dosimeter located under the cap provided an estimate of the dose received by the head shielded with the cap. Dosimeters were processed by the National Atomic Energy Authority. A detailed analysis of personal dosimeter records is conducted every three months.
A ceiling-suspended articulated glass shield (40-50 cm; MAVIG, Munich, Germany) which is lengthened by an attached lead flap (35-50 cm), a longitudinal table-mounted lead shield (60-75 cm), and a lead cap (Burkhart Roentgen International, St Petersburg, FL, USA) all with 0.5 mm lead equivalent were used to provide radiation protection in the study.
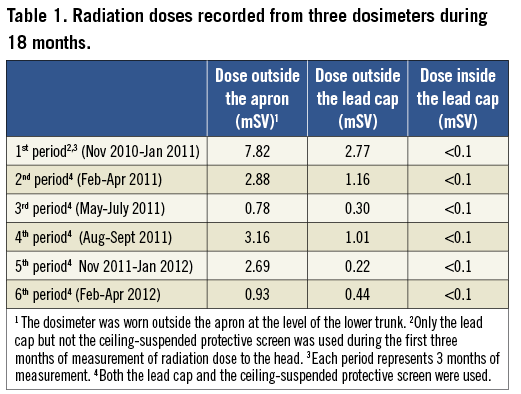
The data were recorded from three dosimeters for a total of 18 months between November 2010 and April 2012. The operator performed 1,282 procedures during the study period. These procedures included 1,073 diagnostic coronary procedures, 158 coronary interventions and 51 cardiac device implantations. The lead cap was worn by the operator in every procedure on a regular basis during the entire study period. Only the lead cap but not the ceiling-suspended protective glass screen was used during the first three months of measurement of radiation dose to the head. Later, both protection devices (the lead cap and the ceiling screen) were used by the operator for the remaining 15 months of radiation measurement. Under these real-life conditions, the efficacy of the lead cap was compared with the ceiling-mounted lead glass screen. The effectiveness of the concomitant use of both protection devices was also analysed.
The radiation dose to the head recorded by the dosimeters outside the lead cap was highest during the first period. The doses were 2.4 to 12.5 times higher in comparison to the measurements that were recorded when the ceiling-suspended screen was used.
The use of a ceiling-mounted screen has significantly reduced the radiation dose to the head recorded by the dosimeter outside the lead cap, but the dose measured by the dosimeters inside the lead cap was <0.1 mSv during the whole study period, regardless of the use of a ceiling-mounted screen (Table 1). The reading of the dosimeter outside the apron located at the level of the lower trunk was also reduced with the use of a ceiling-suspended shield (Table 1).
Although being a subjective conclusion, the operator regularly wearing the lead cap reported that the lead cap was reasonably comfortable and offered an acceptable level of comfort when used in daily practice.
Discussion
Interventional cardiologists are exposed to the highest doses of ionising radiation among medical staff using x-rays8. This long-term occupational exposure to ionising radiation lasting for decades could pose a health hazard and has been suggested to be associated with an increased incidence of malignancies including brain tumours1-5,10-12. Roguin et al reported a total of 18 head and neck tumours in interventional cardiologists and radiologists working with ionising radiation3. During interventional procedures, the left side of the head is known to be more exposed to radiation than the right side. The side of the brain involved is known in 10 of the malignant brain tumours reported by Roguin et al. Among these patients, the tumour was located on the left side of the brain in 92% of cases, which cannot be explained by coincidence. These observations reverberated strongly in the cardiac world, and some authorities proposed the development of protection devices, such as special helmets or specially designed panels13.
Our study revealed that the use of a ceiling-mounted screen reduced radiation to the head to some degree, yet a remarkable dose of radiation was received by the operator’s head despite the use of this shield. Our study has been performed in a single operator and this can be considered as a limitation. However, we clearly documented that a lead cap is extremely effective, and much more effective than a ceiling-suspended screen, in reducing head radiation exposure. There is a common prejudice against these caps which are thought to be potentially uncomfortable, which add yet more weight to the load already being worn and which may therefore lead to degenerative cervical disease and neck pain. However, the operator in our study who has eight years of experience without a cap commented that the lead cap has a reasonable level of comfort and can be worn on a regular basis.
Long-term follow-up studies investigating the risk of brain cancer associated with chronic radiation exposure in interventional cardiologists are necessary. Until we have sufficient data to make definite conclusions, we believe it is better to be on the safe side and take the necessary precautions to limit radiation exposure to our heads. We hope the high effectiveness and comfort of the lead caps, as evidenced in this study, may encourage interventionists to consider using caps in their own catheterisation laboratories.
Conflict of interest statement
The authors have no conflicts of interest to declare.