Introduction
From the previous survey performed by the European Association of Percutaneous Cardiovascular Interventions Women Committee1, it appears that both women and men consider that the overall risk linked to radiation exposure hampers women from a career in interventional cardiology. Interventional cardiologists (IC) are exposed at the highest levels of radiation registered amongst medical staff using X-rays2.
Despite a specific definition of the safe dose limit and protective strategies for the foetus3,4,5,6, the “risk of pregnancy” is often evoked as a reason for not pursuing an interventional career, or to justify not choosing young women for a position. However, little is known about the current radiation-reducing strategies in European cath labs7.
Accordingly, the first aim of the “EAPCI Women’s Radiation Exposure and Regularities in European Catheterisation Laboratories Survey” was to assess current practices on radiation protection; the second was to examine the sex ratio and practices during pregnancy.
Methods
A web-based survey was developed by the EAPCI Women Committee (Supplementary Appendix 1, Supplementary Appendix 2).
Results
The survey was emailed to 1,065 cath lab directors in March 2016 (Supplementary Appendix 1).
Finally, 18 countries participated in the survey (Supplementary Table 1).
Baseline characteristics are shown in Supplementary Table 2. Ninety-seven centres had at least one item of radiological equipment older than 10 years, with a higher proportion (42.8%) in centres with more than three angiographic suites (p=0.006).
Figure 1 shows the number and type of personal dosimeters and available radioprotective shielding. Active personal dosimeters (see definition in Supplementary Appendix 3) were available in 48% of centres, with a higher proportion in high-volume PCI centres (difference 35.5%, p<0.01). Concerning radioprotective measures, cath labs were well equipped with appropriate protective tools.
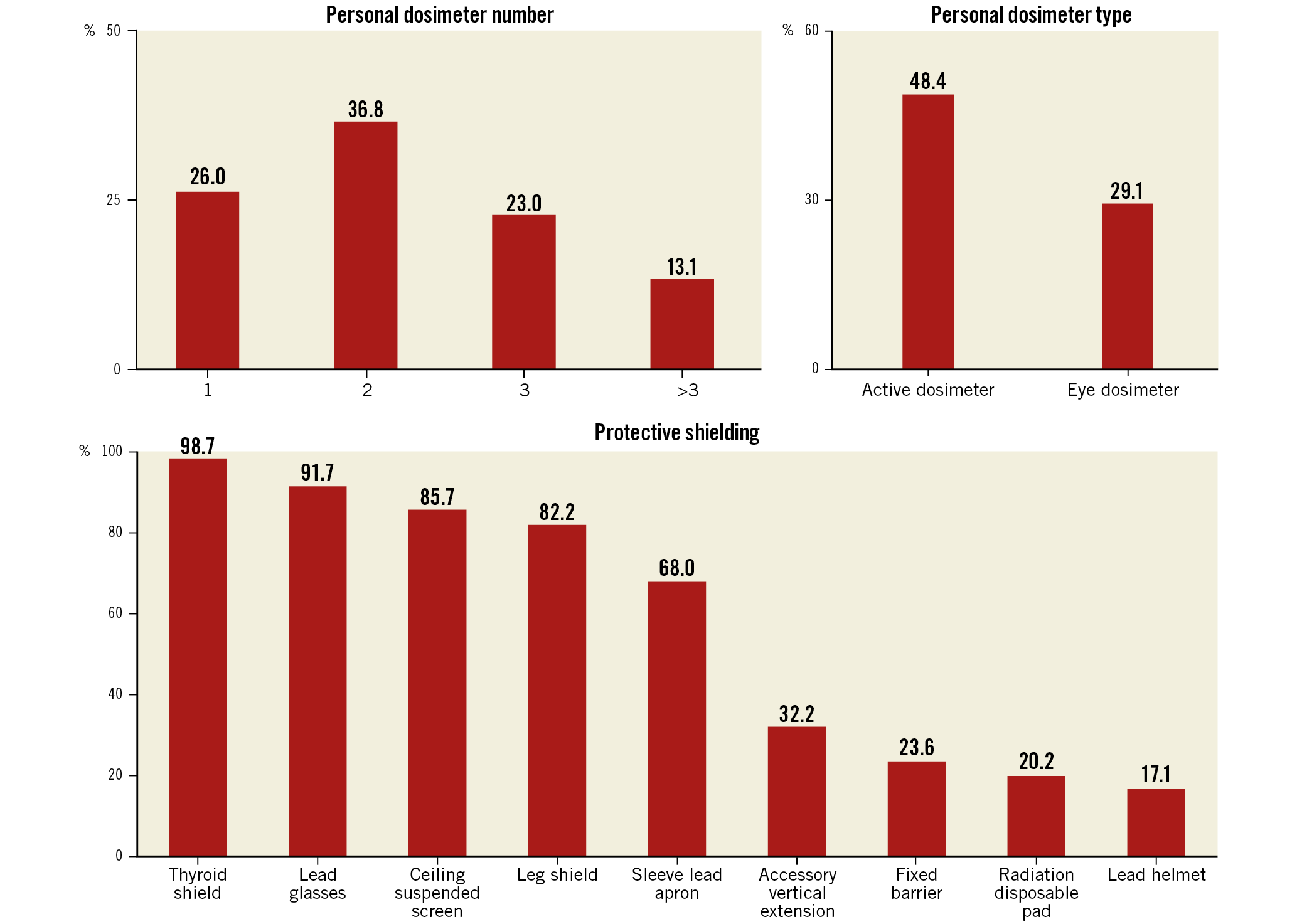
Figure 1. Number and type of personal dosimeters and available radioprotective shielding.
The reporting frequency of radiation exposure was monthly in 39% of cases (Supplementary Figure 1). A medical follow-up was scheduled in 80% of the centres, with one (29%) or two (36.5%) control visits per year with blood count (78.5%), thyroid function evaluation (61%) and eye examination (54%). Only a small percentage could state their cumulative and eye radiation dose for the past year (8% and 5%, respectively); 5% had never attended any educational programme on radiation protection.
In more than one third of all catheterisation laboratories, none of the IC were women. Female operators accounted for 18% (n=353) of 1,952 IC, with a similar proportion whatever the type of institution: tertiary centre, public or private, or high- or low-volume centre. Cath lab director roles were held by females in 25 centres. Female fellows accounted for 24.5% (n=147) of the total 599 fellows (p<0.01). Supplementary Figure 2 shows the distribution of physicians according to their age and sex.
For 8% of directors, the “risk of pregnancy” constituted a hindrance for a fellowship or permanent position. Nevertheless, work was allowed during pregnancy with radiation limits and adapted radiation protection equipment for 64 female physicians in 51 centres: for 14/53 in France, 2/147 in Italy, 9/11 UK and 3/4 in Denmark. Knowledge of the foetus dose limit was insufficient.
Discussion
The main findings of the survey are as follows:
1) 29.7% of the radiological equipment is older than 10 years;
2) 2/3 of the physicians wear at least two dosimeters. The minimal radiation protection equipment is present;
3) Interventional cardiology is still predominantly a male sub-speciality;
4) Local policies concerning work during pregnancy are very heterogeneous, even within each country.
The European Directive3 has updated basic safety standards: the dose limit for eye lens has been lowered from 150 to 20 mSv/year, and the recommended number of dosimeters is at least two.
It has been suggested that no more than 10% of radiological equipment should be older than 10 years8. Compared to the WIN survey7, we observed a larger reported use of lead glasses and table-suspended lead screens.
Current data do not suggest increased risks to the foetus5, with a dose limit for the foetus of 1 mSv3, and monthly monitoring of foetus dose4,5,6. Reproductive concerns have also been raised for interventional male physicians9. Nearly 60% of medical students worldwide are women, but women in cardiology still account for less than 20%10,11, with interventional cardiology remaining the lowest proportion. It has been shown that companies make more profit when workers and boards consist of both sexes12. Cath labs could benefit similarly from this.
Limitations
The survey was completed in 326 centres (30.6%).
Conclusions
Interventional cardiologists are the most exposed to ionising radiation. Newer strategies are available to reduce the radiation dose; improvement in awareness and follow-up are crucial.
|
Impact on daily practice The survey showed the availability and use of minimal radiation protection tools; however, less than 30% use a lens dosimeter and less than 10% know their level of radiation exposure. Sex disparity is still high. Evolution of the regulations upon pregnancy in the working environment seems possible. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.