Abstract
Aims: Interventional cardiologists who work in cardiac catheterisation laboratories are exposed to low doses of ionising radiation that could pose a health hazard. DNA damage is considered to be the main initiating event by which radiation damage to cells results in development of cancer.
Methods and results: We report on four interventional cardiologists, all with brain malignancies in the left hemisphere. In a literature search, we found five additional cases and thus present data on six interventional cardiologist and three interventional radiologists who were diagnosed with brain tumours. All worked for prolonged periods with exposure to ionising radiation in the catheterisation laboratory.
Conclusions: In interventional cardiologists and radiologists, the left side of the head is known to be more exposed to radiation than the right. A connection to occupational radiation exposure is biologically plausible, but risk assessment is difficult due to the small population of interventional cardiologists and the low incidence of these tumours. This may be a chance occurrence, but the cause may also be radiation exposure. Scientific study further delineating occupational risks is essential. Since interventional cardiologists have the highest radiation exposure among health professionals, major awareness of radiation safety and training in radiological protection are essential and imperative, and should be used in every procedure.
Introduction
Glioma is the most common primary malignant brain tumour in adults and has a poor prognosis. The age specific incidence of this tumour is increasing in many developed countries, and this increase appears to be only partly explained by improved diagnostic techniques1.
Although, several epidemiological studies have investigated the role of potential risk factors for glioma, its aetiology remains poorly understood, and there appears to be no association between glioma and the various dietary and lifestyle factors commonly associated with cancer at other body sites2. The higher incidence of glioma in males has long suggested an occupational cause, and possible risk factors include ionising and non-ionising radiation. Several previous studies have examined the possibility that occupational exposure to radiation increases the risk of brain tumour but their results have been largely inconsistent3-5.
There are several occupational hazards of interventional cardiology, one of the unspoken secrets of this field. Interventional cardiologists, either treating the coronaries or doing electrophysiology procedures, are likely to receive high radiation exposure in spite of adequate protection. This protection has its price. The operator works standing and wearing lead. This is done repeatedly over many years. As a result, especially those over the age of 35 years old will frequently develop orthopaedic problems, such as aches and pains in the neck, back, hips, knees and ankles that range in severity6. Fortunately, the orthopaedic problems usually can be relieved by rest and other conservative methods.
The more potentially serious danger in interventional cardiology is radiation. Yet, what are the hazards of radiation? Recently, Ciraj-Bjelac7 reported on the risk of radiation-induced cataracts for staff in interventional cardiology. The authors examined eyes of interventional cardiologists, nurses and age- and sex-matched unexposed controls, and found a dose-dependent increased risk of posterior lens opacities for interventional cardiologists and nurses. The relative risk of lens opacity was 5.7 (95% CI: 1.5-22) for interventional cardiologists and 5.0 (95% CI: 1.2-21) for nurses. Astrong dose-response relationship was found between occupational exposure and the prevalence of radiation-associated posterior lens changes.
While the trunk and the thyroid are protected with lead, and special glasses can protect the eyes, the head is completely exposed! Is there a real risk for head tumours in this growing field of medicine? The operators are doing more procedures than ever, which usually last longer, with the overall result being more exposure to radiation than in the past. This paper presents some of the known cases of brain tumours among interventional cardiologists and presents data on four new cases and to summarise what is known from the literature today.
Methods
An extensive literature search was performed. The search looked for malignancies, brain neoplasms, dose-response relationships, occupational exposure, radiography, risk assessment hazards, coronary angiography (adverse effects), ionising radiation, neoplasms (radiation-induced), radiation hazards. The authors of the manuscripts were contacted for any additional information. We also contacted several heads of neurosurgery departments as to whether they have additional physicians as patients.
The new cases data was obtained from the medical records and interviews with family members and/or colleagues.
Results
We were able to collect data on nine cases all working in catheterisation laboratories (Table 1). There were five cases previously reported. The first paper published in 1997, was entitled “Is brain cancer an occupational disease of cardiologists?”. This paper discussed the cases of two interventional cardiologists from Toronto, Canada, who were diagnosed with brain tumours (glioblastomas)8. Both worked at the University of Toronto and both had exceptional records of quality of patient care, education and research9. One was in his early 60’s and had worked as an interventional cardiologist for many years at the Toronto General Hospital; the other was younger, in his early 50’s, and worked not only in the catheterisation laboratory, but also as a nuclear cardiologist for 20 years. The time from diagnosis to death was several months.
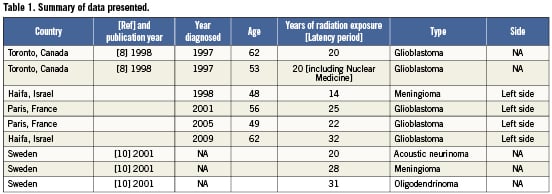
Another paper from Sweden in 2001, described three physicians working with fluoroscopy10. The latency periods were 20, 28 and 31years, although all three worked for only part of this period with x-ray exposure. They were diagnosed with acoustic neurinoma, meningioma and oligodendrinoma, respectively. The authors calculated an increased risk for brain tumours in the work of a physician as OR 6.00, 95% CI 0.62-57.7.
We were unable to obtain additional information concerning whether the five malignancies reported above were on the right or left side of the brain. The four new cases that we will now report on in this paper all concerned left side involvement.
In Haifa, Israel in 1998, a 48-year-old interventional cardiologist was found to have left side meningioma with trigeminal neuralgia, ptosis and diplopia as his presenting symptoms. He had worked with old cine-film equipment and had been exposed to x-ray radiation on a daily basis for 14 years.
In Paris, France, two cardiologists were diagnosed with brain tumours. Both were very experienced interventional cardiologists who had performed a high volume of procedures, working for many years with old cine-film equipment in the catheterisation laboratory.
The first was diagnosed in 2001 at the age of 56, with left temporal grade III oligoastrocytoma. He died in 2005, at the age of 59. The second was diagnosed in 2005, at the age of 49, with left temporo-occipital grade IV oligoastrocytoma; he died in 2006, at the age of 50.
In 2009, in Haifa, Israel, a 62-year-old male interventional cardiologist was diagnosed with a left frontal gliobalstoma multiforme (Grade IV) after a seizure as his presenting symptom. He had performed thousands of procedures over the past several years and had been exposed to x-ray radiation on an almost daily basis for approximately 32 years. He underwentradical surgery followed by radiotherapy and chemotherapy. He died several months after diagnosis, at the age of 63. Interestingly, his father died at the age of 87, several weeks after being diagnosed with a glioma.
Discussion
We present information on three radiologists with brain tumours, as well as six interventional cardiologists all with several years of exposure to ionising radiation. Five of the cardiologists developed brain glioma and died a few months after diagnosis. Interventional cardiologists who work in cardiac catheterisation laboratories are exposed to low doses of ionising radiation that could pose a health hazard.
As we noted above, we were not able to determine the side of the malignancy in the previously published papers8-10. It is of interest that in the four new cases which we describe all concerned the left side of the head (Table 1). This is consistent with the dose distribution of the radiation exposure pattern for the interventional cardiologist/radiologist. The annual head exposure to these specialists head area is in the range of 20 to 30 mSv per year11, about 10 times higher than the whole body exposure, and it is the left side of the head which is exposed two times more than the right side12.
DNA damage is considered to be the main initiating event by which radiation damage to cells results in development of cancer and hereditary disease. In fact, chromosomal aberrations in peripheral blood lymphocytes have been used for many years to monitor human populations exposed to potential carcinogens. Results from prospective cohort studies have shown a significant increase for all cancers in subjects with a high frequency of chromosomal aberrations, as acute myeloid leukaemia10,13.
Chromosomal abnormalities can reliably be assessed by evaluating the frequency of occurrence of micronuclei (MN) in dividing cells, inasmuch as MN mainly originate from chromosome breaks or whole chromosomes that fail to engage with the mitotic spindle when the cell divides1. Indeed, the MN assay has recently been endorsed by the International Atomic Energy Agency as one of the main cytogenetic methods for assessing chromosome damage after radiation accidents and as a biological dosimeter of radiation exposure5.
Andreassi et al13 assessed the effects of chronic low-dose x-ray radiation exposure on somatic DNA damage of interventional cardiologists working in high-volume cardiac catheterisation laboratories. They used peripheral lymphocytes and the assay for MNs, which is considered to be a reliable biological dosimeter for radiation exposure. They compared 31 interventional cardiologists to 31 age- and sex-matched clinical cardiologists and found that interventional cardiologists showed higher MN values (20.5±1.6 vs. 12.8±1.3, p=0.001), although some overlap was apparent in the individual subject analysis. A correlation between the years of professional activity and MN frequency value was detectable for interventional cardiologists (r=0.428, p=0.02), but not for clinical cardiologists (r=0.253, p=0.17). The results indicated that, overall, interventional cardiologists working in a high-volume catheterisation laboratories have higher levels of somatic DNA damage when compared with clinical cardiologists working outside the catheterisation laboratory. In summary, they say that the amount of this damage varies and is only weakly related to the duration of professional exposure, which suggests that a dominant modulation of the underlying genetic substrate by environmental factors has a role in determining the harm in individual physicians.
Similar findings were reported by Zakeri et al14 who compared 37 interventional cardiologists and 37 clinical physicians as the control group with similar age, sex and duration of employment, without any work-related exposure to ionising radiation. The frequencies of chromosomal aberrations were significantly higher in the group of interventional cardiologists as compared to that of the clinical physicians. The frequencies of aberrant cells, chromosome breaks and dicentrics plus centric rings were significantly higher in the exposed group as compared to the control group, without positive correlation between the frequency of dicentric and centric ring aberrations and the cumulative doses on the interventional cardiologists. Immune responses seem to be more resistant to the effects of such a low-dose ionising radiation exposure, although some cellular responses are stimulated and some cytokine productions are modulated. The authors concluded that while cytogenetic results show higher chromosomal damage, some immune responses are stimulated or modulated immunologically in interventional cardiologists.
Several previous studies indicated that chronic low doses of ionising radiation can lead to significant somatic DNA damage in professionally exposed physicians. Hospital workers exposed to low doses of ionising radiation had a higher frequency of MN than did controls15,16. Maffei et al also found increased MN values in exposed hospital workers who smoked17. A significant increase in the occurrence of chromosomal aberrations was also observed in hospital workers chronically exposed to ionising radiation16-20. In addition, Bozkurt et al found a 50% increase in cells with sister chromatid exchange in 16 nuclear physicians when compared with 16 non-exposed physicians21. Similar findings were obtained when the alkaline Comet assay was used to evaluate medical personnel exposed to x-rays15.
As these malignancies are rare, the question whether exposure to ionising radiation indeed increases the risk is not easy to answer.
Most of the calculations are based on atomic bomb calculations, and there is a great debate if this can be applied to cancer probability. Risk estimates such as these at the population level can be highly inaccurate at the individual level. Most analyses trying to determine risk have methodological weaknesses and are based on hypotheses and assumptions that are not solidly based22,23. Calculations and analysis performed by several groups, such as Jacob et al22, does not confirm that the cancer risk per dose for low-dose-rate and moderate-dose (LDRMD) exposures is lower than that for atomic bomb survivors. This result challenges validity of the cancer risk values currently considered for occupational exposures.
However, several papers which measured occupational doses from fluoroscopy-guided interventional procedures, such as the recently published report by Venneri et al24, calculated that there was an increased cancer risk caused by professional radiation exposure in modern invasive cardiology practice.
The chromosomal DNA damage after cardiac catheterisation procedures has been assessed in children with congenital heart disease who were exposed to a significant cumulative radiation dose25. MN, as a biomarker of DNA damage and long-term risk predictor of cancer values, increased significantly after these procedures in comparison with baseline. This indirect cancer risk estimation and direct DNA data both emphasise the need for strict radiation dose optimisation, especially in children.
We know that interventional cardiologists work in the catheterisation laboratory for many hours, some on a daily basis, usually for many years. Several reports found that the dosage of ionising radiation in interventional cardiology were the highest ones registered among medical staff using x-rays12,24. Thus, there is no doubt that there is a significant exposure to an ionising radiation environment5. We also know that DNA is especially prone to mutations, and in recent years we have learned about the cellular changes occurring in brain tumours1.
Solid “evidence-based medicine” in this field is lacking. Malignant brain tumours account for about 2% of cancers, and 24,000 cases of brain or spinal cancer are diagnosed each year in the USA alone. Radiation is a known risk factor for brain tumours. The cases reported in this paper could all be a simple matter of chance without any relationship to occupational exposure. Still, it is reasonable to assume that ionising radiation does not improve health!
Epidemiologic evidence for radiation-induced brain cancer in fluoroscopists is suggestive, but by no means conclusive. One study26 found that the death rate from brain cancer in radiologists was almost three times that of other medical specialists who did not use radiation. A case-control study10 of 233 patients with brain tumours reported that work as a physician with the use of fluoroscopy increased the risk of developing a brain tumour, with an odds ratio of 6.0 (95% CI, 0.62-57.7), although there were only three such individuals among the 233 cases. Another case-control study27 of 476 individuals diagnosed with glioma, also observed an increased risk in physicians and surgeons (odds ratio, 3.5; 95% CI, 0.7-17.6). However, such studies cannot exclude other biological agents or chemicals which are unrelated to radiation as causative, and other case-control studies28,29 failed to identify a significant risk of brain tumours as a result of exposure to medical ionising radiation.
The topic of occupational hazards, including cancers, to medical workers is an area of active study by the Multi-Specialty Occupational Health Group (MSOHG), a joint effort of several professional organisations29-32. Its purpose is to confirm that the interventional laboratory poses workplace hazards that must be acknowledged, better understood, and mitigated to the greatest extent possible.
There is an urgent need to expand the limited information on average annual, time-trend and organ doses from occupational radiation exposures as well as to assess lifetime cancer risks of these workers. Scientific studies further delineating occupational risks are essential. The MSOHG has initiated epidemiologic studies designed to help answer fundamental questions important to those working in fluoroscopic environments32.
For physicians and technologists performing interventional procedures, more information about occupational doses should be collected and long-term follow-up studies of cancer and other serious disease risks should be initiated. Such studies will help optimise standardised protocols for radiologic procedures, determine whether current radiation protection measures for medical radiation workers are adequate, provide guidance on cancer screening needs, and yield valuable insights on cancer risks associated with chronic radiation exposure.
To conclude, the available evidence suggests that chronic exposure to low-dose radiation has an adverse effect on somatic DNA of professionally exposed workers. This effect seems to be cumulative over time, although the majority of these studies failed to establish a dose-effect relationship for low doses11-20. Cumulative professional radiological exposure is associated with a non-negligible lifetime attributable potential risk of cancer, and this, above all, for the most exposed contemporary cardiac catheterisation laboratory staff12,24. Since interventional cardiologists have the highest radiation exposure among health professionals, major awareness of radiation safety and training in radiological protection are essential and imperative, and should be applied in every procedure.
The author invites physicians to report any information concerning the diagnosis of brain tumours in interventional cardiologists to the author or to the editors.
Conflict of interest statement
The authors have no conflict of interest to declare.

